Practice Parameter for Electrodiagnostic Studies in Ulnar Neuropathy at the Elbow
This guideline is greater than 5 years old. Every five years, an interim literature search is performed and the guidelines reviewed. While new studies have been published since this guideline was last reviewed, the Practice Issue Review Panel Committee of the AANEM has determined that these studies are not sufficient to mandate a revision of the guideline at the present time. The information contained in this guideline and the recommendations offered are still relevant to the current practice. Introduction
Literature Review
A Medline search was conducted for literature in English from 1983 through 1996 under the Medical Subject Headings (MeSH) (1) ulnar nerve, (2) electrodiagnosis, (3) nerve compression syndromes, (4) neural conduction, and (5) elbow. The initial search generated 282 article titles with abstracts. The abstracts were reviewed by two American Association of Electrodiagnostic Medicine (AAEM) Quality Assurance Committee members. Of the 282 articles, 56 articles referring to electrodiagnosis and other laboratory studies to evaluate UNE were found and reviewed. The bibliographies of these 56 articles were examined and additional articles identified and reviewed. In total, 398 titles, abstracts, and papers were evaluated for inclusion in the review. A total of 19 of the 398 articles and abstracts met five or six literature classification criteria; six of these articles were excluded from subsequent analysis for various reasons. For example, some investigators performed ulnar nerve conduction studies (NCSs) in the course of looking primarily at other phenomena, such as the effects of age on the conduction properties of multiple nerves, the correlation between clinical and electrodiagnostic findings, or the difference between proximal and distal nerve segments; the findings therefore have scant or no applicability to the evaluation of the clinical problem of UNE. Studies of normal control subjects met a maximum of five of five criteria; studies of patients with UNE met a maximum of six of six criteria. The remaining 13 articles formed the basis for the recommendations of this report. The findings of these and other additional studies are reviewed in a document developed by the AAEM.1 The conclusions and recommendations are based on a review of Class A evidence from 702 normal control elbows and 564 UNE elbows. The 13 articles reported sensitivities of electrodiagnostic studies ranging from 37% to 86% and specificities of 95% or greater.
Developed by the AAEM Quality Assurance Committee: William W. Campbell, MD, MSHA, Chair; Dorothy J. Carroll, MD; Michael K. Greenberg, MD; David A. Krendel, MD; Rhonda M. Pridgeon, MD; Kadambi P. Sitaram, MBBS; and Faren H. Williams, MD, in conjuction with the American Academy of Neurology and the American Academy of Phyical Medicine and Rehabilitation.
Authors had nothing to disclose.
*Medical College of Virginia, Richmond, VA; **University of Alberta, Edmonton, AB, Canada; ***Malcolm Grow USAF Medical Center, Andrews AFB, DC; ****Emory University, Atlanta, GA; *****The Rehabilitation Centre, Ottawa, ON, Canada; ******Virginia Mason Medical Center, Seattle, WA.
For review and critique of the manuscript, we would like to acknowledge the assistance of Michael T. Andary, MD, MS; Francis J. Bonner Jr., MD; Neil A. Busis, MD; Andrew A. Eisen, MD; Sudhansu Chokroverty, MD; Janice
L. Cockrell, MD; Les Dorfman, MD; Donna L. Frankel, MD; Earl R. Hackett, MD, Gerald J. Herbison, MD; M. David Jackson, MD; Kevin R. Nelson, MD; Mark Hallett, MD; Charles K. Jablecki, MD; James A. Leonard Jr., MD; Robert G. Miller, MD; Trilok N. Monga, MD; Richard K. Olney, MD; Gareth J. G. Parry, MBChB; Atul T. Patel, MD; Donald B. Sanders, MD; Yuen T. So, MD, PhD; J. Clarke Stevens, MD; John D. Stewart, MBBS, FRCP(C), MRCP; Robert L. Sufit, MD; Cheryl F. Weber, MD; Jacqueline J. Wertsch, MD; John R. Wilson, MD; Shirlyn A. Adkins, JD; Lori H. Hattenhauer, JD, MBA; and, especially, John C. Kincaid, MD. Literature Review approved by the Board of Directors: August 1996. Summary Statement approved by the Board of Directors: October 1997.
Literature Classification Criteria
1. Prospective study. 2. Diagnosis of UNE in the patient population based on clinical criteria independent of the electrodiagnostic procedure under evaluation. 3. Electrodiagnostic procedure described in sufficient detail, or reference provided to a published technique, to permit duplication of the procedure; the position of the elbow was stated and the same elbow position used throughout the study. 4. Limb temperature monitored and reported. 5. Reference values for the electrodiagnostic procedure obtained with either (a) concomitant studies of a reference population or (b) previous studies of a reference population in the same laboratory. 6. Criteria for abnormal findings clearly stated, and defined in statistical terms, e.g., range, mean + 2 standard deviations (SD), from data derived from the reference population. Definitions for Classification of Evidence
1. Class A evidence: studies that meet all six literature classification criteria, or five criteria in the case of studies only on normal control subjects. 2. Class B evidence: studies that meet four or five literature classification criteria, or less than five criteria in the case of studies only on normal control subjects. 3. Class C evidence: studies that meet three or fewer literature classification criteria. Definition of Practice Recommendation Strengths
The strength of a recommendation or conclusion is based on the quality and consistency of supporting evidence, as well as the magnitude of benefits, risks, and costs. The following rating system is used:
1. Practice standards: generally accepted principles for patient management which reflect a high degree of clinical certainty (Class A evidence). 2. Practice guidelines: recommendations for patient management which reflect moderate clinical certainty (Class B evidence). 3. Practice options/advisories: other strategies for patient management for which the clinical utility is uncertain (Class C evidence). Conclusions and Recommendations
The following conclusions and recommendations are made for the electrodiagnostic medicine evaluation of patients with suspected UNE. The recommendations are given in greater detail in the attached literature review. These recommendations are practice guidelines unless otherwise indicated.
General principles:
1. Ulnar sensory and motor NCSs should be performed with surface stimulation and recording. Limb temperatures should be monitored and maintained in a reference range and should be reported if outside a reference range. Corrections in conduction for temperature, if any, should be indicated in the report, although warming cool limbs and repeating the studies is preferable when possible. This recommendation is a practice standard. 2. If ulnar sensory or motor NCSs are abnormal, further NCSs should be carried out to exclude a diffuse process. This recommendation is a practice standard.
Elbow position:
3. Ulnar motor NCS reports should specify the elbow position used during the performance of the studies and the reference values employed. The technique used should be the same as that used to determine the reference values. The same elbow position should be employed during both stimulation and measurement. This recommendation is a practice standard. 4. The most logical elbow position for ulnar NCSs is moderate flexion; 70º to 90º from horizontal. Moderate flexion provides the greatest correlation between surface skin measurement and true nerve length. 5. Across-elbow distances used in evaluations performed with the elbow in moderate flexion have been in the range of 10 cm; this distance correlates best with published reference values. However, studies performed over this distance may mask a focal abnormality. Normal results over a 10-cm distance may occur despite a significant focal lesion. 6. Stimulation more than 3 cm distal to the medial epicondyle should be avoided as the nerve is usually deep within the flexor carpi ulnaris muscle by this point and there is substantial risk of submaximal stimulation.
Technique:
7. When using moderate-elbow flexion, a 10-cm across elbow distance, and surface stimulation and recording, the following suggest a focal lesion involving the ulnar nerve at the elbow: Multiple internally consistent abnormalities are more convincing than isolated abnormalities, which raise the possibility of artifact or technical mishap. (Note: The following are listed in order of strength of evidence):
a. Absolute motor nerve conduction velocity (NCV) from above elbow (AE) to below elbow (BE) of less than 50 m/s. b. An AE-to-BE segment greater than 10 m/s slower than the BE-to-wrist (W) segment. The literature is inadequate to make a recommendation regarding the percent of slowing. c. A decrease in compound muscle action potential (CMAP) negative peak amplitude from BE to AE greater than 20%; this suggests conduction block or temporal dispersion indicative of focal demyelination. This presumes that anomalies of innervation, i.e., Martin-Gruber anastomosis, are not present. d. A significant change in CMAP configuration at the AE site compared to the BE site. This presumes that anomalies of innervation, i.e., Martin-Gruber anastomosis, are not present. e. Nerve action potential (NAP) recording may aid in diagnosis, especially in patients with only sensory symptoms. However, NAP studies have significant pitfalls and limitations. Before relying on changes in NAP amplitude or conduction velocity (CV) as a diagnostic criterion for UNE, the examiner should be fully aware of the content and technical details of the applicable literature. Abnormalities of the distal sensory or mixed NAP, especially loss of amplitude, are nonspecific and nonlocalizing features of UNE. f. The literature is not adequate to make a recommendation regarding conduction through the AE-to-W or BE-to-W segments. 8. If ulnar motor conduction studies with stimulation at the wrist, above and below the elbow recording from the abductor digiti quinti are inconclusive, the following procedures may be of benefit:
a. NCSs recorded from the first dorsal interosseous (FDI) muscle. Because of differential fascicular involvement, fibers to the FDI may show abnormalities not evident when recording from the abductor digiti minimi. b. An inching study, exploring for changes in the CMAP amplitude, area or configuration, or for abnormal changes in latency over precisely measured 1- or 2-cm increments from AE to BE. The most convincing abnormality involves both a change in latency and a change in either amplitude, area, or configuration; however, latency changes in isolation may be significant. c. With severe UNE, distal wallerian degeneration may slow the BE-to-W segment secondarily and make localization difficult. Comparison of the AE to BE segment with the axilla-to-AE segment may be useful under such circumstances, but normative data is scant. This recommendation is a practice option. d. NCSs to forearm flexor muscles are not generally useful, but may be employed as a last resort with awareness of the technical limitations and the applicable literature. This recommendation is a practice option. e. Depending on the results of NCSs, needle electromyography (EMG) may be indicated. Needle examination should always include the FDI muscle, which is the most frequent muscle to demonstrate abnormalities in UNE, and ulnar innervated forearm flexor muscles. Neither changes limited to the FDI, nor sparing of the forearm muscles, exclude an elbow lesion. If ulnar innervated muscles are abnormal, the examination should be extended to include nonulnar C8/medial cord/lower trunk muscles, to exclude brachial plexopathy, and the cervical paraspinals, to exclude radiculopathy. Recommendations for Future Research
It is recommended that:
1. Future evaluations of electrodiagnostic studies in UNE patients be constructed to:
a. Meet all six literature classification criteria described in this report. b. Report the specific clinical criteria used for the diagnosis of UNE. c. Include calculation of the sensitivity and specificity of the test results. d. Include sufficient data to permit comparison to the results of previously published studies. 2. An outcome study be performed to assess the harm, benefit, and cost of performing NCSs and needle EMG in patients with symptoms suggestive of UNE. The value of electrodiagnostic studies in predicting treatment outcomes, including surgery, deserve future study. 3. The AAEM reviews this report every 5 years and updates the report as necessary. References
1. AAEM Quality Assurance Committee: Campbell WW, Chair; Carroll
DJ, Greenberg MK, Krendel DA, Pridgeon RM, Sitaram KP,
Williams FH. Literature review of the usefulness of nerve conduction studies and electromyography in the evaluation of patients with ulnar neuropathy at the elbow. Muscle Nerve 1999;22:S408-S411.
Approved by the Board of Directors: October 1997.
LITERATURE REVIEW OF THE USEFULNESS OF NERVE CONDUCTION STUDIES AND ELECTROMYOGRAPHY IN THE EVALUATION OF PATIENTS WITH ULNAR NEUROPATHY AT THE ELBOW
The sensitivity and specificity of nerve conduction studies and needle electromyography for the diagnosis of ulnar neuropathy at the elbow were evaluated by a critical review of the literature. With a search of the medical literature in English through January 1996, 101 articles were identified and reviewed on the basis of six criteria of scientific methodology. The findings of 6 articles that met all 6 criteria and the results of 22 additional studies that met 4 or 5 criteria are presented. We concluded that ulnar sensory and motor nerve conduction studies and needle electromyography performed by physicians with training in electrodiagnostic medicine are valid and reproducible clinical laboratory studies that confirm a clinical diagnosis
Abstract
of ulnar neuropathy at the elbow with a high degree of sensitivity and specificity. Clinical practice recommendations are made based on the literature review of several different ulnar nerve conduction study techniques.
The Quality Assurance (QA) Committee of the American Association of Electrodiagnostic Medicine (AAEM) is charged to develop practice guidelines for the use of electrodiagnostic studies (nerve conduction studies, evoked potentials, and needle electromyography) for the evaluation and management of clinical problems.
Overview
This report is an educational effort by the AAEM, based upon a systematic review of the scientific literature which purports to provide evidence of the usefulness of nerve conduction studies (NCSs) and needle electromyography (EMG) for the diagnosis of ulnar neuropathy at the elbow (UNE). The committee was charged by the AAEM Board to perform a literature review to provide recommendations for the use of NCS and EMG in the evaluation of patients with symptoms and signs suggestive of UNE. The study was a critical review of the literature conducted and supported solely by the AAEM.
Justification
UNE was chosen for review because it is a common clinical problem, a frequent cause for patient referral for electrodiagnostic evaluation, and because the electrodiagnostic workup is sometimes vexing. British clinicians have commented eloquently on the vicissitudes of the electrodiagnosis of UNE.4,75
The sort of epidemiologic information available for carpal tunnel syndrome (CTS) does not seem to exist for UNE.44 The incidence of nerve compression syndromes seems to be increasing and the etiologic spectrum of UNE has changed over the years. Fewer cases due to obvious trauma and gross elbow deformity are being seen now than in the past, and more cases are being seen which appear to be idiopathic or related to the activities of work or daily living. This shift in the causes of UNE has significant implications both for diagnosis and management.27
Some clinicians diagnose UNE on clinical grounds alone and eschew electrodiagnostic evaluation altogether, relying particularly on the presence of Tinel’s sign to localize a lesion to the elbow, even though this sign may occur in normal patients.83 Other reported examination techniques include the elbow flexion test, pressure provocation and a combination of elbow flexion and pressure provocation.27,69
Brown and colleagues recently debated the issue of the interplay of clinical and electrodiagnostic data in the evaluation of patients with focal neuropathies in general.11 Most clinicians would agree that there is potential to improve the care of patients with symptoms and signs suggestive of UNE with laboratory studies that improve the reliability of the diagnosis of UNE.
The literature review was conducted in a manner which would permit others to access the same literature for review in order to verify the study’s conclusions. We began by reviewing the methodology developed for the AAEM Practice Parameter for Electrodiagnostic Studies in Carpal Tunnel Syndrome. We concluded that six criteria similar to those used in the CTS study could be employed to evaluate the literature on the electrodiagnosis of UNE.44
Description of the Review Process
Six Literature Classification Criteria1. Prospective study. A prospective study design permits uniform collection and analysis of data. 2. Diagnosis of UNE in the patient population based on clinical criteria independent of the electrodiagnostic procedure under evaluation. Use of clinical criteria for the diagnosis of UNE permits identification of a defined population in which to test the sensitivity of the electrodiagnostic procedure. The clinical criteria include, but are not limited to, a history of numbness and paresthesias in an ulnar distribution, weakness or wasting of ulnar innervated muscles, history of elbow trauma, elbow deformity, and the presence of a Tinel’s sign. 3. Electrodiagnostic procedure described in sufficient detail, or reference provided to a published technique, to permit duplication of the procedure; the position of the elbow was stated and the same elbow position was used throughout the study. An adequate description of the procedure permits duplication of the study for confirmation of the results and subsequent use in the clinical laboratory. Knowledge of the elbow position used is crucial to the interpretation of conduction study results. 4. Limb temperature monitored and reference values reported. The speed of sensory and motor nerve conduction is temperature dependent. 5. Reference values for the electrodiagnostic procedure obtained either (a) with concomitant studies of a reference population or (b) with previous studies of a reference population in the same laboratory. The results of the electrodiagnostic procedure in control subjects determine the specificity of the procedure in UNE patients. 6. Criteria for abnormal findings clearly stated, and if the measurement is a quantitative one, the criteria for an abnormal value defined in statistically computed terms, e.g., range, mean + 2 standard deviations (SD), from data derived from the reference population. Use of standard statistical terms permits computation of the sensitivity and specificity of the electrodiagnostic procedure and comparison of the procedure to other electrodiagnostic and nonelectrodiagnostic tests for UNE.
The six criteria were listed on a review sheet followed by a forced yes or no choice indicating whether the article fulfilled each criterion. Each article was reviewed by two reviewers; when disagreements arose, a third reviewer discussed the article with the two initial reviewers and a consensus reached. Articles were ranked in terms of the number of criteria met. Table 1 lists those articles meeting four, five or six of the literature selection criteria.
The source of the articles reviewed was a Medline search for literature in English from 1983 through 1994 under the Medical Subject Headings (MESH) (1) ulnar nerve, (2) electrodiagnosis, (3) nerve compression syndromes, (4) neural conduction, and (5) elbow. The literature search was conducted again in January 1996 to discover newly published articles. The initial search generated 282 article titles with abstracts. The abstracts were reviewed by two AAEM QA committee members. Of the 282 articles, 56 reports referring to electrodiagnosis and other laboratory studies to evaluate UNE were found and reviewed. The bibliographies of these 56 reports were examined and additional articles identified and reviewed. In total, 398 titles, abstracts or papers were evaluated for inclusion in the review.
Tables were constructed to summarize the data in the articles. Because of the paucity of articles meeting all six criteria, the tables include articles meeting five or six criteria. Although the AAEM CTS review excluded studies using needle stimulation or recording electrodes, eliminating such investigations for the UNE literature would have eliminated several important papers, including the classic study of Payan.74 Details of technique are discussed in the text and legends to the tables.
The tables describing the results of conduction studies were to include the following information:
1. Author (date). 2. Control subjects:
a. Number of elbows (subjects). b. Mean (range) age. 3. Test parameters:
a. Conduction distance in centimeters. b. Distal elbow stimulation site. c. Proximal elbow stimulation site. d. Elbow position. 4. Range (or lower limit) of arm temperature. 5. Distal latency. 6. Conduction velocity over various ulnar nerve segments as described in the article, generally expressed as mean + SD. 7. Abnormal value, generally the 95% limits of normal. 8. Basis of choice of abnormal value, generally mean + x SD (usually 2). 9. Percentage of normal arms with abnormal test results (calculated or actual). 10. UNE patients:
a. Number of UNE elbows. b. UNE subjects’ age as mean (range). 11. Percentage of symptomatic elbows with abnormal studies.
Where applicable, some tables include other data as well, especially regarding technique. Since criterion 2 does not apply to normal control subjects, studies reporting reference values only and meeting the remaining five review criteria were included in separate tables.
The measurement of ulnar conduction velocity across the elbow varies remarkably with the degree of elbow flexion, and elbow position is an important variable in studies reporting reference values or UNE patient data. Because different investigators have used various elbow angles, studies were grouped into different tables as follows: studies done with the elbow extended (0º flexion, referred to by some authors as 180º), studies done in slight flexion (20º45º), studies done in moderate flexion (70º-90º), and studies done in full flexion (-135º). The language used in describing elbow position can be deceptive (see below).
The review and writing processes required the voluntary efforts of 11 AAEM physicians and a total of approximately 558 hours, as follows: literature search (3 hours), abstract selection and review (10 hours), article review and classification (120 hours), data assembly from selected articles (65 hours), preparation of tables (130 hours), and preparation and review of text and bibliography (270 hours). In addition, the project cost approximately $1850 for librarian, secretarial, and communication (postage, fax and electronic mail) services. Publication costs were approximately $1500.
A number of problems arise in evaluating suspected UNE. There are several potential sites of ulnar compression in the region of the elbow which may have different electrodiagnostic pictures.1,17,18,32,61 The clinical manifestations of disease at the wrist, elbow and more proximal sites can be similar. The nerve’s branching pattern limits both clinical and electrodiagnostic localization.100 Selective vulnerability may produce varying degrees of involvement of different fascicles.87 Forearm muscles are often spared in lesions at the elbow.15 Lesions of the brachial plexus and lower cervical roots may cause signs and symptoms which closely simulate UNE. Patients with anterior horn cell disease and myelopathies may develop hand muscle wasting resembling that seen in UNE. The sensory symptoms of UNE can mimic those of cervical radiculopathy, plexopathy and ulnar lesions at the wrist or upper arm.
Background
In the face of these clinical limitations, electrodiagnosis should play an important role in sorting out the pathology and localizing the lesion. However, the electrodiagnostic evaluation of ulnar neuropathies has met with a number of problems. Patients with purely sensory symptoms frequently have unrevealing electrodiagnostic evaluations. Elbow position markedly influences the measurement of ulnar conduction velocity (CV), and there has been great difficulty reaching agreement on the best elbow position for NCSs. The optimal segment length for across elbow NCSs remains debatable. UNE in some patients affects amplitude and area parameters more than CV parameters, and the relative importance of conduction block vs. conduction slowing is disputed. Lesions characterized predominantly by axon loss may be even more difficult to localize by conduction studies alone, and needle EMG plays a key role in such instances. Lastly, a terminologic morass has grown out of imprecision in the use of terms such as tardy ulnar palsy and cubital tunnel syndrome.
The ulnar nerve may sustain compression injury at three different sites in the region of the elbow: the retroepicondylar groove (most common), the humeroulnar arcade (HUA) [the “cubital tunnel”], and the point of exit from the flexor carpi ulnaris (FCU) muscle (least common). After traversing the ulnar groove with its sparse protective covering, the nerve dips beneath the HUA, a dense aponeurosis which typically lies 1.0 - 2.0 cm distal to the medial epicondyle and forms the origin of the FCU muscle. Credit for the first description of ulnar compression at the HUA rightfully goes to Buzzard and Sargent.31 Fiendel and Stratford later coined “cubital tunnel syndrome” to refer to compression by the HUA, but the term has since become a nonspecific generic for any UNE.32 After passing beneath the HUA, the nerve runs through the belly of the FCU, then exits through the deep flexor-pronator aponeurosis lining the under surface of the muscle 4.0-.0 cm beyond the medial epicondyle, another potential entrapment site.1,18
Pathophysiology of Ulnar Neuropathy at the Elbow
Retroepicondylar compression may result from external pressure, as from habitual leaning on the elbow. Prolonged external pressure likely accounts for most postoperative UNEs, some of which may remain asymptomatic.63,97 Important anatomical changes occur with movement of the elbow. In extension, the medial epicondyle and olecranon are juxtaposed with the HUA slack and the nerve lying loosely in the groove. With elbow flexion, the olecranon moves forward and separates from the medial epicondyle, progressively tightening the HUA across the nerve.5,96 Pressure between the HUA and the nerve may rise from 0-19 mm Hg in extension to >200 mm Hg with flexion combined with isometric contraction of the FCU.98 In extension, the ulnar groove is smooth, round and capacious while in flexion it is flattened, tortuous, narrow, and inhospitable.5 With extreme flexion, the medial head of the triceps pushes against the nerve posteriorly, additionally narrowing its passageway and fostering subluxation.16,90 These anatomical relationships account for the susceptibility of the ulnar nerve to injury at the elbow.
With elbow joint derangement due to trauma or arthritic changes, the nerve’s vulnerability increases even further. Valgus deformities increase the stretch on the nerve with elbow flexion, and osteophytic overgrowth further narrows an often already narrow passageway.86 UNEs may occur bilaterally, especially when there is HUA entrapment.26,41,61 Diabetes mellitus and rheumatoid arthritis are the two systemic diseases most likely to have a complicating UNE.6,26
Nerve compression or entrapment may cause focal demyelination or axon loss, or any combination of the two. Remyelination with short, slowly conducting internodes adds another consideration to the interpretation of conduction studies. Focal demyelination may produce either (1) conduction block, (2) uniform or synchronous slowing affecting all fibers equally, or (3) differential or asynchronous slowing affecting fibers to varying degrees.99 Combinations of these may coexist. UNEs which only cause axon loss are often very difficult to localize, and some authorities believe pure axon loss is the most common pathophysiology in UNE.99,100
The internal fascicular organization of the nerve and varying susceptibility of different fascicles to injury may explain some of the puzzling diversity in clinical expression of ulnar neuropathies.15,87 The fibers to the first dorsal interosseous (FDI) seem more susceptible to injury than those to the abductor digiti minimi (ADM).74,87 Different fascicles may exhibit different pathophysiology, with conduction block affecting fibers to the FDI while those to the ADM display a pure axon loss picture. Anomalous innervation should always be excluded in such circumstances.87,100 Fascicles innervating forearm flexors and the fascicles comprising the dorsal ulnar cutaneous branch may paradoxically escape injury with lesions at the elbow.
In 1956, Simpson first described focal slowing in a chronic traumatic lesion of the ulnar nerve at the elbow.84 He demonstrated slowing through the affected region with relatively normal conduction in segments above and below the lesion, setting the future pattern for evaluating suspected UNE. In 1960, Gilliatt and Thomas evaluated 14 patients with UNE and 15 control subjects, localizing the lesion to the elbow in 13 patients. Even this early investigation included an effort to study nerve action potentials (NAP) and to record from both the ADM and FDI.36
Review of Electrodiagnostic Studies
Spiegel, Johnson and Schubert examined the difference in conduction velocity between proximal and distal ulnar segments in normal control subjects.82,85 Kaeser was one of the first to perform ulnar conduction studies with the elbow flexed, and to use a short segment technique.46
Carpendale developed a four-point segmental technique stimulating axilla (AX), above elbow (AE), below elbow (BE), and wrist (W); and reported its value in two patients.21 Elbow position was not reported, nor was temperature monitored or results discussed in statistically meaningful terms. Melvin and colleagues did an early study of NAP CV in normal median and ulnar nerves.60
Recurrent issues in the electrodiagnosis of ulnar neuropathy have been elbow position, optimal length for an acrosselbow segment, the value of absolute vs. relative across elbow slowing, motor and sensory potential amplitude and configuration changes across the elbow, and evaluation of the patient with purely sensory symptoms and normal motor conduction studies.
Anatomical factors influence the electrodiagnosis of UNE. In extension, the nerve lies lax and redundant, lightly coiled in the retroepicondylar groove. Through slight to moderate flexion, the nerve uncoils and becomes progressively more taut, and the overlying skin stretches. With further flexion, the nerve itself begins to stretch and move distally, and with extreme flexion the nerve may partially or completely sublux out of its groove.40 Any discrepancy in the elbow position used for stimulation and that used for measurement is a major potential source of error. Electrodiagnostic medicine consultants should also realize surgeons operate with the elbow in slight flexion, generally 20º-45º, never in full extension or even moderate flexion.
Elbow Position
With the elbow in full extension, the distance over the skin surface measures considerably less than the true nerve length, resulting in a falsely short distance and an artifactually slow CV. Skin surface measurements more realistically approximate nerve length in slight-to-moderate flexion.23 In more extreme flexion, the nerve may migrate distally up to 1.4 cm. (W.W. Campbell, personal observations on 29 cadaver elbows). Harding and Halar found a mean distal movement of 1.3 cm on full flexion in 4 cadaver elbows.40 In addition, the ulnar nerve subluxes out of its groove in about 18% of normal individuals, and may rest on the lip of, or come to lie completely anterior to, the medial epicondyle.90 In effect, the subluxed nerve takes a shortcut across the elbow, and conduction studies done in full flexion run the risk of a falsely long skin distance measurement and a falsely fast CV: the inverse of the problem of studies done in extension.
The language used in describing elbow position can be ambiguous and problematic. In the classic paper of Checkles and colleagues,23 the statement that the elbow was flexed at 70º has been widely misconstrued to mean partial flexion with an obtuse angle at the elbow. In fact, Checkles and colleagues used extreme flexion with an acute angle at the elbow (personal communication, N. Checkles, 1996). Felsenthal, in contrast, in referring to 70º, meant partial flexion with an obtuse angle at the elbow (personal communication, G. Felsenthal, 1996). For purposes of this paper, full extension is 0º of flexion, angles less than 90º refer to partial flexion with an obtuse angle between the arm and forearm, and angles greater than 90º refer to the fully flexed position with an acute angle between the arm and forearm.
Most early studies of ulnar neuropathy were done with the elbow in full extension.21,36,74,82,84,85 Remarkable slowing in the across elbow segment in extension has been reported in normal control subjects. Tackmann and colleagues found up to 20 m/s slowing across the elbow in normal subjects, Rosenfalck up to 30 m/s in a single normal subject.81,91 Numerous other authors have reported similar findings.45,54,74
Checkles and colleagues, in a landmark paper, compared ulnar CV in flexion and extension.23 They found the mean across elbow CV 1.5% faster than the forearm segment with the elbow flexed to 110º, but 20% slower with the elbow extended.
Payan used near nerve needles for sensory recordings, then the same needles for motor stimulation; he kept the elbow extended for greater convenience in placing the needles.74 Checkles and colleagues recommended 70º (actually 110º) of flexion.23 Harding and Halar concluded 45º of flexion provided the least variability for motor conduction studies, with artifactually slow CVs in extension and artifactually fast CVs at 90º and 135º of flexion.40 Kincaid and colleagues studied normal control subjects in 135º of flexion, assuming this would provide maximal elongation of the nerve across the elbow and eliminate the measurement error complications.53 They also found the 135º flexed elbow position allowed supramaximal stimulation at lower stimulus intensity and increased the ease of stimulus site location compared to the extended position. Miller is now persuaded that the 135º flexed position is the preferable one.62
Patients with UNE have been studied in extension9,43,48,54,74,77,79 (Table 3), slight flexion8,91 (Table 4), and moderate flexion9,54 (Table 5). The only studies of UNE patients with the elbow in extreme flexion are in the minimonograph by Kincaid, and the format of that discussion does not lend itself to extraction of the data into tabular form.52
Two investigations reached different conclusions regarding the yield of extended vs. flexed elbow positioning in the diagnosis of suspected UNE. One found no significant difference in diagnostic sensitivity between the two positions for detecting abnormalities in patients with UNE defined on the basis of clinical symptomatology.9 The other found the 90º flexed technique detected all of 35 UNEs but the extended technique found only 5 of the 35 (14%).54 However, this investigation used the results of NCSs, rather than clinical criteria, to define patients as having UNE and conclusions about the relative sensitivity of the two positions in detecting clinically defined UNE must be drawn cautiously.
Early UNE investigators are generally silent on the issue of the length used for studying the across elbow segment. In 1972, Maynard and Stolov published an influential paper on sources of error in conduction studies, concluding that CVs done over distances less than 10 cm were prone to unacceptably high experimental error.59 Latency measurement uncertainty accounted for 89% of the error and distance measurement for only 11%. Distance error consisted predominantly of skin movement errors rather than tape measure reading errors. The authors noted that if errors of the magnitude found in their investigation occurred in previous studies on normal ulnar CV, then true biologic variation may have accounted for only half the total variation reported.
Segment Length
Following Maynard and Stolov, most investigators and clinicians adopted a minimum 10 cm across the elbow
distance.9,43,54,77 Harding and Halar concluded the optimal across elbow segment length was 12-14 cm.40 The mean across elbow segment length used by Kincaid and colleagues was 12.9 cm.53
However, it is obvious and well recognized that the study of long nerve segments may mask focal slowing by including lengths of normally conducting nerve, thus diluting any focal abnormality. A reciprocal relationship may then exist between experimental error and sensitivity for lesion detection.40,53,78 Kaeser, in 1963, had studied segments as short as 2 cm.46 Other investigators have successfully used very short segments in the study of UNE, either percutaneously or intraoperatively.12,13,17,20,47 Kimura popularized short segment techniques in evaluating CTS, later stating: “A large per-unit increase in latency more than compensates for the inherent measurement error associated with multiple stimulation in short increments.”50 The need to distinguish between different sites of involvement in UNE, the retroepicondylar groove versus HUA (cubital tunnel), makes the issue of segment length even more critical.17 See the section on short segment studies for further discussion of this issue.
Two methods to detect focal slowing in the across elbow segment are to compare the absolute CV value to normal reference values determined in like manner for the across elbow segment, and to compare the relative CV of the across elbow segment to the CV of another segment of the same nerve. Axon loss distal to a focal lesion at the elbow may cause slowing in the forearm segment, so that the AE-to-W, BE-to-W, and AE-to-BE segments are all slow, and the additional focal abnormality, directly due to the elbow lesion, less readily detectable. Theoretically, with milder lesions the across elbow segment will show abnormalities while the BE-to-W (forearm) segment will not.Comparisons of the across elbow CV to the axilla to AE segment or to the median nerve CV are possible but have seldom been attempted. Kincaid summarized published normal values for the axilla-to-elbow segment, which range from 43-52 m/s.29,46,52
Absolute Versus Relative Conduction Velocity
Various criteria have been proposed for assessment of the relative across elbow motor nerve conduction velocity (MNCV). Krogness advocated calculating a ratio between the AE to W and the BE to W velocity.55 Eisen arbitrarily picked 10 m/s difference between the AE-to-BE and BE-toW segments as the lower normal limit (following the method of Payan, elbow extended), even though Payan had found a normal mean relative slowing range of 17 m/s, and Eisen’s 10 m/s criterion included 14.6% of his normal control subjects.29,74 Some authors conclude such slowing across the normal elbow reflects subclinical, incidental UNE.29,43,70 Odusote and Eisen surmised subclinical UNE was present in 30% of their control subjects over the age of 60.70 There is some pathologic support for this conjecture.67 It is nevertheless difficult to believe that subclinical UNE is more important than technical factors, primarily elbow position, in explaining the across elbow slowing reported in normal individuals.
Absolute MNCV lower limits in m/s for across elbow conduction reported in normal control subjects include: elbow extended - 32,77 34,23 35,61 38,29 38,53 41,45 44,74 4643; elbow slightly flexed - 43,8 51,40 5391; elbow moderately flexed - 51,54 52,23 549; and elbow fully flexed - 49.53
Relative MNCV upper limit differences in m/s reported between the across elbow and forearm segments (i.e., [BEW CV] - [AE-BE CV]) in normal control subjects include: elbow extended - 7,9 10,29 26,38 3077; elbow slightly flexed 1240; elbow moderately flexed - 10,38 179; and elbow fully flexed - 11.52,53
Differences in MNCV between the across elbow and forearm segments in normal control subjects have also been reported as a percent value: [(BE-W CV)-(AE-BE CV)/(BEW CV) x 100]. Upper limits reported in per cent decrease in the across elbow segment relative to the forearm segment include: elbow extended - 46%,23 18%48; elbow moderately flexed - 7.6%.23
Bielawski and Hallett found the yield of absolute MNCV determinations was higher than relative calculations.9 In 20 patients with clinical UNE and both motor and sensory deficits, Kincaid found 86% had absolute MNCV slowing over the elbow segment, while only 46% localized to the elbow by relative slowing criteria because the forearm velocity was also slow.52
Recording sensory or mixed nerve action potentials (NAPs) poses more difficulties than recording M-waves, with more pitfalls and sources of error and uncertainty. The smaller potentials create greater problems controlling shock artifact and with extracting the signal from the noise.Techniques are much more varied. Different investigators have used surface or needle recordings, used different points on the NAP to measure latency and amplitude, as well as used different elbow positions.
Nerve Action Potential Studies: Sensory or Mixed
Conversely, NAP studies have potential utility. Payan believed sensory fibers were first to be affected in UNE.74 The common occurrence of predominantly sensory symptoms and normal routine motor NCSs repetitively substantiates the shortcomings of conventional methods, and makes techniques for studying sensory fibers theoretically attractive. The appeal of sensory studies is apparent in even the earliest studies of the electrodiagnosis of UNE.36 Surface and near nerve needle recording techniques each have advantages and disadvantages.10
The amplitude and duration of the NAP, much more so than the M-wave, vary with the distance between stimulation and recording sites. The fastest and slowest conducting fibers increasingly separate over distance, prolonging the NAP duration.50 Phases of the NAP with similar velocity but opposite polarity may cancel out to produce significant amplitude decrements over distance even under normal circumstances.50,51
The length of nerve segment studied correlates linearly with NAP amplitude, duration and area.51 Payan found NAP amplitude decreases up to 50% and duration increases up to 50% from BE to AE in normal control subjects.74 Other investigators have reported BE-to-AE NAP decrements in the 40% range in normal control subjects.53,91
The NAP amplitude and shape vary as well with (1) the distance between the potential’s origin and the recording electrode, (2) the recording technique, and (3) whether potentials were obtained orthodromically or antidromically. When recording the orthodromic NAP, particularly with surface electrodes, amplitude may be decreased even BE due to the nerve’s buried position in the FCU.53 Payan commented that his normal NAP amplitude values differed from those of Buchthal and Rosenfalck merely because he had used the motor threshold as a guide for placing the near nerve needles, rather than placing them blindly.74 With all these variables, deducing the expected normal orthodromic surface NAP amplitude at the AE site of an obese elbow seems fanciful.
The NAP is composed of a multitude of individual spikes. Desynchronization of the NAP into individual fragmented components occurs with increasing age in normal control subjects. Payan, using near nerve needle recording, found marked desynchronization of NAPs at all levels in normal control subjects over 70 years old.74 Martinez and colleagues, studying surface recorded orthodromic sensory and mixed NCV in normal control subjects of varying ages for different ulnar segments, found the NAP recorded AE was desynchronized in 13% of their subjects, mostly those over the age of 50 years.58
A decrease in M-wave amplitude or area at the AE site compared to the BE site may signal conduction block due to a focal demyelinating lesion, but the acceptable normal limits of across elbow amplitude change remain unclear.The topic of conduction block is complex and the details are beyond the limits of this discussion.24,71 Conduction block generally occurs as a transient process, either progressing to axonal degeneration or resolving with remyelination and repair to leave synchronous or asynchronous slowing. It can rarely persist for long periods.42,65 Conduction block was seen in about one third of UNEs studied intraoperatively.12
Across Elbow M-Wave Amplitude Changes
Only recently have precise criteria and definitions regarding conduction block been proposed.24,71 Most UNE investigators have used a change in the amplitude of the negative peak as an indication of conduction block, and temporal dispersion due to asynchronous slowing as an ancillary sign of focal demyelination. M-wave amplitude and area normally decrement over distance, but to a much lesser degree than NAPs.34,51,95 Some investigators found no significant variation in the amplitude, duration or area of the M-wave negative peak between below and above the elbow in extension or various degrees of flexion.40,51,54,68,91 Checkles and colleagues found negative peak amplitude variation up to 43% between AE and BE, but the larger amplitude usually occurred with AE stimulation, likely reflecting submaximal distal activation. The authors attributed this large variation to technical factors, such as electrode movement.23 Kincaid and colleagues found Mwave amplitude between AE and BE differed by up to 10.5% with the elbow flexed and up to 14% with the elbow extended.53 Stewart found the maximum amplitude decrement between wrist and AE in 40 control nerves was 10%.87 Kothari and Preston defined across elbow conduction block as a >50% drop in M-wave area or >20% drop in M-wave amplitude without temporal dispersion.54
Pickett and Coleman found the M-wave amplitude change from AE to BE in control subjects was -2.2+7.2%, in patients with UNE the change was -14.5+24.2%. The authors concluded the best way to localize a ulnar nerve lesion to the elbow was by a drop in motor amplitude >25% across the elbow.77 Having found M-wave amplitude changes more useful than CV changes, regression analysis was employed in a subsequent paper, using the distal motor amplitude to predict the proximal motor amplitude in order to detect conduction block or temporal dispersion. The regression predicted AE amplitude was more sensitive than the percentage drop in amplitude for localizing UNE.76
Felsenthal and colleagues found the below-to-above elbow M-wave amplitudes recording from hypothenar muscles did not differ by more than 7%-10%, but recording from FCU or flexor digitorum profundus was associated with much greater variability.33,34 Side-to-side across elbow MNCV should not vary by more than 9.5 m/s, or side-to-side Mwave amplitude differ by more than 50% when recording from any muscle studied.33
Miller popularized the “inching” technique, in which the stimulator is moved in short stepwise fashion around the elbow in search of areas of abrupt change in amplitude or configuration signifying immediately subjacent demyelination.61 A decrease of M-wave amplitude >30% or a change toward a desynchronized response was considered localizing. This method can very accurately localize the pathology when conduction block or differential slowing is present. See the section on short segment studies for further discussion.
Anomalous fibers connecting the median to the ulnar nerve in the forearm, the Martin-Gruber anastomosis, occur in 15%-20% of normal individuals.39 Some studies report incidences over 30% when recording from the FDI.3,89 Rarely, ulnar-to-median communication occurs.37,88 Anomalous innervation may explain paradoxical sparing of ulnar innervated muscles in an apparent UNE.28,93 The presence of a forearm anastamosis may simulate ulnar conduction block at the elbow, especially when recording from the FDI, the most frequent muscle to have anomalous innervation, or when the BE stimulation site is relatively distal.89 Anomalous innervation must be ruled out in any instance of apparent ulnar conduction block at the elbow.
Temperature
Temperature has well recognized effects on nerve conduction. Unfortunately, some important early studies of ulnar neuropathy did not include temperature measurements and monitoring.8,23,45 Tackmann and colleagues did studies at 36º and Bielawski and Hallett corrected conductions to 36º, their mean AE-to-BE MNCV values of 66 and 61 m/s, respectively, are 4-14 m/s faster than most other investigators who did studies at 34º.9,43,48,54,74,91
Traditionally, electrodiagnostic reference values have been derived by determining the mean+2SD in control subjects. Recent studies suggest this approach may be too simplistic. The distribution curve for some conduction parameters significantly skews from the normal, bell-shaped Gaussian distribution, making a mean+2 SD definition of normality inaccurate to a clinically important degree.19
Statistics
Robinson and colleagues found a significantly positive coefficient of skewness (g1) for 5 of 8 amplitude and 6 of 8 latency measurements in 22 NCS parameters, using 75 control subjects. The ulnar M-wave amplitude, motor latency, sensory nerve action potential (SNAP) amplitude and sensory nerve conduction velocity (SNCV) all demonstrated significant skew. Raw data can be transformed (“deskewed”) toward a more normal distribution using various mathematical operations. In a group of 66 diabetics, use of mean+2SD, mean+2.5SD and range of the raw data produced significant positive and negative misclassifications as compared to transformed data. The authors concluded analyses using raw data to derive normal limits result in an unacceptable rate of misclassification, and normal limits should be derived from the mean+2SD of the optimally transformed data.80
Failure to find abnormalities in patients felt certain to have a disease may lead to the performance of multiple tests, hoping to confirm the clinical suspicion. No diagnostic test perfectly discriminates between normal and abnormal.Using the common mean+2SD approach and a normal distribution, 95% of the control population will fall within the limit from -2SD to +2SD, and 2.5% of the control subjects will fall beyond the limits of the curve at either end. Electrodiagnostic data do not classify as abnormal individuals with NCVs “too fast,” latencies “too short” or amplitudes “too large,” so that approximately 2.5% of normal subjects will be mistakenly called abnormal (type I error).
If tests are independent, the 2.5% error summates with each additional procedure. A person who has two tests runs a 5% risk of being called abnormal, four tests 10%, and so on. While additional testing will identify more abnormal subjects, it also increases the likelihood of misclassifying a normal subject as abnormal. Even after accounting for interdependency, the total error of combined tests may be unacceptably high. Increasing the number of critical value SDs to 2.5 or 3.0 decreases the type I error rate, but increases the type II error rate (abnormals considered normal). If a single, highly discriminating test is not available and multiple tests are used, diagnosis should rest on a pattern of multiple, internally consistent abnormalities to distinguish between normals and abnormals.
The article review process was designed to ensure all articles cited used comparable scientific methods. Some variation in result is expected even with identical techniques because the percentage of abnormal values depends on several factors including (1) the number of and selection process for the normal subjects, (2) the number of and selection process for the UNE patients, and (3) the numeric values chosen as the normal limits for NCS.
Results
A total of 19 articles of the 398 articles and abstracts met 5 or 6 literature classification criteria (Table 1); 6 articles were excluded from subsequent analysis for various reasons.13,22,36,70,87,92 For example, some investigators performed ulnar conduction studies in the course of looking primarily at other phenomena, such as the effects of age on the conduction properties of multiple nerves, the correlation between clinical and electrodiagnostic findings, or the difference between proximal and distal nerve segments; the findings therefore have scant or no applicability to the evaluation of the clinical problem of UNE. Studies of normal control subjects met a maximum of 5 of 5 criteria; studies of patients with UNE met a maximum of 6 of 6 criteria.
The 13 articles selected for Tables 2-7 met 5 or 6 literature classification criteria. These studies included 564 patients with ulnar neuropathy and 702 normal controls. Tables reporting normal reference values are separated from those reporting results in patients with UNE; both normal reference value tables and patient tables are grouped by the elbow angle employed into extension, slight flexion, moderate flexion, and full flexion, as detailed above.
Table 2 presents the results of four studies of ulnar MNCV in normal subjects. Most investigators used surface stimulation and recording.23,40,53
Normal Motor Nerve Conduction Velocity Reference Value Studies
Checkles and colleagues studied ulnar MNCV in the across elbow and forearm segments in 18 normal persons in full extension and in flexion at 110º from the horizontal.23 (Table 2) They did not measure or control temperature. Mwave duration and amplitude were not affected by elbow position. MNCVs were highest across the elbow when flexed. Compared with the forearm segment, MNCV across the elbow was 1.5% faster in flexion; 20% slower and with much greater variation in extension. From a cadaver dissection, the authors concluded the true length of the ulnar nerve across the elbow segment is more accurately measured with the elbow flexed. They judged that performing ulnar conduction studies with the elbow in the 110º flexed position would enhance precision.
Harding and Halar studied ulnar motor and sensory CV across the elbow in four different increments of elbow flexion: 0º (full extension), 45º, 90º, and 135º (full flexion); finding 45º was the position of least variation between the across elbow and forearm MNCVs.40 After cadaver studies showed a mean difference in movement between skin and nerve markers of 1.3 cm in extreme flexion, the authors concluded the quickening of MNCV with more extreme elbow flexion was spurious and artifactual, and mostly due to stretching of the skin over the flexed elbow producing disproportional movement between the skin surface and the underlying nerve.
Kincaid and colleagues evaluated 50 normal subjects to assess the influence of elbow position and nerve segment length on CV values and to define normal sensory CV values.53 Motor conduction studies done with the elbow fully extended were compared with those done in 135º of flexion. Mean length of the AE-to-BE segment with the elbow flexed was 12.9 cm. The mean MNCV for the segments AE to W, AX to W, and AE to BE with the elbow extended were significantly slower (59.0, 59.1 and 50.3 m/s, respectively) than with the elbow flexed (63.0, 62.6 and 62.8 m/s, respectively), numbers uncannily echoing Checkles and colleagues.23 With the elbow flexed, 96% of the subjects had an AE to W CV no more than 4.7 m/s slower than the BE to W CV. When considering the elbow segment itself, the AEto-BE segment was up to 11.4 m/s slower than the BE-to-W segment. The slowest CV from AE to BE recorded in a normal subject in 135º flexion was 49 m/s.
Studies in patients with ulnar neuropathy at the elbow
Studies done in patients with UNE are arranged into sections dealing with motor NCS grouped by elbow position, sensory NCS, results of recordings from forearm flexors, short segment studies and needle examination findings.
Motor Conduction Studies in Patients with Ulnar Neuropathy at the Elbow
Studies done in patients with ulnar neuropathy at the elbow and using the elbow extended position. (Summarized in Table 3.)
Payan (criteria met 6/6) studied ulnar motor conduction in 50 patients with UNE and in normal control subjects, stimulating with needle electrodes already placed for NAP studies, recording with a concentric needle electrode from both the ADM and FDI.74
In UNE patients, the distal motor latency was prolonged in 40%, and 75% had MNCV slowing in the forearm. In 85% trans-sulcal slowing was evident recording from both FDI and ADM, in 75% using only one muscle. M-wave amplitude changes across the sulcus were not found to be of value. Motor studies were localizing in 35 of 50 cases, 25 because of trans-sulcal slowing and an additional 10 because of increased latency to the FCU. (See also Table 7) Although 85% of cases showed trans-sulcal MNCV slowing, only 50% localized to the elbow because of the high incidence of forearm slowing. Using all available electrophysiological methodology, 48 of the 50 lesions were localized to the elbow.
Pickett and Coleman (criteria met 6/6) studied 61 focal ulnar nerve lesions in 50 patients, using 210 nerves in 172 patients as control subjects.77 The ulnar nerves of patients with polyneuropathy were studied as well. Conduction velocity from AE to BE was as slow as 32 m/s in control subjects (mean + 2 SD), and the calculated cutoff point for the lower limit of normal AE-to-BE velocity was 22 m/s. In UNE patients, motor and sensory amplitudes were affected more than conduction velocities, and the authors concluded the best way to localize an ulnar lesion to the elbow was a drop in motor amplitude >25% across the elbow.
Kimura (criteria met 6/6) examined motor and sensory conduction parameters in 64 symptomatic elbows of 44 patients, using 32 normal control elbows.48 All their patients were clinically felt to have ulnar entrapment at the HUA. Sensory findings are discussed in the sensory results section. Using motor conduction studies, 81% of symptomatic elbows showed abnormal CV. No abrupt changes in sensory or motor potential amplitude occurred on inching studies around the elbow in any patient.
Hawley and Capobianco (criteria met 6/6) compared patients with UNE alone with UNE superimposed on a diabetic or nondiabetic (mostly alcoholic/nutritional) generalized axonal peripheral neuropathy.43 These investigators used monopolar needle recording from the ADM, stimulating BE, AE and axilla percutaneously. Normal control subjects had up to 22 m/s slowing (mean 10.7 m/s) of CV across the elbow compared to the brachial segment. The proposed criterion of 13 m/s as the upper normal limit of across elbow slowing, while detecting 84% of patients with isolated UNE in this study, also included half the normal control subjects.
Bielawksi and Hallett (criteria met 6/6) studied the yield of abnormality in flexion vs. extension in patients with a clinical diagnosis of UNE, finding no major differences between the two positions except that normal values varied.9 The yield of abnormal findings was greatest from measuring absolute motor CV across the elbow as opposed to comparing the difference in velocities between the elbow segment and either adjacent segment.
Kothari and Preston (criteria met 5/6) compared the utility of a 90º flexed vs. an extended elbow position in demonstrating focal slowing at the elbow, relative to the forearm segment, in 35 patients with UNE, using 50 control subjects.54 Patients were considered to have definite electrophysiologic localization to the elbow by either (1) conduction block across the elbow, defined as >50% drop in M-wave area or >20% drop in M-wave amplitude without temporal dispersion, or (2) focal slowing exceeding 2 SD below the mean of the controls demonstrated in one of the two positions (see also Table 5). All 35 patients demonstrated focal slowing in flexion, whereas only 5 of the 35 did so in extension. The study concluded that the flexed position is more sensitive in localizing UNE.
Eisen (criteria met 4/6) studied 56 instances of mild and 34 instances of severe UNE, and 48 control nerves.29 A relative across elbow MNCV drop of 10 m/s was deemed the lower limit of normal, even though it included 14.6% of the control subjects. Of the mild UNE patients, 19.7% had a 10 m/s or more fall in the across elbow MNCV; 53% of the severe UNE patients had such a fall. Measurement of proximal (AE) motor latency to the ADM was believed to have more value than across elbow MNCV. In the subsequent study with Odusote no attempt was made to do BE stimulation or calculate across elbow velocities.70
Odusote and Eisen (criteria met 5/6) studied 239 cases of UNE and developed clinical and electrophysiologic grading systems which they used to correlate electrodiagnostic findings with clinical severity.70 They used an extended elbow position, did not monitor temperature, attempted no BE stimulation and no BE-to-W or AE-to-BE MNCV determinations (see above). They found 14.6% of the 239 control subjects had an abnormal EMG score. Of the clinically severe UNE cases, 71.4% had abnormal electrodiagnostic evaluations and the diagnosis of “cubital tunnel syndrome” was confirmed “in the majority.” Despite the criteria score of 5/6 and the prodigious number of cases, this paper was not included in the table because of the limited applicability of the MNCV data.
Studies done in patients with ulnar neuropathy at the elbow using slight elbow flexion. (Summarized in Table 4.)
Tackmann and colleagues (criteria met 5/6) studied 103 patients with UNE, 40 with purely sensory disturbances and 63 with sensory and motor deficits, using 52 normal control subjects.91 Needle electrodes were used for motor stimulation, while recording from the hypothenar surface; sensory stimulation was via surface rings while recording was with the same near nerve needles used for motor stimulation; all after the method of Payan.74 Temperature along the nerve was kept constant at 36º C-37º C, generally higher than in other investigations and perhaps contributing to the 5-8 m/s faster CVs reported compared with other studies.
Conduction studies were done with the elbow in 20 degrees of flexion. In normal control subjects, MNCV across the elbow was found to be up to 20 m/s slower and SNCV up to 18 m/s slower than in the BE-to-W segment. Nearly one third of their normal control subjects showed across elbow slowing in the 10-20 m/s range. Eisen’s 10 m/s criterion of abnormality was termed “impractical” by these authors.29 Measuring latency to an ulnar innervated forearm muscle added to the localizing value of motor conduction studies, but measurement of M-wave amplitude was rarely helpful.
Of 63 patients with motor and sensory signs, 41 had slowing of MNCV across the elbow, and 44 had prolongation of latency to a forearm muscle. Of 40 patients with only sensory dysfunction, 13 had slowing of MNCV across the elbow, and another 5 had prolongation of latency to a forearm muscle.
Bhala (criteria met 5/6) investigated 61 control subjects and 78 patients with 117 instances of suspected UNE (elbow flexed to 35º, CNE recording, surface stimulation).8 Of the 78 patients, 51.3% had a MNCV across the elbow of <45 m/s, 42.3% had absent or abnormal ulnar sensory responses in the hand, and 43.6% had abnormal needle EMG.
Stewart (criteria met 5/6) found such variation of MNCV across the elbow that it was not even used as a criteria for the diagnosis of UNE in his series.87 In 40 control nerves, the MNCV varied from 39-100 m/s recording from the FDI and 43-92 m/s recording from the ADM (elbow flexed 30º, 12 cm distance, no temperature monitoring). MNCV from both nerves in the same individual could vary by as much as 40 m/s. An amplitude decrement >20% between W and AE was judged to signify UNE. An abnormal amplitude decrement was detected more frequently when recording from the FDI (68%) than when recording ADM (48%).
Two studies have investigated ulnar neuropathy at the elbow patients using moderate elbow flexion.9,54 (Summarized in Table 5.)
Using the 135º flexion position and the reference values reported in a previous study, Kincaid studied 50 patients with clinical UNE.52,53 In the 40% of patients with both motor and sensory symptoms, 86% had elbow segment motor slowing, but only 48% could be localized to the elbow. The remainder failed to localize because forearm conduction was also slow. In the patients with sensory symptoms only, 48% had elbow segment MNCV slowing and a greater than normal across elbow versus forearm CV difference. Another 16% had a normal absolute across elbow CV, but slowing was detectable by comparison to the forearm CV.
Sensory and Mixed Nerve Conduction Studies in Patients with Ulnar Neuropathy at the Elbow
Studies of sensory or compound NAPs are summarized in Table 6. See previous nerve action potential studies section for a discussion of the theoretical and technical problems associated with NAP studies.
Melvin and colleagues were early advocates of the feasibility and potential usefulness of sensory techniques.60 In 1960, Gilliatt and Thomas found the orthodromic NAP recorded AE with finger stimulation was unsatisfactory because of the small size of the potentials.36 They resorted to nerve trunk stimulation at the wrist and still found considerable amplitude variation, even in control subjects. None of their patients with UNE had recordable NAPs.
Payan (criteria met 6/6) recorded sensory potentials with near nerve needle electrodes at the wrist, 5 cm distal and 5 cm proximal to the medial epicondyle, stimulating with surface electrodes on the small finger, averaging 500 to 1000 responses and measuring the latency to the peak of the first positive deflection, amplitude peak to peak and assessing duration and shape.74 Slowing of SNCV BE to W was seen in 83% of the cases and slowing across the sulcus in 86%. Prolongation of distal sensory latency occurred in 67%. Sensory studies localized the pathology to the elbow in 34 of the 50 cases, 30 because of trans-sulcal slowing. In 4 cases without MNCV or SNCV slowing, the lesion was localized to the elbow by changes in the shape of the sensory potential across the sulcus. Clinically, 7 patients had purely sensory syndromes, 6 of these had damage to motor fibers (6 with slowed MNCV across sulcus and 1 with increased latency to the FCU) and 3 patients with clinically pure motor syndromes had abnormal SNAPs. Payan proposed that sensory fibers were first to be affected in UNE.
Harding and Halar (normal reference study, criteria met 5/6) found that antidromic sensory conduction study (latencies to the peak negative deflection) results paralleled the MNCV findings, but with such large intersubject variability the investigators questioned the validity of sensory CV studies for evaluating UNE.40
Kimura (criteria met 6/6) measured sensory latencies to the onset of the potential.48 All symptomatic elbows displayed slowing of SNCV across the elbow (< 82.8% of the value of the forearm segment); 2 normal control elbows demonstrated abnormal slowing using study criteria.In 25 of 64 symptomatic extremities no sensory potentials could be obtained.
For the antidromically recorded SNCV, taking latencies from the negative peak onset and with the elbow flexed to 135º, Kincaid and colleagues (normal reference study, criteria met 5/6) found 96% of their normal subjects had an AE-to-W segment no more than 3.4 m/s slower than BE to W, and AE to BE no more than 8.5 m/s slower than BE to W. Sensory amplitude recorded in response to stimulation at the AE site was up to 43% smaller than at the BE site.53
Raynor and colleagues (criteria met 6/6) investigated the relative sensitivities of across elbow surface recording studies of elbow extended sensory, mixed nerve, and motor conduction studies in 43 patients with symptoms of UNE and 40 controls.79 Segmental MNCV slowing localized the lesion to the elbow in 67% of patients with clear evidence of UNE by physical examination, but in only 9% who had subtle or no physical examination abnormalities. The diagnostic yield was increased by finding segmental slowing of sensory or mixed nerve CV across the elbow to 86% and 68%, respectively, for each of the groups. Antidromic sensory studies alone were only localizing in 55% of the cases because of the frequent absence of recordable NAPs in patients with more severe lesions. The authors concluded surface recorded sensory and mixed NCSs appeared more sensitive than motor studies, especially in patients with subtle clinical involvement.
In Tackmann and colleagues’ study (criteria met 5/6), SNAP amplitude recorded AE was reduced up to 40% compared to BE in control subjects.91 Orthodromic sensory conduction studies proved helpful in patients with pure sensory disturbances, but in patients with motor deficits sensory potentials were too often absent or abnormal in all segments of the nerve to have substantial localizing value. Sensory parameters alone indicated elbow compression in 24 nerves, with slowing of SNCV across the elbow (12) or changes in the amplitude, duration or number of components of the sensory potential.
Bhala (criteria met 5/6) found 42% of his series of UNE patients had low amplitude SNAPs recorded from the hand.8 Eisen (criteria met 4/6) found 32% of his patients with mild, and 79% with severe, UNE had absent distal sensory potentials.29 Miller (criteria met 3/6) found abnormal or absent distal SNAPs in 14 of 15 cases of cubital tunnel syndrome.61 None of these investigators attempted more proximal recording. Brown and Yates found 5 absent and 1 low amplitude digital SNAP in 13 UNEs.13 Odusote and Eisen (criteria met 5/6) recorded NAPs AE in control subjects and patients with mild UNE, and found the most significant abnormality lay in dispersion of the NAP; no CVs were calculated.70
In a study (criteria met 4/6) of UNE in rheumatoid arthritis, surface antidromic sensory studies in 56 control ulnar nerves (elbow flexed 35º, no temperature control, latency to the peak, across elbow distance 10-14 cm) showed a BE-to-W SNCV of 59.4+5.6 m/s, and an AE-to-BE SNCV of 61.1+7.6 m/s.6
Forearm Muscle Recordings in Patients with Ulnar Neuropathy at the Elbow
Results of investigations recording from forearm flexor muscles are presented in Table 7.
Payan (criteria met 6/6) found motor latency to the FCU was prolonged in 3 UNE cases in which transsulcal studies were normal. Thirty-five cases were localized by motor studies, 25 because of transsulcal slowing and a further 10 because of increased latency to the FCU.74
Felsenthal and colleagues (normal reference study, criteria met 5/6) studied amplitudes, latencies and CVs to the FCU and flexor digitorum profundus using surface stimulation and recording in 48 control nerves.33 Their data is summarized in the table. Benecke and Conrad (criteria met 3/6) reported a normal latency of 3.12+0.3 ms to the FCU (surface stimulation 2 cm above medial epicondyle, concentric needle electrode recording 10 cm distal to medial epicondyle, no mention of elbow position or temperature).7 Wilbourn found recording from the FCU “singularly unhelpful.”100 Others have found FCU studies useful when M-waves were absent from distal muscles.94
Overall CV can clearly remain in the normal range over the commonly used distances of 10-12 cm when the abnormal segments are very short in relation to the total span of nerve studied. The probability of detecting abnormally slow conduction depends on the length of the most abnormal segment, the degree of slowing across it, and the length of normal nerve included in the measurement.13
Short-Segment Incremental Studies
Attempts to localize conduction abnormalities in UNE using segments as short as 2 cm were first made many years ago.46 Brown and colleagues demonstrated the feasibility of conduction studies over segments as short as 0.5 cm intraoperatively, and showed the most abnormal, and sometimes only abnormal, segment could be as short as 5 to 10 mm.12 Kimura demonstrated the feasibility of percutaneous short-segment studies for the median nerve.49 Brown and Yates later confirmed the concept and extended it to the ulnar nerve at the elbow.13
Miller awoke the neurologic community to the HUA (the cubital tunnel) as a compression site.61 He introduced “an inching technique...(moving) the stimulator along the nerve in several steps...to detect the site at which an abrupt change occurred in the amplitude (or configuration) of the CMAP.” This inching technique did not include measurement of latency changes over consecutive segments, or precise measurement of segment lengths. For purposes of this discussion, Miller’s technique is referred to as conventional inching to distinguish it from short-segment incremental studies (SSIS) which entail latency determinations over precisely measured 1- or 2-cm segments.
Working percutaneously, Brown and Yates (criteria met 5/6) found the maximum CV could be very abnormal and substantial conduction block present in a relatively short segment of nerve.13 Major conduction abnormalities were sometimes distributed over distances less than one fifth of the total distance over which conduction is routinely measured. No obvious relationship existed between the location of the primary conduction abnormality and the clinical history or examination in most patients.
Kanakamedala and colleagues (criteria met 4/6) stimulated the ulnar nerve at 2-cm intervals from 6 cm proximal to 4 cm distal to the medial epicondyle in 13 patients with suspected UNE and 20 normal control subjects, maintaining the elbow at 90º with a plastic splint.47 Two patients had trivial M-wave amplitude reductions but markedly increased conduction times over a discrete segment, 9 had both a latency change and an amplitude reduction across the same segment, 1 patient demonstrated only an abnormal latency change, and 1 only an amplitude change. In 8 patients, abnormalities were confined to a single 2-cm segment, in 4 the abnormalities spanned 2 segments and in 1 patient, 3 segments.
Campbell and colleagues (criteria met 4/6) compared localization by Miller’s conventional inching technique to localization by SSIS in 35 patients who underwent ulnar nerve exploration.17 Results of percutaneous studies were compared with findings of intraoperative electroneurography. Conventional inching studies disclosed a localizing abnormality in 19% and SSIS in 81% of cases. SSIS and intraoperative electroneurography findings correlated highly, but not perfectly. Of 33 patients undergoing primary ulnar exploration, 11 had HUA compression, but in 3 of these the HUA lay directly behind the medial epicondyle in a far proximal location and the clinical and electrodiagnostic findings simulated ordinary retroepicondylar compression. Studies confined to a search for conduction block or differential slowing may be limited by the low incidence of conduction block in chronic UNE.
From the available data the normal maximal latency change is in the range of 0.4249 to 0.4320 ms over a 1-cm segment, and 0.63 over a 2-cm segment,47 and the normal maximal Mwave amplitude reduction is in the range of 5%-6% over 1-2 cm.13,47 Felsenthal and Teng reported a maximal normal amplitude change of 1.07% per cm.34 Kimura found no abrupt changes in NAP or M-wave amplitude on inching studies around the elbow in any UNE patient.48
In the two studies which convincingly address the issue using percutaneous techniques, there is notable concordance in the incidence of retroepicondylar abnormalities (69% versus 62%), humeroulnar arcade abnormalities (23% versus 28%) and changes in both locations (8% versus 10%).17,47
Pickett and Coleman (criteria met 6/6) found needle EMG detected about two thirds of the ulnar nerve lesions, localizing the lesion to or above the elbow in one fifth. Fibrillations were seen in the FDI in 32% of the patients, the ADM in 15% and the FCU in 7%. Reduced interference pattern was seen in 58%, 55%, and 20%, and some needle examination abnormality was seen in 65%, 55%, and 22%, respectively.77 Kimura (criteria met 6/6) saw evidence of denervation in the ADM muscle in 50% of extremities, the FDI in 53.3%, the flexor digitorum profundus in 20% and the FCU in 6.7%. Needle examination abnormalities were most frequent in patients with absent SNAPs.48
Needle Electromyography Results
Bhala (criteria met 5/6) found abnormal insertional or spontaneous activity in 43.6% of his 78 patients overall, and 77.5% of the patients with a MNCV <45.0 m/s across the 35º flexed elbow. The FDI was the most commonly affected muscle (28%), followed by the ADM (23%) and the FCU (23%).8 Stewart (criteria met 5/6) found fibrillations in the FDI in 84%, the ADM in 52%, the FCU in 16%, and the flexor digitorum profundus in 16% of the UNEs in his series. Motor unit abnormalities were not used as a criterion for denervation.87
Eisen (criteria met 4/6) found needle EMG of little value in patients with mild UNE. In his patients with severe UNE, neurogenic MUP abnormalities and fibrillations were present in the FDI in 50%, the ADM in 37%, and the FCU in 6%. FCU MUP abnormalities were present in 27%.29
The frequent sparing of forearm flexors in UNE appears related to the severity of the neuropathy, to the level of compression, to redundant innervation via several branchlets and to the differential susceptibility of fascicles to injury not to the level of origin of the branch innervating the FCU.15
The conservative and operative management of patients with UNE are complex issues, which are beyond the scope of this discussion. Payan has editorialized on the concerns of many electrodiagnostic medicine consultants in discussing surgery and its complications.75 The subject of treatment is addressed in some of the references.14,25-27,30,32,35,56,57,64,66,72-74,90,101
Management of Ulnar Neuropathy at the Elbow
The following conclusions and recommendations are made for the electrodiagnostic medicine evaluation of patients with suspected UNE.These recommendations are practice guidelines unless otherwise indicated.
Conclusions and Recommendations
General principles:
1. Ulnar sensory and motor NCSs should be performed with surface stimulation and recording. Limb temperatures should be monitored and maintained in a reference range and should be reported if outside a reference range. Corrections in conduction for temperature, if any, should be indicated in the report, although warming cool limbs and repeating the studies is preferable when possible. This recommendation is a practice standard. 2. If ulnar sensory or motor NCSs are abnormal, further NCSs should be carried out to exclude a diffuse process. This recommendation is a practice standard.
Elbow position:
3. Ulnar motor NCS reports should specify the elbow position used during the performance of the studies and the reference values employed. The technique used should be the same as that used to determine the reference values. The same elbow position should be employed during both stimulation and measurement. This recommendation is a practice standard. 4. The most logical elbow position for ulnar NCSs is moderate flexion; 70º to 90º from horizontal.Moderate flexion provides the greatest correlation between surface skin measurement and true nerve length. 5. Across-elbow distances used in evaluations performed with the elbow in moderate flexion have been in the range of 10 cm; this distance correlates best with published reference values. However, studies performed over this distance may mask a focal abnormality. Normal results over a 10-cm distance may occur despite a significant focal lesion. 6. Stimulation more than 3 cm distal to the medial epicondyle should be avoided as the nerve is usually deep within the flexor carpi ulnaris muscle by this point and there is substantial risk of submaximal stimulation.
Technique:
7. When using moderate-elbow flexion, a 10-cm acrosselbow distance, and surface stimulation and recording, the following suggest a focal lesion involving the ulnar nerve at the elbow: Multiple internally consistent abnormalities are more convincing than isolated abnormalities, which raise the possibility of artifact or technical mishap. (Note: The following are listed in order of strength of evidence):
a. Absolute MNCV from AE to BE of less than 50 m/s. b. An AE-to-BE segment greater than 10 m/s slower than the BE-to-W segment. The literature is inadequate to make a recommendation regarding the percent of slowing. c. A decrease in CMAP negative peak amplitude from BE to AE greater than 20%; this suggests conduction block or temporal dispersion indicative of focal demyelination. This presumes that anomalies of innervation, i.e., Martin-Gruber anastomosis, are not present. d. A significant change in CMAP configuration at the AE site compared to the BE site. This presumes that anomalies of innervation, i.e., Martin-Gruber anastomosis, are not present. e. NAP recording may aid in diagnosis, especially in patients with only sensory symptoms. However, NAP studies have significant pitfalls and limitations. Before relying on changes in NAP amplitude or CV as a diagnostic criterion for UNE, the examiner should be fully aware of the content and technical details of the applicable literature. Abnormalities of the distal sensory or mixed NAP, especially loss of amplitude, are nonspecific and nonlocalizing features of UNE. f. The literature is not adequate to make a recommendation regarding conduction through the AE-to-W or BE-to-W segments. 8. If ulnar motor conduction studies with stimulation at the wrist, above and below the elbow recording from the abductor digiti quinti are inconclusive, the following procedures may be of benefit:
a. NCSs recorded from the FDI muscle. Because of differential fascicular involvement, fibers to the FDI may show abnormalities not evident when recording from the abductor digiti minimi. b. An inching study, exploring for changes in the CMAP amplitude, area or configuration, or for abnormal changes in latency over precisely measured 1- or 2-cm increments from AE to BE. The most convincing abnormality involves both a change in latency and a change in either amplitude, area, or configuration; however, latency changes in isolation may be significant. c. With severe UNE, distal wallerian degeneration may slow the BE-to-W segment secondarily and make localization difficult. Comparison of the AEto-BE segment with the axilla-to-AE segment may be useful under such circumstances, but normative data is scant. This recommendation is a practice option. d. NCSs to forearm flexor muscles are not generally useful, but may be employed as a last resort with awareness of the technical limitations and the applicable literature. This recommendation is a practice option. e. Depending on the results of NCSs, needle electromyography (EMG) may be indicated.Needle examination should always include the FDI muscle, which is the most frequent muscle to demonstrate abnormalities in UNE, and ulnar innervated forearm flexor muscles. Neither changes limited to the FDI, nor sparing of the forearm muscles, exclude an elbow lesion. If ulnar innervated muscles are abnormal, the examination should be extended to include nonulnar C8/medial cord/lower trunk muscles, to exclude brachial plexopathy, and the cervical paraspinals, to exclude radiculopathy. Interface with AAEM Guidelines
This literature review cites published studies that support the recommendations in the AAEM Guidelines in
Electrodiagnostic Medicine for patients undergoing electrodiagnostic evaluation for symptoms suggestive of UNE.2 The Guidelines recommend the following: motor conduction studies which include the distal motor latency, CMAP amplitude at wrist, below medial epicondyle and above medial epicondyle, CV from below medial epicondyle to W, above medial epicondyle to W and above medial epicondyle to below medial epicondyle, all employing the same technique used in obtaining the reference values; distal sensory studies assessing the peak or onset latency over some fixed distance for which reference values are available, or calculating the sensory CV. The Guidelines state that NAP studies across the elbow are of uncertain value, that needle examination should be sufficient to exclude brachial plexopathy or cervical radiculopathy, and that inching or SSIS studies can sometimes help resolve difficult cases.
Summary of Harms, Benefits and Costs for Interventions Considered
The risks of electrodiagnostic medicine evaluation to the patient include transient discomfort, bruise, hematoma, and infection from the needle insertion required to perform needle EMG, and the transient discomfort of the electric shocks to perform the NCSs. The risk of the electrodiagnostic medicine evaluation to the consultant includes inadvertent needle puncture of the consultant by the needle used to evaluate the patient and infection by hepatitis, human immunodeficiency virus (HIV), or other communicable disease.
This study has not undertaken a systematic evaluation of the benefits, harms and costs of NCSs and needle EMG in the evaluation of patients suspected of UNE. Such an evaluation would require an outcome study; our review of the literature did not identify such a study.
It is recommended that:
Recommendations for Future Research
1. Future evaluations of electrodiagnostic studies in UNE patients be constructed to:
a. Meet all six literature classification criteria described in this report. b. Report the specific clinical criteria used for the diagnosis of UNE. c. Include calculation of the sensitivity and specificity of the test results. d. Include sufficient data to permit comparison to the results of previously published studies. 2. An outcome study be performed to assess the harm, benefit, and cost of performing NCSs and needle EMG in patients with symptoms suggestive of UNE. The value of electrodiagnostic stuides in predicting treatment outcomes, including surgery, deserve future study. 3. The AAEM reviews this report every 5 years and updates the report as necessary. Ethical/Legal Considerations
In view of the convincing evidence of the sensitivity and specificity of NCSs and needle EMG to confirm the diagnosis of UNE, the AAEM concludes that healthcare providers and insurers have an obligation to accept NCSs and needle EMG, performed as described in this review, as valid and reproducible techniques for the evaluation of patients suspected of UNE.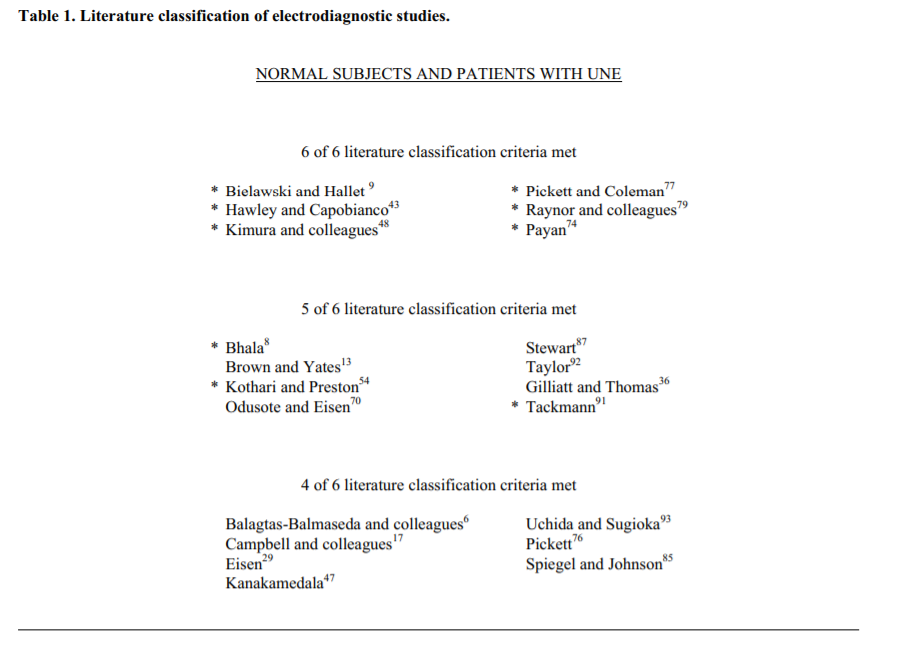
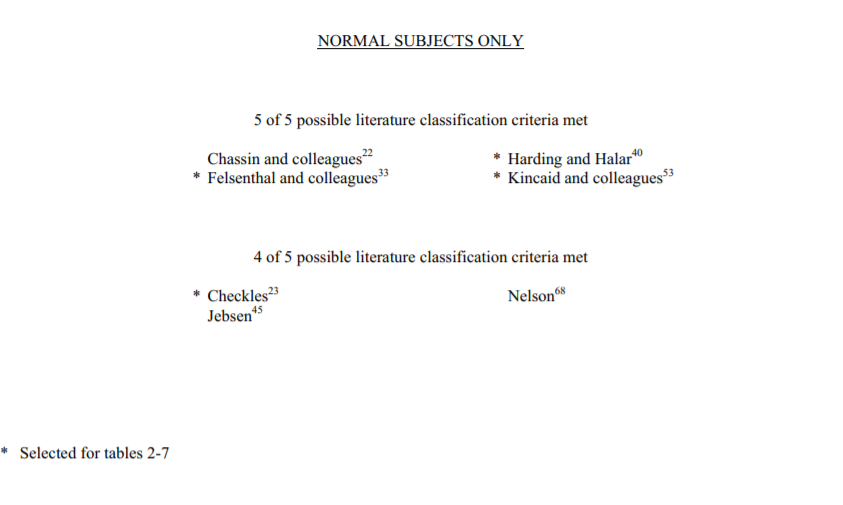
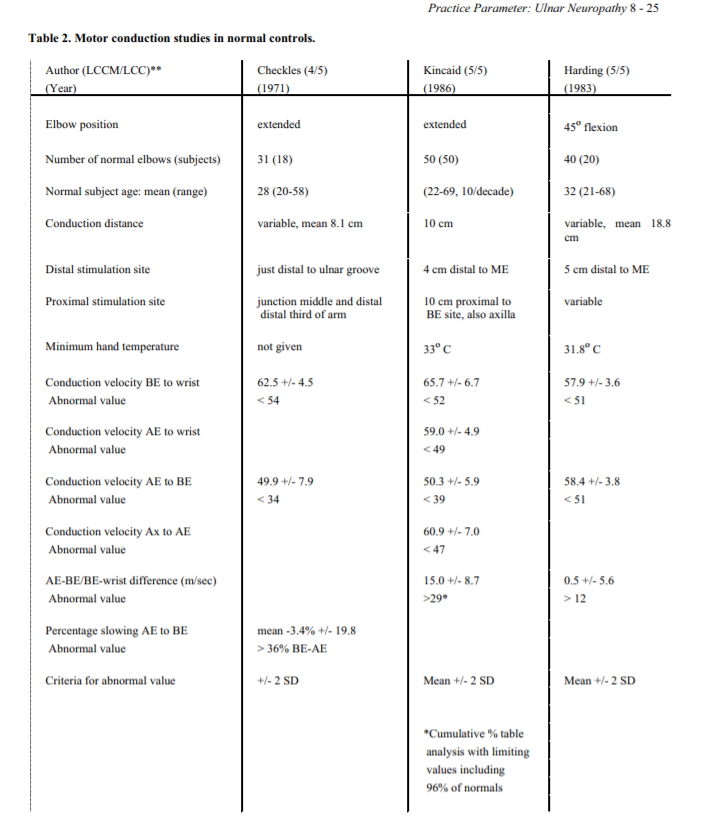
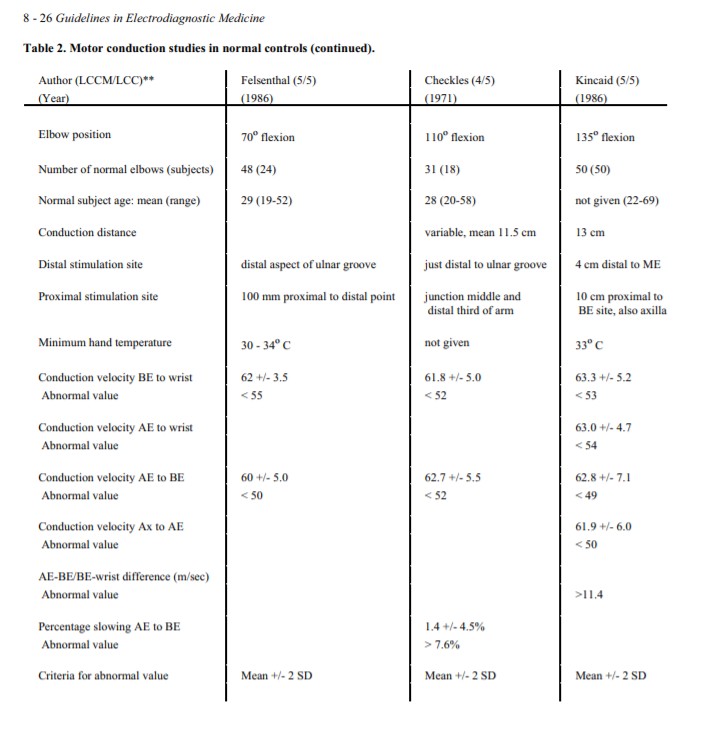
**Number of literature classification criteria met (LCCM)/total number of literature classification criteria (LCC).
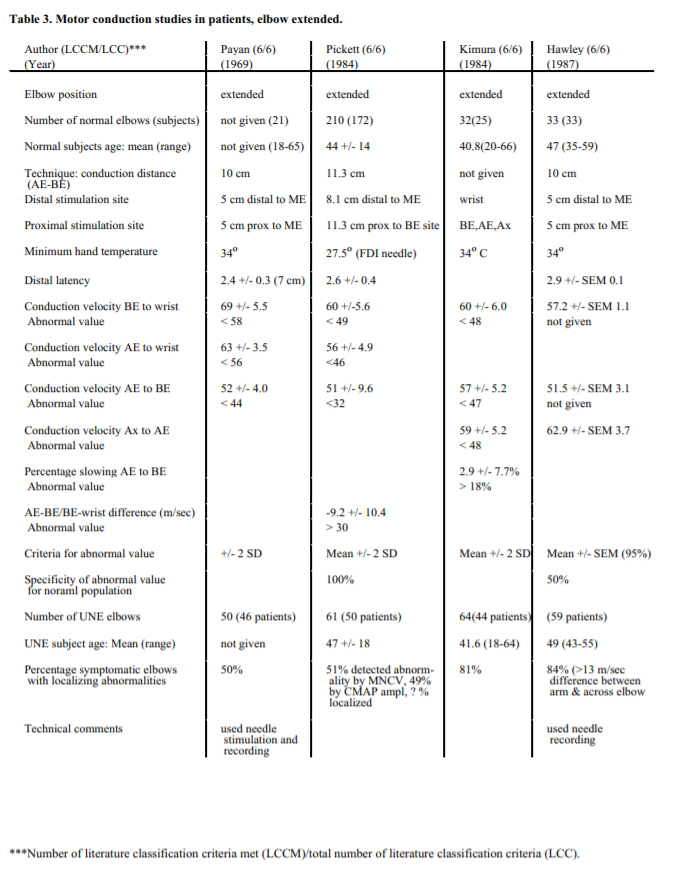
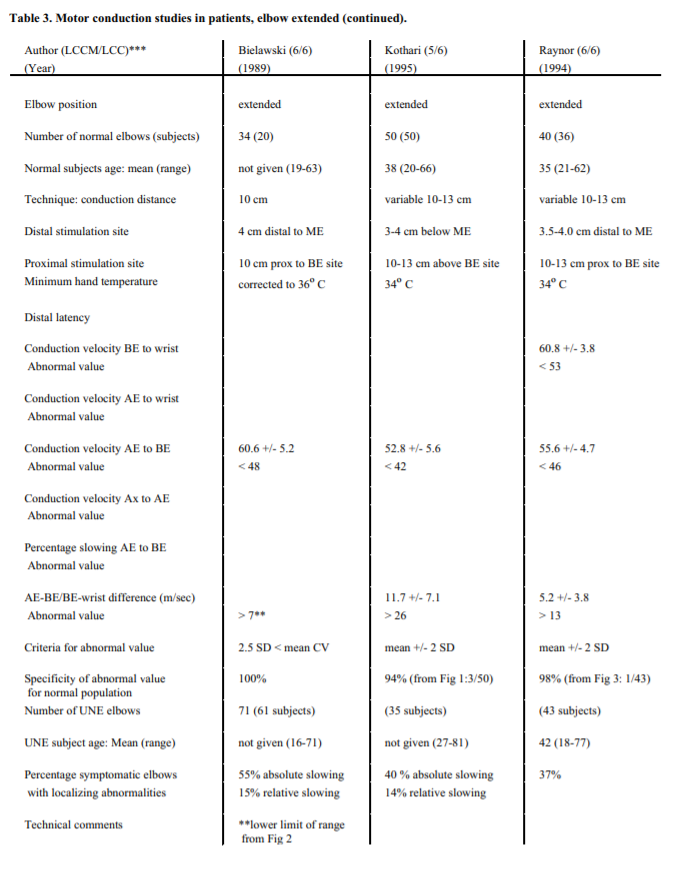
***Number of literature classification criteria met (LCCM)/total number of literature classification criteria (LCC).
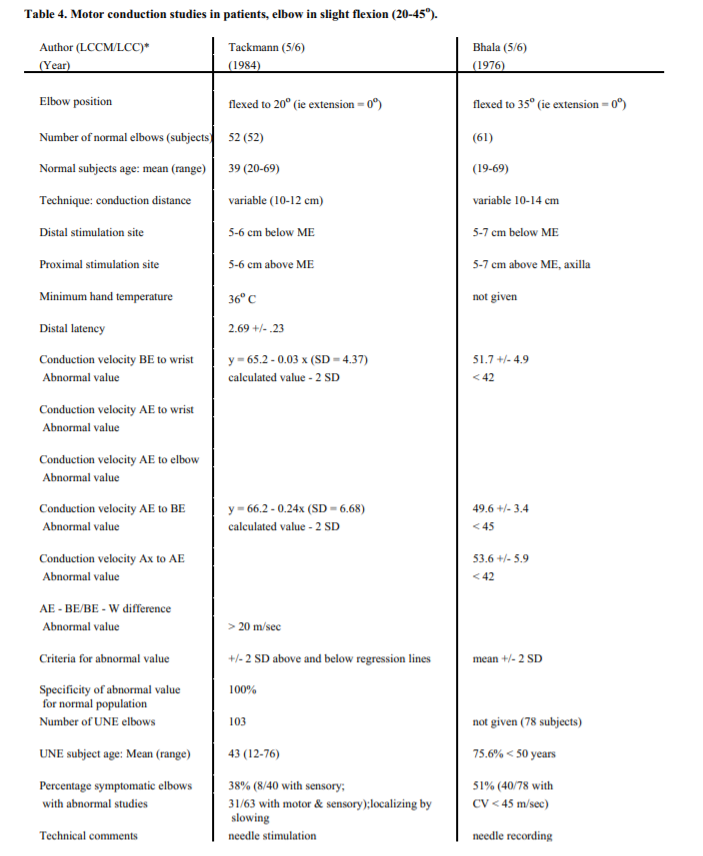
**Number of literature classification criteria met (LCCM)/total number of literature classification criteria (LCC).
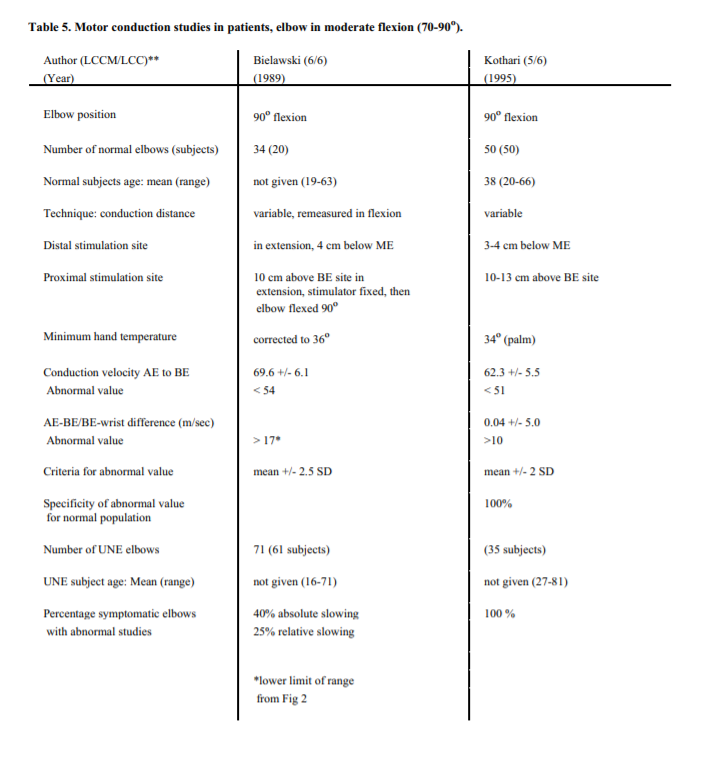
**Number of literature classification criteria met (LCCM)/total number of literature classification criteria (LCC).
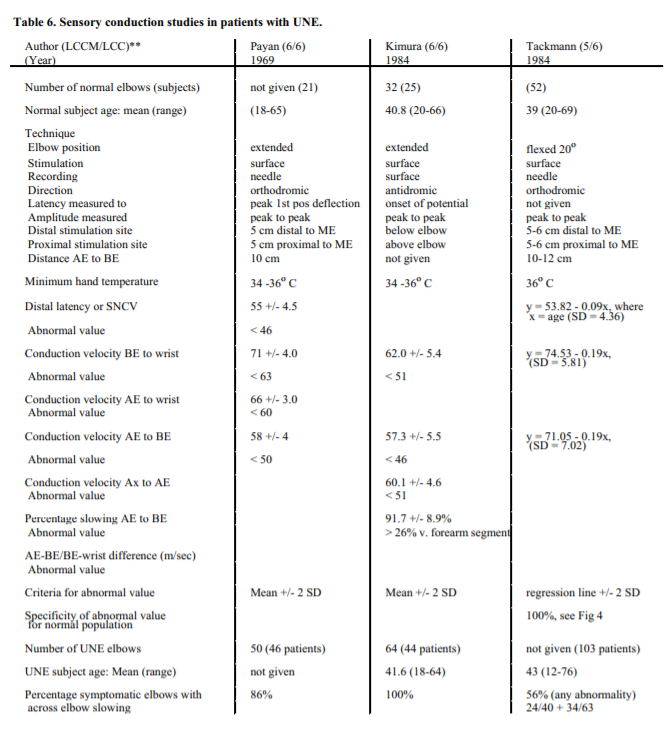
**Number of literature classification criteria met (LCCM)/total number of literature classification criteria (LCC).
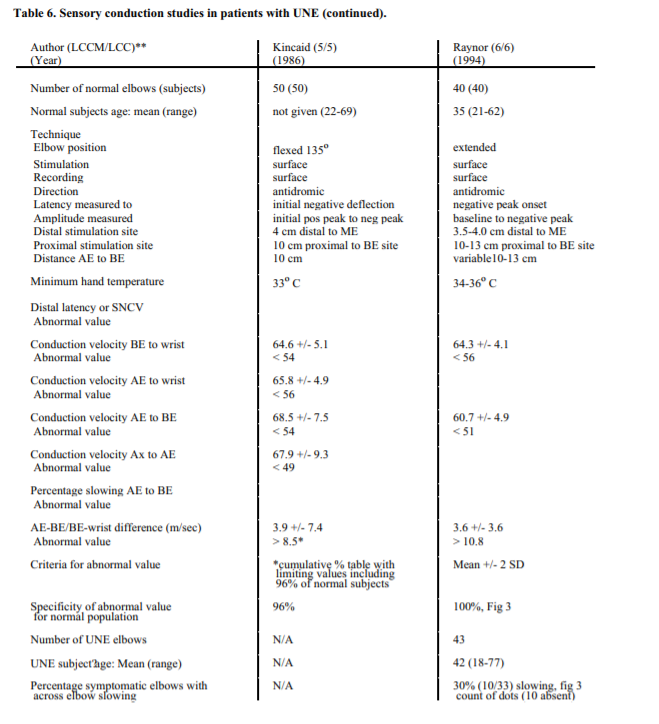
**Number of literature classification criteria met (LCCM)/total number of literature classification criteria (LCC).
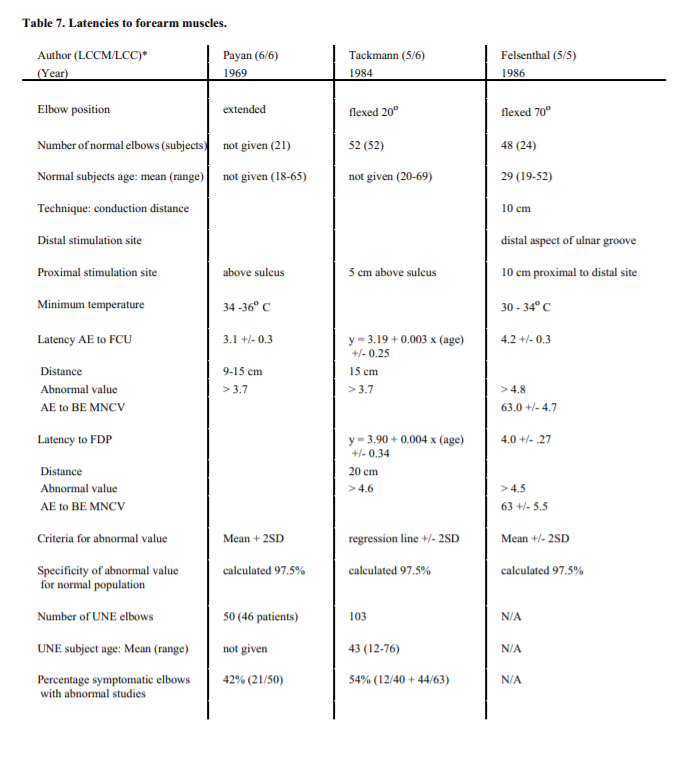
*Number of literature classification criteria met (LCCM)/total number of literature classification criteria (LCC).
References
| 1. | Amadio PC, Beckenbaugh RD. Entrapment of the ulnar nerve by the deep flexor-pronator aponeurosis. J Hand Surg Am 1986;11:83-87. Background reference. Source: AAEM consultant. | |
| 2. | American Association of Electrodiagnostic Medicine. Guidelines in electrodiagnostic medicine. Muscle Nerve 1993;16:1390-1414. Background reference. Source: AAEM consultant. | |
| 3. | Amoiridis G. Median-ulnar nerve communications and anomalous innervation of the intrinsic hand muscles: An electrophysiological study. Muscle Nerve 1992;15:576-579.Background reference. Source:Medline search. | |
| 4. | Anonymous. Electrodiagnosis of ulnar neuropathies. Lancet 1987;67:25-26. Background reference. Source: Medline search. | |
| 5. | Apfelberg DB, Larson SJ. Dynamic anatomy of the ulnar nerve at the elbow. Plast Reconstr Surg 1973;51:76-81. Background reference. Source: AAEM consultant. | |
| 6. | Balagtas-Balmaseda OM, Grabois M, Balmaseda PF, Lidsky MD:Cubital tunnel syndrome in rheumatoid arthritis. Arch Phys Med Rehab 1983;64:163-166. Criteria met (4/6: 1,3,5,6). Source: Medline search. Abstract:There has been an increase in reported cases of peripheral neuropathy and nerve entrapment syndromes in rheumatoid arthritis. (RA). To date, only a few incomplete studies on the prevalence of cubital tunnel syndrome (CuTS) in patients with RA have been reported. We investigated the prevalence of electrodiagnostic findings of CuTS in patients with RA and correlated them with the clinical findings. Forty-nine patients with the diagnosis of classic RA were evaluated clinically and by electrodiagnostic studies performed on the ulnar nerve, bilaterally, across the elbow. The study found 1 patient with slowing of both sensory and motor nerve CV (NCV), 8 patients with slowing of sensory NCV only, and 1 patient with slowing of motor NCV only. However, the correlation was poor between clinical and electrodiagnostic findings. | |
| 7. | Benecke R, Conrad B. The value of electrophysiological examination of the flexor carpi ulnaris muscle in the diagnosis of ulnar nerve lesions at the elbow. J Neurol 1980;223:207-217. Background reference. Source: Kincaid, 1988. | |
| 8. | Bhala R. Electrodiagnosis of ulnar nerve lesions at the elbow. Arch Phys Med Rehabil 1976;57:206-212. Criteria met (5/6: 1,2,3,5,6). Source: Kincaid, 1988. Abstract: To determine electrical criteria which might be helpful in the diagnosis of ulnar nerve entrapment at the elbow, clinical and electrodiagnostic features in 78 patients with suspected ulnar nerve entrapment at the elbow are described and compared to the results of sensory and motor conduction in the ulnar nerve in a control group of normal persons. These criteria include (1) absent or abnormal evoked sensory nerve action potential in the little finger, (2) motor CV of less than 45.0 m/sec in across elbow segment of the ulnar nerve with elbow flexed at 35 degrees, and (3) abnormal electromyographic findings including the presence of increased insertional activity or signs of denervation in the FDI, ADM, and /or FCU muscles. Electromyographic abnormality was seen in 77.5% of patients with ulnar motor CV of less than 45.0 meters/sec across the elbow. The first dorsal interosseous was the most commonly affected muscle. A study of certain important anatomic and histologic factors, such as the arrangement and relative concentration of the motor and sensory fibers at certain key points in the course of the ulnar nerve trunk, is necessary to understand the correlation between the clinicopathologic and electrodiagnostic features in patients with ulnar nerve entrapment at the elbow. | |
| 9. | Bielawski M, Hallett M. Position of the elbow in determination of abnormal motor conduction of the ulnar nerve across the elbow. Muscle Nerve 1989;12:803-809. Criteria met 6/6. Source: Medline search. Abstract:Routine evaluation of patients for suspected ulnar neuropathy includes testing of motor CV across the elbow, although the best position of the elbow for this test is controversial. The preferred testing position--elbow flexion or extension--was studied by determining the yield of abnormality at both positions in patients selected for possible ulnar nerve abnormalities on criteria unrelated to motor conduction. There were no major differences between the flexed or extended position of the elbow except that normal values for each of these positions varied. The yield of abnormal findings was greatest from measuring absolute motor CV across the elbow as opposed to comparing the difference in velocities between the elbow and either adjacent segment. | |
| 10. | Brown WF. The Physiological and Technical Basis of Electromyography. Boston: Butterworths; 1984. Background reference. Source: AAEM consultant. | |
| 11. | Brown WF, Dellon AL, Campbell WW. Electrodiagnosis in the management of focal neuropathies: The “WOG” syndrome. Muscle Nerve 1994;17:1336-1342. Background reference. Source: Medline search. | |
| 12. | Brown WF, Ferguson GG, Jones MW, Yates SK. The location of conduction abnormalities in human entrapment neuropathies. Can J Neurol Sci 1976;3:111-122. Background reference. Source: Brown, 1982. Abstract:Direct stimulation of 23 median, 13 ulnar, and 2 peroneal nerves at the time of surgical exploration has been used to locate and characterize the conduction abnormalities in the nerves. The most frequent location of the major conduction abnormalities in the median nerve was in the first 1-2 cm distal to the origin of the carpal tunnel. In the ulnar nerve the important conduction abnormalities were located most frequently in the segments 1 cm proximal and distal to the medial epicondyle. In the peroneal nerve the major conduction abnormalities occurred proximal or distal to the entry point of the common peroneal nerve into the peroneus longus muscle. | |
| 13. | Brown WF, Yates SK. Percutaneous localization of conduction abnormalities in human entrapment neuropathies. Can J Neurol Sci 1982;9:391-400. Criteria met (5/6: 1,2,3,5,6). Source:Kincaid, 1988. Abstract:In entrapment neuropathies the characteristic abnormalities in conduction are frequently limited to a short segment of the nerve. Recognition and precise localization of these discrete conduction abnormalities may require measurement of conduction over shorter lengths of the nerves than those lengths commonly employed in the clinical laboratory. Techniques are described for the more precise location of the primary conduction abnormalities in median, ulnar and peroneal nerve entrapments. Distinctive or atypical locations of the major conduction abnormalities may point towards different mechanisms in the pathogenesis of these localized neuropathies. | |
| 14. | Campbell WW. Ulnar neuropathy at the elbow: Anatomy, causes, rational management and surgical strategies, in 1991 AAEM Course D: Focal Peripheral Neuropathies: Selected Topics. Rochester, MN, American Association of Electrodiagnostic Medicine, 1991, pp 7-12. Background reference. Source: AAEM consultant. | |
| 15. | Campbell WW, Pridgeon RM, Riaz G, Astruc J, Leahy M, Crostic EG. Sparing of the flexor carpi ulnaris in ulnar neuropathy at the elbow [see comments]. Muscle Nerve 1989;12:965-967. Criteria met (1/6: 6). Source: Medline search. | |
| 16. | Campbell WW, Pridgeon RM, Riaz G, Astruc J, Sahni KS.Variations in anatomy of the ulnar nerve at the cubital tunnel: Pitfalls in the diagnosis of ulnar neuropathy at the elbow. Muscle Nerve 1991;14:733-738. Background reference. Source: Medline search. | |
| 17. | Campbell WW, Pridgeon RM, Sahni KS. Short-segment incremental studies in the evaluation of ulnar neuropathy at the elbow. Muscle Nerve 1992;15:1050-1054. Criteria met (4/6: 1,3,5,6). Source: Medline search. Abstract: Conventional electrodiagnosis may localize an ulnar neuropathy to the general region of the elbow. Separating retroepicondylar compression from compression by the humeroulnar aponeurotic arcade from compression by the deep flexorpronator aponeurosis is more difficult. In 35 patients, we compared localization by conventional inching (stimulating stepwise around the elbow searching for focal conduction block or differential slowing) to localization by a more quantitative short-segment incremental stimulation (SSIS) technique assessing latency change over consecutive 1 cm segments. Results of percutaneous studies were compared with findings of intraoperative electroneurography. We conclude that SSIS identifies compression levels more accurately than conventional inching, and that SSIS and intraoperative electroneurography correlate highly, but not perfectly. Studies confined to a search for conduction block or differential slowing are limited by the low incidence of conduction block in chronic compression neuropathies. | |
| 18. | Campbell WW, Pridgeon RM, Sahni SK. Entrapment neuropathy of the ulnar nerve at its point of exit from the flexor carpi ulnaris muscle. Muscle Nerve 1988;11:467-470. Criteria met (2/6: 2,3). Source: Medline search. | |
| 19. | Campbell WW, Robinson LR. Deriving reference values in electrodiagnostic medicine. Muscle Nerve 1993;16:424-428. Background reference. Source:Medline search.Abstract:Traditional methods for determining nerve conduction reference values have usually involved studying a group of normal controls, and determining the mean + 2 standard deviations (SD) for each parameter. Recent studies suggest other factors should be taken into account. Height has a greater effect on CV than age or temperature. The common assumption that conduction values follow a normal, bell shaped Gaussian distribution appears unwarranted. The curve for some conduction parameters is significantly skewed, making a mean + 2 SD definition of normality inaccurate to a clinically important degree. In developing and using reference values one should consider height, age, and temperature, and calculate the mean + 2 SD of the transformed data to remove the effects of skew. Reference values provide only a guide to the probability a given result came from a healthy or diseased individual; one should therefore seek multiple internally consistent abnormalities before diagnosing disease on the basis of electroneurography. | |
| 20. | Campbell WW, Sahni SK, Pridgeon RM, Riaz G, Leshner RT. Intraoperative electroneurography: Management of ulnar neuropathy at the elbow. Muscle Nerve 1988;11:75-81. Background reference. Source: Kincaid, 1988. | |
| 21. | Carpendale MT. The localization of ulnar nerve compression in the hand and arm: An improved method of electroneuromyography. Arch Phys Med Rehabil 1966;47:325-330. Criteria met (3/6: 1,2,4). Source: Kincaid, 1988. | |
| 22. | Chassin S, Little J, DeLisa J. Compound nerve action potentials from the median and ulnar nerves. Arch Phys Med Rehabil 1987;68:31-358. Criteria Met (5/6: 1,3,4,5,6). Source: Medline search. Abstract:The compound nerve action potentials from mixed motor/sensory (MNAP) and sensory (SNAP) nerve stimulation in the median and ulnar nerves were recorded in both arms of 20 able-bodied subjects. Intranerve and internerve peak-to-peak amplitudes were compared. An SNAP/MNAP amplitude ratio greater than 0.25 exceeded the mean by 2SD. The fastest, intermediate, and slowest conduction velocities were calculated from chosen points on the biphasic waveform. An intermediate MNAP CV for the median and ulnar nerves of less than 49.5 m/sec was more than 2SD below the mean. Likewise, an intermediate SNAP CV of less than 45.5 m/sec exceeded 2SD below the mean. Median MNAP latency across the carpal tunnel was 1.0 +/- 0.3 and ulnar MNAP CV across the elbow was 59.7 +/- 3.8 m/sec. This technique may supplement traditional electrodiagnostic studies in evaluating upper extremity neuropathies. | |
| 23. | Checkles NS, Russakov AD, Piero DL. Ulnar nerve conduction velocity - effect of elbow position on measurement. Arch Phys Med Rehabil 1971;53:362-365. Criteria met (4/6: 1,3,5,6). Source: Bielawski, 1989. Abstract: Studies of the rate of ulnar nerve conduction, across-elbow segment and forearm segment, were done on 18 normal persons in 2 positions, full extension and flexion at an acute angle. The ulnar nerve was stimulated 8 cm. proximal to the motor point of the ADQ, a point distal to the ulnar groove, and a point proximal to the ulnar groove. Comparisons of the amplitude and duration of the action potential after stimulation at 3 points were made. The duration and amplitude of the evoked potentials were not affected by elbow position. Conduction velocities were highest across the elbow segment when the elbow was flexed, probably due to change in the distance. When compared with the forearm segment, the velocity of the segment across the elbow was 1.5% faster when the elbow was flexed, and 20% slower when the elbow was extended. The variation of the across-elbow velocity with the elbow extended was much greater than that with the elbow flexed. From studying the ulnar nerve in situ in a cadaver arm, we found the true length of the ulnar nerve across the elbow segment was more accurately measured with the elbow flexed. We conclude the precision would be enhanced if ulnar nerve conduction studies were carried out with the elbow in the 70 degree flexed position (110º as defined in this paper). | |
| 24. | Cornblath DR, Sumner AJ, Daube J, Gilliatt RW, Brown WF, Parry GJ, Albers JW, Miller RG, Patajan J. Conduction block in clinical practice. Muscle Nerve 1991;14:869-871. Background reference. Source: AAEM consultant. | |
| 25. | DeJesus PV, Steiner JC. Spontaneous recovery of ulnar neuropathy at the elbow. Electromyogr Clin Neurophysiol 1976;16:239-248. Background reference. Source: AAEM consultant. | |
| 26. | Dellon AL, Hament W, Gittelshon A. Nonoperative management of cubital tunnel syndrome: An 8-year prospective study. Neurology 1993;43:1673-1677. Background reference. Source: Medline search. | |
| 27. | Dellon AL, Mackinnon SE. Surgery of the Peripheral Nerve. New York: Thieme Med Publishers; 1988. p 217-273. Background reference. Source: AAEM consultant. | |
| 28. | Duinslaeger L, DeBacker A, Ceulemans L, Wylock P. Ulnar nerve injury with Martin-Gruber Anastomosis. Eur J Plast Surg 1987;10:37-39. Background reference. Source: Medline search. | |
| 29. | Eisen A. Early diagnosis of ulnar nerve palsy. Neurology 1974;24:256-262. Criteria Met (4/6: 1,2,3,5). Kincaid, 1988. Abstract: Simple, quick electrophysiologic tests make it possible to diagnose the early cubital tunnel syndrome. Electrophysiologic investigation demonstrated dysfunction of the ulnar nerve due to a lesion localized to the elbow in (1) 60% of 56 patients with a presumptive diagnosis of cubital tunnel syndrome but no confirmatory clinical signs, (2) 25% of 48 control subjects, and (3) 91% of 34 patients with clear cut clinical evidence of an ulnar nerve compression at the elbow. The terminal motor latency from above the elbow to the abductor digiti quinti minimi muscle was of the most value in diagnosing early cubital tunnel syndrome. If this latency is greater than 9 msec, the diagnosis of the syndrome should be seriously considered. | |
| 30. | Eisen A, Danon J. The mild cubital tunnel syndrome. Neurology 1974;24:608-613. Background reference. Source: Kincaid, 1988. | |
| 31. | Farquhar Buzzard E. Some varieties of toxic and traumatic ulnar neuritis. Lancet 1922;1:317-319. Background reference. Source: AAEM consultant. | |
| 32. | Feindel W, Stratford J. The role of the cubital tunnel in tardy ulnar palsy. Can J Surg 1958;1:287-300. Background reference. Source:Kincaid, 1988. | |
| 33. | Felsenthal G, Brockman PS, Mondell DL, Hilton EB. Proximal forearm ulnar nerve conduction techniques. Arch Phys Med Rehab 1986;67:440-444. Criteria met (5/6: 1,3,4,5,6). Source: Medline search. Abstract: Compression of the ulnar nerve across the elbow is a common clinical diagnosis frequently referred for electrodiagnostic evaluation. Motor conduction studies with recording over the abductor digiti minimi and stimulating proximal and distal to the ulnar notch have been the standard technique employed in these evaluations--mean, 60.0 m/s; SD 5.0 m/s. Two other techniques are described, with data from normal subjects, recording from proximal forearm muscles. One technique is a refinement of a previously described method recording from the flexor carpi ulnaris--mean, 63.0 m/s; SD, 4.7 m/s. The second is a newly developed technique recording from the flexor digitorum profundus- -mean, 63.0 m/s; SD, 5.5 m/s. All three methods were found to have a small range of comparable normal values, and appear to be easily and quickly performed with reliable and reproducible information.The techniques described enhance specific localization of ulnar nerve lesions, and may prove useful when more distal recording sites are unavailable. | |
| 34. | Felsenthal G, Teng CS. Changes in duration and amplitude of the evoked muscle action potential (EMAP) over distance in peroneal, median, and ulnar nerves. Amer J Phys Med 1983;62:123-134. Criteria met (3/6: 1,3,6). Source: Medline search. | |
| 35. | Foster RJ, Edshage S. Factors related to the outcome of surgically managed compressive ulnar neuropathy at the elbow level. J Hand Surg 1981;6:181-192. Background reference. Source: AAEM consultant. | |
| 36. | Gilliatt RW, Thomas PK. Changes in nerve conduction with ulnar lesions at the elbow. J Neurol Neurosurg Psychiat 1960;23:312-320. Background reference. Criteria met (5/6: 1-3,5,6). Source: Stewart, 1987. | |
| 37. | Golovchinsky V. Ulnar-to-median anastomosis and its role in the diagnosis of lesions of the median nerve at the elbow and wrist. Electromyogr Clin Neurophysiol 1990;30:31-34. Background reference. Source: Medline search. | |
| 38. | Grundberg AB. Ulnar tunnel syndrome. J Hand Surg 1984;9:72-74. Background reference. Source: Medline search. | |
| 39. | Gutmann L. AAEM Minimonograph #2: Important anomalous innervations of the extremities. Muscle Nerve 1993;16:339-347. Background reference. Source: Medline search. Abstract: Anomalous innervations of the extremities are common and influence the interpretation of electrophysiologic studies in normal patients and those with peripheral nerve lesions. The following anomalous innervations are reviewed: median to ulnar nerve communication; ulnar to median nerve communication; variations in the innervation of intrinsic muscles of the hand; accessory deep peroneal nerve; and tibial to peroneal nerve communication. The electrophysiologic recognition of these anomalies and the manner in which they affect the interpretation of electrodiagnostic studies in various conditions is emphasized. | |
| 40. | Harding C, Halar E. Motor and sensory ulnar nerve conduction velocities: Effect of elbow position. Arch Phys Med Rehab 1983;64:227-232. Criteria met (5/6:1,3,4,5,6).Source:Kincaid, 1988. Abstract:Ulnar motor and sensory nerve conduction velocities (NCV) were studied bilaterally in 20 able-bodied subjects for below elbow (BE) and across elbow (AE) segments to assess the effect of 4 different elbow positions on NCV (0 degrees, 45 degrees, 90 degrees, and 135 degrees). Although constant skin stimulation marker points were used, the AE segment length became progressively longer with increased elbow flexion. At 0 degrees flexion the AE segment motor NCV was found to be slower, and at 45 degrees it was found faster than the BE NCV. At each subsequent elbow flexion position (90 degrees and 135 degrees) there was an erroneous increase in motor and sensory NCV for the AE segments (p less than 0.01). This increase in AE NCV with elbow flexion was mostly due to stretching of skin over the flexed elbow. The nerve itself was observed in 4 cadaver specimens to slide distally with respect to the above elbow skin marker. Since 45 degrees elbow flexion was the position of least variation in motor NCV for AE and BE segments, this degree of elbow flexion appears to be optimum. From these measurements and from literature review neither short AE segment length (less than 10 cm) nor long AE segment length (greater than 15 cm) is optimum for measurement of AE NCV in the assessment of compressive neuropathy at the elbow. Short segments are subject to increased NCV variation while long segments may not detect pathological slowing of NCV only occurring over a short portion of the nerve. | |
| 41. | Harmon RL. Bilaterality of ulnar neuropathy at the elbow. Electromyogr Clin Neurophysiol 1991;31:195-198. Criteria met (1/6: 3). Source: Medline search. | |
| 42. | Harrison MJG. Pressure palsy of the ulnar nerve with prolonged conduction block. J Neurol Neurosurg Psychiatry 1976;39:96-99. Background reference. Source: AAEM consultant. | |
| 43. | Hawley J, Capobianco J Localizing ulnar nerve lesions by motor nerve conduction study. Electromyogr Clin Neurophysiol 1987;27:385-392. Criteria met 6/6. Source: Medline search. Abstract:Individual patients with isolated ulnar neuropathy with damage at the elbow underwent slowing by a mean of 22.4 (4.7 SEM) in going from their brachium to their elbow segment. In a patient with no diffuse neuropathy, and only a possible ulnar nerve lesion at the elbow, a criterion is proposed that 13 m/sec slowing of the elbow segment below the brachial segment be considered a sign of an ulnar nerve lesion at the elbow. Individual patients with nondiabetic diffuse peripheral neuropathy with superimposed clinical ulnar neuropathy from damage at the elbow underwent slowing by a mean of 27.4 (4.4 SEM) m/sec in going from their brachium to their elbow segment. For patients with diffuse nondiabetic peripheral neuropathy a criterion is proposed that 18 m/sec slowing of the elbow segment below the brachial segment be considered a sign of an ulnar nerve lesion at the elbow. Because of slowing of CV throughout the ulnar nerve of patients with diabetic diffuse peripheral neuropathy, no criterion is proposed for these patients. | |
| 44. | Jablecki CK, Andary MT, So YT, Wilkins DE, Williams FH. Literature review of the usefulness of nerve conduction studies and electromyography for the evaluation of patients with carpal tunnel syndrome. Muscle Nerve 1993;16:1392-1414.Background reference. Source: AAEM consultant. Abstract:The sensitivity and specificity of nerve conduction studies (NCS’s) and electromyography (EMG) for the diagnosis of carpal tunnel syndrome (CTS) were evaluated by a critical review of the literature. With a search of the medical literature in English through May 1991, 165 articles were identified and reviewed on the basis of six criteria of scientific methodology. The findings of 11 articles that met all six criteria and the results of 48 additional studies that met four or five criteria are presented. We concluded that median sensory and motor NCS’s are valid and reproducible clinical laboratory studies that confirm a clinical diagnosis of CTS with a high degree of sensitivity and specificity. Clinical practice recommendations are made based on a comparison of the sensitivities of the several different median nerve conduction study (NCS) techniques. | |
| 45. | Jebsen RH. Motor conduction velocities in the median and ulnar nerves. Arch Phys Med Rehabil 1967;48:185-194. Criteria met (4/6: 1,3,5,6). Source: Kincaid, 1988. Abstract: Motor CV can be reliably determined over proximal segments of the median and ulnar nerves using Erb’s point as the proximal point of stimulation, and calipers for measurement of the proximal distance. Such determinations may be useful in the diagnosis of local proximal neuropathy and in generalized neuropathies in which a proximal-distal CV gradient may exist. | |
| 46. | Kaeser HE. Erregungsleitungsstorungen bei ulnarlsparesen. Dtsch Z Nervenheilkd 1963;185:231-243. Background reference. Source: Kincaid, 1986. | |
| 47. | Kanakamedala RV, Simons DG, Porter RW, Zucker RS. Ulnar nerve entrapment at the elbow localized by short segment stimulation. Arch Phys Med Rehab 1988;69:959-963. Criteria met (4/6: 1,3,5,6). Source: Medline search. Abstract:The purpose of the study was to evaluate the differences in the amplitudes of the compound muscle action potentials of the hypothenar muscles and the differences in conduction times. Differences in short segment responses were determined by stimulating the ulnar nerve at 2-cm intervals across the elbow in 20 normal adults. Thirteen ulnar nerves on the left side and 12 nerves on the right of 14 men and six women were studied for motor nerve CV. The amplitudes of the hypothenar compound muscle action potentials and the conduction times after supramaximal stimulation of the ulnar nerve were also determined. The distal-to-proximal reduction in the amplitude of the potentials was 6% on the left and 4.2% on the right. The maximum conduction time in a 2-cm segment on the right side was 0.63 msec (mean +2SD = 0.43 + 0.20) and on the left, 0.60msec (mean +2SD = 0.44 + 0.16). Using the same short segment stimulation technique, ulnar nerve motor conduction was also studied in 13 patients with suspected ulnar neuropathy at the elbow in order to localize the nerve lesion. Conduction time only was abnormal in one patient, both conduction time and amplitude in nine, amplitude only in one, and conduction time and mild reduction in amplitude in two. It was concluded that short segment stimulation of the ulnar nerve at the elbow is useful in localizing the exact site of entrapment/compression of the nerve at the elbow. | |
| 48. | Kimura I, Ayyar DR, Lippmann SM. Early electrodiagnosis of the ulnar entrapment neuropathy at the elbow. Tohoku J Exp Med 1984;142:165-172. Criteria met 6/6. Source: Medline search. Abstract:Reliable, easy electrodiagnostic tests make it possible to diagnose ulnar entrapment neuropathy at the elbow. Ulnar nerve was stimulated supramaximally at the wrist, below and above the elbow, and at the upper arm, and the sensory nerve action potential (SNAP) and compound muscle action potential (CMAP) were recorded. Sensory and motor nerve conduction velocities (SNCVs, MNCVs) were calculated in each segment. In 12 of 64 symptomatic extremities of 44 patients with a presumptive diagnosis of ulnar neuropathy at the elbow MNCVs of all segments were within normal limits and only SNCV across the elbow was significantly slowed (P<0.001). In 25 extremities, SNAP was not obtained. Evidence of denervation in the first dorsal interosseous and abductor digiti minimi muscles was detected in about 50% hands tested. This percentage was higher in the hands with absence of SNAP than those with presence of SNAPs. It would appear that measurement of SNCV across the elbow is a more sensitive parameter to detect abnormal conduction across the cubital tunnel in patients with ulnar neuropathy. | |
| 49. | Kimura J. The carpal tunnel syndrome: Localization of conduction abnormalities within the distal segment of the median nerve. Brain 1979;102:619-635. Background reference. Source:AAEM consultant. | |
| 50. | Kimura J. Principles and pitfalls of nerve conduction studies. Ann Neurol 1984;16:415-429. Background reference. Source: AAEM consultant. Abstract:Reviews fundamental principles and changing concepts of nerve stimulation techniques and discusses their proper application in the differential diagnosis of peripheral nerve disorders. NCS help delineate the extent and distribution of the neural lesion and distinguish two major categories of peripheral nerve disease: demyelination and axonal degeneration.Although the method is based on simple principles, pitfalls abound in practice. Variability in nerve conduction measurement may result from temperature change, variations among nerve segments, and the effects of age. Other sources of error include excessive spread of stimulation current, anomalous innervation, temporal dispersion, and inaccuracy of surface measurements. Unlike a bipolar derivation, which selectively records near-field potentials, a referential recording may give rise to stationary far-field peaks from a moving source. Overlooking this possibility can lead to an incorrect interpretation of findings. Conventional NCS deal primarily with measurements of the distal nerve segments in an extremity. More recent techniques are applicable to less accessible anatomical regions, as illustrated by the elicitation of the blink reflex, F wave and H reflex, and the use of the inching technique. Other methods used to assess special aspects of nerve conduction include the ischemic test and studies of slow-conducting fibers. | |
| 51. | Kimura J, Machida M, Ishida T, Yamada T, Rodnitzky RL, Kudo Y, Suzuki S. Relation between size of compound sensory or muscle action potentials, and length of nerve segment. Neurology 1986;36:647-652. Background reference. Source: Medline search. | |
| 52. | Kincaid JC. AAEE Minimonograph #31: The electrodiagnosis of ulnar neuropathy at the elbow. Muscle Nerve 1988;11:1005-1015. Background reference. Source: Medline search. | |
| 53. | Kincaid JC, Phillips LH, Daube JR. The evaluation of suspected ulnar neuropathy at the elbow. Normal conduction study values. Arch Neurol 1986;43:44-47. Criteria met (5/6: 1,3,4,5,6). Source:Medline search. Abstract:Local compression of the ulnar nerve occurs at several points, with the elbow region being the most common. Nerve conduction studies can be useful in identifying and localizing such lesions; however, the specifics of the technique, including normal values, have not been firmly established. We evaluated the effect of elbow position on segmental conduction velocities (CVs), the influence of elbow, nerve segment length on CV calculations, the change in compound action potential amplitude at sites along the nerve, and the use of performing segmental sensory CVs. Conductions done with the elbow flexed produced less segment-tosegment CV variation than those obtained with the elbow extended. The influence of using overlapping nerve segments compared with short adjacent ones for segmental CV comparison is discussed. | |
| 54. | Kothari MJ, Preston DC. Comparison of the flexed and extended elbow positions in localizing ulnar neuropathy at the elbow. Muscle Nerve 1995;18:336-340. Criteria met (5/6: 1,3,4,5,6). Source: Medline search. Abstract:This study compared the utility of flexed and extended elbow positions in demonstrating focal slowing at the elbow relative to the forearm segment in 35 patients with UNE, using 50 controls. Patients had definite electrophysiologic localization to the elbow by either conduction block or by focal slowing demonstrated in one of the two positions. Applying cutoff values from the control group, all 35 patients demonstrated focal slowing in flexion, whereas only 5 of the 35 did so in extension. They concluded the flexed position is more sensitive in localizing UNE. | |
| 55. | Krogness K. The cubital ratio method. Electromyogr Clin Neurophysiol 1978;18:213-216. Background reference. Source: Kincaid, 1988. | |
| 56. | LeRoux PD, Ensign TD, Burchiel KJ. Surgical decompression without transposition for ulnar neuropathy: Factors determining outcome. Neurosurg 1990;27:709-714. Background reference. Source:Medline search. | |
| 57. | Lugnegard H, Juhlin L, Nilsson BY. Ulnar neuropathy at the elbow treated with decompression. Scand J Plast Reconstr Surg 1982;16:195-200. Background reference. Source: LeRoux, 1990. | |
| 58. | Martinez A, Barrio M, Conde MCP, Gutierrez AM. Electrophysiological aspects of sensory CV in healthy adults: 1. CV from digit to palm, from palm to wrist, and across the elbow, as a function of age. J Neurol Neurosurg Psychiatry 1978;41:1092-1096. Criteria met (3/6: 4,5,6). Source: Harding, 1983. | |
| 59. | Maynard FM, Stolov WC. Experimental error in determination of nerve conduction velocity. Arch Phys Med Rehabil 1972;53:362-372. Background reference. Source: Kincaid, 1988. | |
| 60. | Melvin JL, Harris DH, Johnson EW. Sensory and motor conduction velocities in the ulnar and median nerves. Arch Phys Med Rehabil 1966; 47:511-519. Background reference. Criteria met (3/6: 1,5,6). Source: Sunderland, 1978. | |
| 61. | Miller RG. The cubital tunnel syndrome: Diagnosis and precise localization. Ann Neurol 1979;6:56-59. Background reference. Source: Kincaid, 1988. | |
| 62. | Miller RG. Ulnar nerve lesions. In: Brown WF, Bolton CF, editors.Clinical electromyography, 2nd edition. Boston: Butterworths; 1993. p 249-269. Background reference. Source: Medline search. | |
| 63. | Miller RG, Camp PE. Postoperative ulnar neuropathy. JAMA 1979;242:1636-1639. Background reference. Source: Kincaid, 1988. | |
| 64. | Miller RG, Hummell EE. The cubital tunnel syndrome: Treatment with simple decompression. Ann Neurol 1980;7:567-569. Criteria met (3/6: 1,2,3). Source: Campbell, 1988. | |
| 65. | Miller RG, Olney RK. Persistent conduction block in compression neuropathy. Muscle Nerve 1982;5:S154-S156.Background reference. Source: AAEM consultant. | |
| 66. | Nathan PA, Myers LD, Keniston RC, Meadows KD. Simple decompression of the ulnar nerve: An alternative to anterior transposition. J Hand Surg 1992;17:251-254. Background reference. Source: Medline search. | |
| 67. | Neary D, Ochoa J, Gilliatt RW. Sub-clinical entrapment neuropathy in man. J Neurol Sci 1975;24:283-298. Background reference. Source: AAEM consultant. | |
| 68. | Nelson RM. Effects of elbow position on motor conduction velocity of the ulnar nerve. Phys Ther 1980;60:780-783. Criteria met (4/6: 1,3,5,6). Source: Kincaid, 1988. Abstract:This study evaluated the ability of the ulnar nerve motor axons to conduct an evoked action potential at three elbow positions (0,90 and 120 degrees).The latency, amplitude and duration of the potential were used to evaluate the effect of elbow position in 50 normal men. The results indicate that latency of the response, negative phase amplitude and duration of the potential did not vary with the elbow position. Clinical implications for the performance of motor nerve conduction studies for the ulnar nerve are presented. Suggestions for arm position during the studies are included. | |
| 69. | Novak CB, Lee GW, Mackinnon SE, Lay L. Provocative testing for cubital tunnel syndrome. J Hand Surg 1994;19:817-820. Background reference. Source: Medline search. | |
| 70. | Odusote K, Eisen A. An electrophysiological quantitation of the cubital tunnel syndrome. Can J Neurol Sci 1979;6:403-410. Criteria met (5/6: 1,2,3,5,6). Source: Kincaid, 1988. Abstract:492 ulnar nerves were studied in 237 patients with cubital tunnel syndrome and 233 subjects without clinically apparent ulnar neuropathy. Terminal motor and sensory latencies, motor and sensory conduction velocities, sensory action potential amplitudes and dispersions, and needle electromyography were analyzed by a 0-10 rating - the EMG score. The patients were clinically graded from 1 (least severe) to 4 (most severe). The median EMG scores of these were 0.9/10 (N=70); 1.6/10 (N=46); 4.7/10 (N=46); and 7.1/10 (N=56), respectively. The median EMG score for the controls was 0.6/10 (N=239) and 14.7% had asymptomatic ulnar entrapments. This incidence reached 30% in controls who were 60 years or older. In 25 other controls, the above sulcus sensory action potential was analyzed. Its mean dispersion was 4.9 +/- 1.0 s(-3). This measurement was significantly prolonged in 84.6% of 13 studies in which the EMG score was 0/10. These patients had either sensory symptoms only or an additional mild sensory deficit. Comparison of the EMG score obtained with sequential studies would allow one to objectively evaluate improvement or deterioration of the clinical state, giving a rational means of determining the need for surgery. | |
| 71. | Olney RK, Miller RG. Conduction block in compression neuropathy: recognition and quantification. Muscle Nerve 1984;7:662-667. Background reference. Source: Medline search. | |
| 72. | Osborne GV. The surgical treatment of tardy ulnar neuritis. J Bone Joint Surg Am 1957;39B:782. Background reference. Source: Kincaid, 1988. | |
| 73. | Paine EW. Tardy ulnar palsy. Can J Surg 1970;13:255-261.Background reference. Source: Dellon, 1988. | |
| 74. | Payan J. Electrophysiological localization of ulnar nerve lesions. J Neurol Neurosurg Psychiatry 1969;32:208-220. Criteria met (6/6). Source: Kincaid, 1988. Abstract: Ulnar sensory potentials were recorded with near nerve needle electrodes at the wrist, 5 cm distal and 5 cm proximal to the medial epicondyle stimulating with surface electrodes on the small finger, averaging 500-1000 responses and measuring the latency to the peak of the first positive deflection, amplitude peak to peak and assessing duration and shape. The electrodes used for sensory recording were then used to stimulate the nerve while recording with a concentric needle electrode in both the hypothenar muscles and first dorsal interosseous, measuring onset latency and peak to peak amplitude. 36 lesions were studied by needle EMG of ulnar hand but not forearm muscles. Results are presented separately for normals 18-65 years old vs. 70-89 years old.Slowing of SNCV BE to wrist was seen in 83% of the cases and slowing across the sulcus in 86%. Prolongation of DSL occurred in 67% and DML in 40%. 75% had MNCV slowing in the forearm. 85% had trans-sulcal slowing using both hand muscles, 75% using only one. Motor latency to the FCU was prolonged in 3 cases in which trans-sulcal studies were normal. 34 of the 50 cases localized to the elbow by sensory studies, 30 because of trans-sulcal slowing and 4 because of “change in the sensory action potential.” 35 cases localized by motor studies, 25 because of trans-sulcal slowing and a further 10 because of increased latency to the FCU. In 23 cases, either sensory or motor parameters localized the lesion, and in 2 cases electrophysiological investigation failed to indicate the site of the lesion. Discussion of needle EMG findings is scant. Although 85% of cases showed trans-sulcal MNCV slowing, only 50% localized to the elbow because of the high incidence of forearm slowing. In 4 cases with MNCV or SNCV slowing, the lesion was localized to the elbow by changes in the shape of the sensory potential across the sulcus. In all, 48 of the 50 lesions could be localized by electrophysiological means, using all available methodology. | |
| 75. | Payan J. An electromyographer’s view of the ulnar nerve. J Bone Joint Surg Br 1986;68:13-15. Background reference. Source: Medline search. | |
| 76. | Pickett JB. The use of regression equations in the localization of ulnar and peroneal nerve lesions. Electromyogr Clin Neurophysiol 1984;24:361-368. Criteria met (4/6: 1,4,5,6). Source:Medline search. | |
| 77. | Pickett JB, Coleman LL. Localizing ulnar nerve lesions to the elbow by motor conduction studies. Electromyogr Clin Neurophysiol 1984;24:343-360. Criteria met 6/6. Source: Medline search. Abstract:Ulnar motor amplitude and CV were studied in 172 normal patients (210 nerves) and 50 patients with 61 ulnar nerve lesions. The efficiency of a test, or proportion of times the test results were true, was used to find the optimal way to separate the normal and nerve lesion groups. Ulnar motor and sensory conduction studies and electromyography of ulnar innervated muscles was abnormal in 87% of the ulnar nerve lesion group. The best way to localize an ulnar nerve lesion to the elbow was a drop in motor amplitude >25% across the elbow. | |
| 78. | Pridgeon RM, Campbell WW. Evaluating focal neuropathies: the long and short of it. Muscle Nerve 1991;14:881-882. (Abstract only). Background reference. Source: AAEM consultant. | |
| 79. | Raynor EM, Shefner JM, Preston DC, Logigian EL. Sensory and mixed nerve conduction studies in the evaluation of ulnar neuropathy at the elbow. Muscle Nerve 1994;17:785-792. Criteria met 6/6. Source: Medline search. Abstract:The relative sensitivities of sensory, mixed nerve, and motor conduction studies in assessing ulnar neuropathy at the elbow have not yet been established. Using surface electrodes, conduction studies were performed across the elbow segment in 43 patients with symptoms referable to the ulnar nerve and 40 control subjects. Segmental slowing of motor conduction localized the lesion to the elbow in 14 or 21 patients (67%) with clear evidence of ulnar neuropathy on physical examination but only in 2 of 22 (9%) with subtle or no physical examination abnormalities. The diagnostic yield was increased by the finding of segmental slowing of sensory or mixed nerve conduction across the elbow to 86% and 68% respectively, for each of the groups. We conclude that surface-recorded sensory and mixed nerve conduction studies appear to be more sensitive than motor studies in the electrodiagnosis of ulnar neuropathy at the elbow and are especially valuable in patients with subtle clinical involvement. | |
| 80. | Robinson LR, Temkin NR, Fujimoto WY, Stolov WC. Effect of statistical methodology on normal limits in nerve conduction studies. Muscle Nerve 1991;14:1084-1090. Background reference. Source: AAEM consultant. Abstract:Mean +/- 2SD, which relies on a Gaussian distribution, has traditionally been used to derive normal limits for NCS. We examined skew in NCS 22 parameters, and compared normal limits derived by several alternative methods in 75 controls. The coefficient of skewness (g1) was significantly positive for 5 of 8 amplitude and 6 of 8 latency measurements. Transformation reduced g1 in 19 of 22 parameters. For each measurement, ideal normal limits were defined as mean + 2SD of the optimally transformed control data. The percentage of 66 diabetics classified as abnormal by the raw data, but normal by the ideal normal limits, was the positive misclassification rate; while the reverse was the negative misclassification rate. Mean +/- 2SD of the raw data produced 11% positive and 12% negative misclassifications.Defining normal limits by the range or 97.5% confidence limits also yielded significant misclassification rates. We conclude that analyses using the raw data to derive normal limits result in an unacceptable rate of misclassification. Normal limits should be derived from the mean +/2SD of the optimally transformed data. | |
| 81. | Rosenfalck P, Rosenfalck A. “Electromyography - Sensory and Motor Conduction - Findings in Normal Subjects.” Rigshospitalet, Copenhagen, Laboratory of Clinical Neurophysiology, 1975 (UnPub). Background reference. Source: Tackmann, 1984. | |
| 82. | Schubert HA. Conduction velocities along course of ulnar nerve. J Appl Physiol 1964;19:423-426. Background reference. Source: Kincaid, 1986. | |
| 83. | Seror P. Tinel’s sign in the diagnosis of carpal tunnel syndrome. J Hand Surg 1987;12-B:364-365. Background reference. Source: Jablecki, 1993. | |
| 84. | Simpson JA. Electrical signs in the diagnosis of carpal tunnel and related syndromes. J Neurol Neurosurg Psychiatry 1956;19:275-280. Background reference. Source: Jablecki, 1993. | |
| 85. | Spiegel MH, Johnson EW. Conduction velocity in the proximal and distal segments of the motor fibers of the ulnar nerve of human beings. Arch Phys Med Rehabil 1962;43:57-61. Background reference. Criteria met (4/6: 1,3-5). Source:Harding, 1983.Abstract: Measurement of CV of motor nerves was done on 38 ulnar nerves of 21 subjects, to determine the relation between the velocity in the proximal and the distal segments of motor fibers to the ADM muscle. The results indicate that the velocity in the distal segments is slightly greater than that in the proximal segments. While these differences are statistically significant, we do not feel that they are of clinical importance in electrodiagnosis. The small differences may be explained by mechanical sources of error in the technique or perhaps by unknown factors. When the isolation of a muscle response is necessary, as in stimulating motor nerves when several are in close proximity, a needle electrode is helpful. | |
| 86. | St John JN, Palmaz JC. The cubital tunnel in ulnar entrapment neuropathy. Radiology 1986;158:119-123. Background reference. Source: Medline search. | |
| 87. | Stewart JD. The variable clinical manifestations of ulnar neuropathies at the elbow. J Neurol Neurosurg Psychiatry 1987;50:252-258. Criteria met (5/6: 1,2,3,5,6). Source: Medline search. Abstract: In twenty-five cases of ulnar neuropathy at the elbow, the involvement of the fibers from three sensory and to four motor branches were examined clinically and, where possible, electrophysiologically. Of the sensory fibers, those from the terminal digital nerves were most commonly involved. The fibers to the hand muscles were much more frequently involved than those to the forearm muscles.These findings suggest that in ulnar neuropathies at the elbow there is variable damage to the fascicles within the nerve. | |
| 88. | Streib EW. Ulnar-to-median anastomosis in the forearm: Electromyographic studies. Neurology 1979;29:1534-1537. Background reference. Source: Sun, 1983. | |
| 89. | Sun SF, Streib EW. Martin-Gruber anastomosis: Electromyographic studies, part II. Electromyogr Clin Neurophysiol 1983;23:271-285. Background reference. Source: Medline search. | |
| 90. | Sunderland S. Nerves and nerve injuries. Edinburgh: Churchill Livingstone; 1978. Background reference. Source:AAEM consultant. | |
| 91. | Tackmann W, Vogel P, Kaeser HE, Ettlin T. Sensitivity and localizing significance of motor and sensory electroneurographic parameters in the diagnosis of ulnar nerve lesions at the elbow. A reappraisal. J Neurol 1984; 231:204-211. Criteria met (5/6: 1,2,4,5,6). Source: Medline search. Abstract:A total of 103 patients (40 with pure sensory disturbances, 63 with sensory and motor deficits) with ulnar nerve lesions at the elbow were examined neurophysiologically. The measurement of motor CV across the cubital tunnel alone did not completely localize the lesion. The latency to an ulnar- innervated flexor muscle was of outstanding importance. The measurement of amplitudes was only rarely of localizing significance. The results of sensory recording proved to be important in patients with pure sensory disturbances. In cases with additional motor deficits, sensory recordings were too often abnormal in all segments of the ulnar nerve to be of substantial localizing value. | |
| 92. | Taylor PK. Non-linear effects of age on nerve conduction in adults. J Neurol Sci 1984;66:223-234. Criteria met 5/6 (1,3,4,5,6). Source: Medline search. Abstract:The effects of age on conduction and amplitude in median and ulnar (motor and sensory), superficial radial, sural and common peroneal (motor) nerves of adults were prospectively investigated. Four routinely recorded parameters, including CV, amplitude and duration, were considered for each sensory nerve and measurements of CV, terminal motor latency and amplitude were made for each motor nerve. The resulting 25 sets of data were analyzed using both linear and quadratic regression. The three sets of terminal motor latency data showed no age dependence while in six other instances there was a linear relationship with age (three of these being motor amplitude). The remaining 16 sets of data were statistically best represented by quadratic analysis. The shapes of the paraboli were remarkably similar, reaching a maximum (CV and amplitude) or minimum (duration) value in the fourth decade and thereafter declining or rising respectively at an accelerating rate. With only one exception, quadratic curves of the same parameter were shown to be parallel. Tables of normal data which make accurate adjustments for the aging effect can be constructed from this analysis for use in routine clinical investigation. | |
| 93. | Uchida Y, Sugioka Y. Electrodiagnosis of Martin-Gruber connection and its clinical importance in peripheral nerve surgery. J Hand Surg Am 1992;17:54-59. Background reference. Criteria met (4/6: 1,2,5,6). Source: Medline search. | |
| 94. | Uchida Y, Sugioka Y. The value of electrophysiological examination of the flexor carpi ulnaris muscle in the diagnosis of cubital tunnel syndrome. Electromyogr Clin Neurophysiol 1993;33:369-373. Background reference. Source: Medline search. Abstract:In the electrodiagnosis of cubital tunnel syndrome, the abductor digiti minimi (ADM) muscle is frequently used to evoke compound muscle action potentials (CMAP) in order to measure the motor nerve conduction velocity (MNCV) in the ulnar nerve. Slowing of the MNCV across the elbow is a major criteria in the electrodiagnosis of cubital tunnel syndrome. However, in advanced cases, slowing of the MNCV is also seen in the forearm segment, thus, localization of the nerve palsy is sometimes difficult. We evoked CMAP from the flexor carpi ulnaris (FCU) muscle to assess the value of electrophysiological examination of this muscle in the diagnosis of cubital tunnel syndrome. CMAP from the FCU muscle could be evoked in many cases when CMAP from the ADM muscle could not. Also, the motor terminal latency (MTL) of the FCU was prolonged in proportion to the slowing of the MNCV across the elbow. Therefore, electrophysiological examination of the FCU muscle is useful in the diagnosis of cubital tunnel syndrome, especially when intrinsic muscle atrophy is severe and the CMAP from these muscles cannot be evoked. | |
| 95. | van Dijk JG, van der Kamp W, van Hilten BJ, van Someren P. Influence of recording site on CMAP amplitude and on its variation over a length of nerve. Muscle Nerve 1994;17:1286-1292. Background reference. Source: AAEM consultant. | |
| 96. | Vanderpool DW, Chalmers J, Lamb DW. Peripheral compression lesions of the ulnar nerve. J Bone Joint Surg Am 1968;50B:729-803. Background reference. Source: Campbell, 1988. | |
| 97. | Watson BV, Merchant RN, Brown WF. Early postoperative ulnar neuropathies following coronary artery bypass surgery. Muscle Nerve 1992;15:701-705. Background reference. Source: Medline search. | |
| 98. | Werner CO, Ohlin P, Elmqvist D. Pressures recorded in ulnar neuropathy. Acta Orthop Scand 1985;56:404-406. Background reference. Source: Medline search. | |
| 99. | Wilbourn AJ. Electrodiagnosis with entrapment neuropathies. In: 1992 AAEM Plenary Session I: Entrapment neuropathies. Rochester, MN: American Association of Electrodiagnostic Medicine; 1992. p 23-37. Background reference. Source: AAEM consultant. | |
| 100. | Wilbourn AJ. Ulnar neuropathy at the elbow: Electrodiagnostic approaches. In: 1991 AAEM Course D: Focal peripheral neuropathies: Selected topics. Rochester, MN: American Association of Electrodiagnostic Medicine; 1991. p 13-17. Background reference. Source: AAEM consultant. | |
| 101. | Wilson DH, Krout R. Surgery of ulnar neuropathy at the elbow: 16 cases treated by decompression without transposition. J Neurosurg 1973;38:780-785. Background reference. Source: Campbell, 1988. |
Document History
This guideline is greater than 5 years old. Every five years, an interim literature search is performed and the guidelines reviewed. While new studies have been published since this guideline was last reviewed, the Practice Issue Review Panel Committee of the AANEM has determined that these studies are not sufficient to mandate a revision of the guideline at the present time. The information contained in this guideline and the recommendations offered are still relevant to the current practice.
Creation of New Guidelines, Consensus Statements, or Position Papers
AANEM members are encouraged to submit ideas for papers that can improve the understanding of the field. The AANEM will review nominated topics on the basis of the following criteria:- Members’ needs
- Prevalence of condition
- Health impact of condition for the individual and others
- Socioeconomic impact
- Extent of practice variation
- Quality of available evidence
- External constraints on practice
- Urgency for evaluation of new practice technology
