International Consensus Guidance for the Management of Glucocorticoid Related Complications in Neuromuscular Disease
1 | Introduction
Autoimmune neuromuscular disorders (NMD), such as myasthenia gravis (MG), chronic inflammatory demyelinating polyradiculoneuropathy (CIDP), and inflammatory myopathies, often require long-term immune suppression. Although new classes of immune therapies are being developed to treat these conditions, glucocorticoids (GC) remain first-line and subsequent treatments in many cases [1–3]. The ongoing use of GC stems from good clinical effectiveness, longstanding familiarity with their use, universal availability, and low cost.
The multitude of adverse reactions (ARs) from GC therapy is well-known to healthcare professionals and patients and can occur with short- and long-term use, limiting their tolerability in many patients. Some of the potential ARs may require ongoing monitoring or preventive prophylactic treatments [4]. Despite the ubiquitous use of GC to treat autoimmune NMD and the known risks of such treatment, there remains high variability in how neuromuscular specialists monitor for and manage potential complications of chronic GC, and no neurology specific guidelines exist [5]. In fact, even a universal definition of “chronic” or “high dose” GC therapy is lacking, further hampering standardization of the management of GC complications.
In a survey of neuromuscular neurologists conducted in Canada, over 90% of respondents expressed the desire for neurology specific guidelines for managing GC complications. Over one-third of those surveyed were not aware of published guidelines in other specialties related to the prevention of specific GC complications (e.g., prevention of osteoporosis) [5–7]. There is a small number of publications that synthesize some data surrounding the risks of GC treatment in NMD or attempt to provide an opinion regarding the management of specific risks, but no formal guidelines exist in the neurological or neuromuscular literature [8, 9]. The lack of evidence-based or consensus-based guidance on managing chronic GC complications is a quality gap that may contribute to nonstandardized care and possibly adverse outcomes for patients. This gap partly stems from a lack of high-quality evidence to inform practice, as one would receive from randomized controlled treatment trials or long-term prospective studies.
An interdisciplinary, international task force was established by the AANEM, consisting of experts from various fields. The goal of the AANEM task force was to develop consensus-based guidance to serve as a practical guide for neuromuscular clinicians in the prevention and management of many GC-induced complications and ARs. As with all such guidance documents, this guidance is not meant to be comprehensive or prescriptive, or to provide a single definitive algorithm, but rather to provide overall guidance which will be modified by local practice patterns and resource availability and will serve as a starting point for further research and future modification.
2 | Methods
2.1 | Topic Selection and Definitions
The task force co-chairs (RSL, CDK, CB) selected the following topics for investigation, considering their practical significance and the absence of existing consensus within neuromuscular practice concerning the use of GC: Pneumocystis jiroveci pneumonia (PJP) prophylaxis, vaccination, osteoporosis and bone health, ocular health, gastrointestinal prophylaxis, hypertension, and hyperglycemia. For the purposes of these guidelines, we have defined chronic GC treatment as >2.5mg/day prednisone equivalent for >3months. However, the duration of GC treatment to define chronic is not consistent in the literature as different specialties use different definitions or thresholds [6, 7, 10, 11]. For alternate-day dosing, the following example of equivalence has been used: 40mg prednisone every other day=20mg prednisone daily [12–15]. Here, dosing refers to the dose of prednisone, but the recommendation applies to the equivalent dose of other GC (whether oral or intravenous). The recommendations assume the use of systemic GC and do not apply to inhaled or topical formulations.
2.2 | Search Strategy
A comprehensive search of OVID Medline was performed to complete a scoping review for the relevant topics limited to articles published since 2010. Potential articles were selected with specified indexed words and keywords with the search terms applied to the title, abstract, and author-supplied keywords to ensure a comprehensive scoping review (Supporting Information, Appendix A).
2.3 | Article Selection
The initial search yielded a total of 1,531 studies. After removing 109 duplicate articles, 1,422 unique studies remained. Each abstract was independently screened by two reviewers to assess their potential relevance. The full-text articles of 284 abstracts were retrieved for evaluation by two independent reviewers. Disagreements were reconciled by a third reviewer. One hundred ninety studies were excluded for assorted reasons (Figure 1, and also see Supporting Information, Appendix A). In total, 94 articles were included in the development of the scoping review (Figure 1).
2.4 | Data Extraction
These studies were summarized by the two independent reviewers into a narrative review on each topic. The summaries included relevant study characteristics and key findings to address the topics of the consensus guidance.

2.5 | Task Force
The task force comprised five neuromuscular specialists and one of each of the following: general neurologist, neuroimmunology specialist, infectious disease specialist, endocrinologist, rheumatologist, gastroenterologist, ophthalmologist, and general internist. For each topic under investigation, relevant experts were selected to participate in the development of consensus statements, ensuring that the expertise aligned with the specific subject matter.
2.6 | Development of Consensus Statements
The task force co-chairs (CDK, CB, RSL) drafted initial statements based on the narrative review for each topic (Supporting Information, Appendix B). The RAND/UCLA appropriateness method (RAM) for formal consensus was employed to establish agreement on each statement. Before voting, all voting task members received the relevant narrative review. The voting process was conducted through anonymous email communication. The methodologist (PN) solely collected the voting materials for analysis and did not participate in the voting. Panel members rated statements on a 9-point scale, with scores ranging from 1 to 9 (1–3: inappropriate, 4–6: uncertain, and 7–9: appropriate). The median and range of ratings were calculated for each recommendation to evaluate the appropriateness and the level of agreement for each statement was determined based on the RAM process [16].
Based on the consensus and feedback from task force members, the co-chairs and methodologists revised the statements after each round for subsequent rounds of voting. Before the subsequent round, each voting member received the results of the voting, anonymous comments, and suggestions from other voters from the previous round. This process was repeated up to three rounds for each statement to achieve consensus as needed. Any recommendation that did not achieve consensus after three rounds of voting was excluded.
3 | Results
3.1 | General Consideration for GC Management
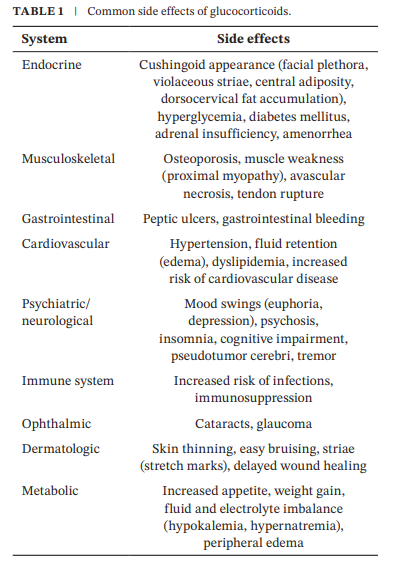
Chronic GC exposure has a multitude of systemic ARs with no universal agreement on the duration or dose of GC at which these AEs may occur [4, 17]. The most common side effects of GC are outlined in Table 1. There is no single “correct” GC tapering regimen, with multiple different regimens described in the literature, including alternate-day or every-day tapering, slower or more rapid methods, and the choice of taper may depend on the disease, disease activity, and comorbidities [13, 14, 18]. We did not evaluate or vote upon any specific GC tapering regimens in this guidance document.
3.1.1 | Consensus Recommendations for General Care and Screening During Chronic GC Therapy
- In patients receiving chronic GC therapy, a multidisciplinary approach involving the primary care clinician and relevant specialists should be established early to effectively monitor, prevent, and manage the general medical issues and potential adverse events associated with GC exposure (median 9, range 8–9).
- Patients starting chronic GC should be counseled on the common and serious side effects of GC therapy (median 9, range 9).
- Glycemic control should be checked before initiation of GC therapy and at regular intervals thereafter, in coordination with the primary care clinician, endocrinologist, or the multidisciplinary team (median 8, range 6–9).
- Blood pressure should be monitored and managed regularly for patients on GC therapy in coordination with the primary care clinician or multidisciplinary team (median 8, range 8–9).
- In patients on chronic GC who have risk factors for peptic ulcer disease (PUD), such as chronic or frequent NSAID use, pharmacologic therapy for PUD prophylaxis should be prescribed, unless there is a contraindication (median 8, range 8–9).
- Ophthalmological examination is recommended for patients on GC therapy for ≥6months, and annually thereafter, or in clinical situations where there is a concern for cataracts or glaucoma (median 8, range 5–9).
- To avoid GC treatment withdrawal, chronic glucocorticoid therapy should be tapered slowly, and not stopped abruptly (median 9, range 8–9).
3.2 | Bone Health
Multiple publications report best practice guidelines for the screening and prevention of GC-induced osteoporosis, particularly the American College of Rheumatology (ACR), with details of risk stratification and pharmacological treatment [6, 7, 19]. As with the other statements in this document, we aimed to develop statements that were within the scope of knowledge and practice of most neuromuscular specialists. For example, details of the tools for fracture risk stratification and pharmacologic agents for treatment or prevention of osteoporosis (other than calcium and Vitamin D supplementation) are outside the scope of neurologic practice. The most recent 2022 ACR guidelines for the prevention of GC-induced osteoporosis are a resource [6].
There is an increased risk of vertebral fracture with GC dosing as low as 2.5mg/day of prednisone, with the highest risk of bone loss being within the first 3 to 6months [7, 20, 21]. For simplicity and because daily GC doses in NMD are usually higher than 2.5mg, the task force statements recommend osteoporosis prevention strategies at any dose of GC used for greater than 3months. For patients in whom the likelihood of being on GC for over 3months is high (i.e., most NMD), these strategies should be implemented at the onset of GC therapy.
3.2.1 | Consensus Recommendations for Bone Health and GC-Induced Osteoporosis Prevention
- At the start of treatment and during active treatment with GC at any dose for >3months, screening for GC-induced osteoporosis should be recommended in coordination with the primary care clinician, and other appropriate specialists (e.g., endocrinology and rheumatology) (median 9, range 8–9).
- Preventative management of GC-induced osteoporosis should be instituted at any dose of glucocorticoid when used for >3months (median 9, range 6–9).
- Patients of any age who require chronic (≥3months) GC treatment should have a fracture risk assessment at baseline, in coordination with the primary care clinician or relevant specialist (e.g., endocrinologist and rheumatologist) (median 8, range 8–9).
- Lifestyle modifications should be recommended to all patients on any dose of GC for > 3 months. These include: a balanced diet, smoking cessation, limiting alcohol intake, and regular weight-bearing exercise (median 9, range 7–9).
- Vitamin D supplementation at 600–800 IU/day should be recommended to all patients on any dose of GC for >3months (median 9, range 3–9).
- Dietary or supplemental calcium intake of 1000–1200mg/ day should be recommended to all patients on any dose of GC for >3months unless there are contraindications (median 9, range 8–9).
- If necessary, input regarding the need for and choice of prescription pharmacologic treatment for GC-induced osteoporosis should be obtained from the primary care clinician and/or other appropriate specialists (e.g., endocrinology and rheumatology) (median 9, range 8–9).
3.3 | Vaccination Considerations
The following recommendations pertain to vaccination decisions beyond standard age-appropriate vaccinations. The U.S. Centers for Disease Control and Prevention (CDC) influences these guidelines, but local and regional regulations should be followed when available.
3.3.1 | Consensus Recommendations for Vaccinations During Chronic GC Therapy
- Vaccination before and during long-term GC therapy (≥2weeks) should be coordinated with the primary care clinician or by infectious disease consultation. Immunization recommendations for immunocompromised patients from local and regional agencies should be consulted and followed (median 9, range 5–9).
- Live attenuated vaccinations should not be given to patients being treated with GC at doses of ≥20mg/day (prednisone equivalent) for >2weeks (median 8, range 4–8).
- For patients who have been treated with GC at doses ≥20mg (prednisone equivalent) for >2weeks, live attenuated vaccines should be deferred for 1month after GC has been discontinued or 1month after the dose has been reduced below the 20mg threshold (median 8, range 6–8).
- In patients who are not on GC and require GC initiation (or re-initiation), treatment should be deferred for 4weeks after live attenuated vaccinations and 2weeks after inactivated vaccination, unless treatment with GC is emergently required (median 7, range 5–9).
- Herpes Zoster (HZ) vaccination should be recommended before starting GC therapy if possible. For those on >20mg of prednisone for >2weeks, the recombinant HZ vaccine should be used (median 8, range 5–9).
- Annual influenza vaccination (with inactivated vaccine) should be recommended to all patients on GC therapy unless there is a contraindication (median 9, range 8–9).
- Pneumococcal vaccinations should be recommended to adult patients 19−65 years of age and who are on>2weeks of GC therapy (median 8, range 6–9).
3.4 | Infectious Disease Prophylaxis
PJP is a fungal infection associated with immunocompromised individuals, including those receiving GC therapy [22, 23]. It is also important to consider prophylaxis for other conditions including tuberculosis (TB), human immunodeficiency virus (HIV), hepatitis, and strongyloides, based on geography and patient demographics. Recommendations for infection prophylaxis vary and there are no neurology specific recommendations [8–10, 24–26].
There remains controversy as to when it is appropriate to initiate PJP prophylaxis. Factors that are reported to increase the risk for PJP in patients on GC include lymphopenia, interstitial lung disease, active malignancy, organ dysfunction, and low CD4 count [8, 9, 22, 24, 27]. These risk factors should be taken into account when deciding whether to recommend prophylaxis. Initiation of PJP prophylaxis when chronic GC is used at a dose ≥20mg/day has been recommended in the infectious disease literature and is not specific to the underlying indication for GC treatment [10, 23, 24]. However, the risk for PJP infection appears to vary and generally is low in the neuromuscular patient population [8, 9, 25, 28]. Disease state, concomitant use of other immunosuppressive agents, or dose of GC may account for this variability [8, 25]. Therefore, individualized assessment is necessary when considering PJP prophylaxis for patients with NM disorders treated with GC.
3.4.1 | Consensus Recommendations for Infectious Disease Prophylaxis During Chronic GC Therapy
- PJP is a rare but serious complication of long-term GC therapy. The underlying disease itself likely influences the risk of PJP. The risk of PJP and the benefit of prophylaxis should be balanced with the adverse effects of prophylactic treatments. PJP prophylaxis should be used when the annual incidence of PJP for a given disease and treatment modality is ≥3.5%; however, there are limited data regarding the incidence of PJP in NMD (median 8, range 5–9).
- GC monotherapy: a. There are no published guidelines for PJP prophylaxis in individuals with NMD receiving GC or other immunosuppressive agents. If the annual incidence of PJP for a particular disease and treatment are not known, prophylaxis may be offered to patients receiving ≥20 mg/day of prednisone equivalent for ≥1 month (as monotherapy). Given the paucity of data, shared decision-making is important (median 7, range 2–9). Combination therapy of GC and additional GC sparing agent: b. There are no published guidelines for PJP prophylaxis in individuals with NMD receiving GC or other immunosuppressive agents. If the annual incidence of PJP for a particular disease and treatment are not known, prophylaxis should be offered for patients receiving ≥20mg of prednisone equivalent for ≥1month if a second immunosuppressive (IS) agent is added. Given the paucity of data, shared decision making is important (median 8, range 6–9).
- Trimethoprim-Sulfamethoxazole (TMP-SMX) one single strength tablet daily, or one double-strength tablet three times a week is the recommended regimen for PJP prophylaxis in patients with normal renal function, or adjusted for renal function (median 9, range 8–9).
- For patients with allergies to TMP-SMX, alternative options include desensitization or another antimicrobial (including atovaquone [1.5 g daily], dapsone [100mg daily], or aerosolized pentamidine [300mg monthly]) (median 8, range 3–9).
- Patients from endemic regions or those who have unexplained eosinophilia should be screened for Strongyloides stercoralis infection with serum IgG antibody levels to Strongyloides before initiation of GC therapy (median 8, range 7–9).
- Screening for latent tuberculosis (TB) is recommended for all patients who will receive ≥15mg prednisone equivalent for 2–4weeks or more and are at highest risk for reactivation of TB (those born in or frequently traveling to countries with high TB rates, or residents /employees of homeless shelters or correctional facilities) (median 8, range 7–9).
- Patients with a positive TB screen test should be referred for infectious disease consultation for treatment before GC is initiated (median 9, range 6–9).
- Hepatitis B screening is recommended in patients with NMD who will receive GC at a dose of ≥10mg prednisone equivalent for ≥4weeks (median 8, range 5–9).
- In situations in which GC needs to be started emergently or urgently, testing for hepatitis B and TB should be performed as soon as possible, and if abnormal, treatment should be instituted as early as possible with the involvement of the appropriate specialists (median 8, range 5–9).
- Screening for Hepatitis C is universally recommended by the US CDC for all people born between 1945 and 1965. There are insufficient data regarding hepatitis C screening in patients with NMD treated with GC. However, the risks of testing are low and testing may be offered to patients with NMD who will receive GC for 4weeks or more. Shared decision-making is important (median 8, range 6–9).
- Patients with positive hepatitis B/C screens should be referred for subspecialty consultation before starting chronic GC and should be comanaged for the duration of GC therapy (median 9, range 6–9).
- Screening for HIV may be offered for all patients with NMD who will receive GC at a dose of ≥20mg per day for ≥4weeks, and if positive, they should be referred to Infectious Disease before starting GC and should be comanaged for the duration of GC therapy. Shared decision-making is important given the paucity of data (median 8, range 7–9).
4 | Discussion
Glucocorticoids remain an effective treatment option for many autoimmune NMD, with a paucity of high-quality literature specific to the management of GC ARs in patients with NMD. This consensus guidance addresses the prevention and management of GC complications with a primary focus on NMD. In the process of developing the statements and voting to achieve consensus, the importance of a multidisciplinary approach became clear. The involvement of the primary care clinician and other relevant specialists is essential to the effective management of GC-related risk and ARs.
These recommendations are evidence-informed and consensus based; they are therefore subject to the conscious and unconscious biases of the panel members. We attempted to mitigate this by selecting panel members from different institutions and countries to have broad and varied input and by using an anonymous formal process for consensus. Although we have attempted to be comprehensive, because of the paucity of relevant evidence to inform strong recommendations, there are multiple areas and opportunities for future research and updates. For example, the value of checking vitamin D levels to determine fracture risk or need for supplementation remains unclear and controversial.
Although consensus was achieved, one of the more controversial areas was the statements related to PJP prophylaxis. More prospective data from clinical practice to inform decisions regarding the timing of PJP prophylaxis would help to inform future updates. Prospective work may also look to evaluate the practicality, usefulness and validity of these recommendations in clinical practice.
Author Contributions
C.B., P.N., R.S.L. and C.D.K. contributed to study conception, data collection, data analysis and manuscript preparation. M.B., F.B., D.D., E.P.F., C.G., J.K.M., R.G.M., S.M., P.K.T., P.S.S. contributed to data collection and manuscript preparation.
Acknowledgments
The panel would like to acknowledge Melanie Anderson, the information specialist and librarian, who assisted with the literature search. We would also like to acknowledge Dr. Bill David (Practice Issues Review Panel Chair) and Practice Issues Review Committee, who supported this project.
Ethics Statement
The authors confirm that they have read Muscle & Nerve's position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Conflicts of Interest
Dr. Bromberg reports being a medical consultant for Accordant Health, speaker's bureau for Argenx and Takeda, and author/royalties from UpToDate, Oxford University Press, and Cambridge University Press. Dr. Marshall has received honoraria received for consulting and/or speaking from AbbVie, Alimentiv, Amgen, Avir Pharma, Bausch Health, Bristol Myers Squibb, Celltrion, Ferring, Fresenius Kabi, Janssen, Lilly, Organon, Pfizer, Pharmascience, Regeneron, Roche, Sandoz, Sanofi, Takeda, Viatris. Dr. Buttgereit has received consulting fees from AbbVie, Grunenthal, and Horizon Therapeutics; has received grants from AbbVie, Biogen, Bristol Myers Squibb, Horizon Therapeutics, Lilly, Medac, Pfizer, and Sanofi; and has received honoraria from AbbVie, Medac, and Pfizer. Dr. Dodig has served on Advisory Boards and received consulting and/or research support from Sanofi, Alexion, Argenx, Alnylam, Akcea. Dr. Flanagan has served on advisory boards for Alexion, Genentech, Horizon Therapeutics and UCB. He has received research support from UCB. He received royalties from UpToDate. Dr. Flanagan is a site principal investigator in a randomized clinical trial of Rozanolixizumab for relapsing myelin oligodendrocyte glycoprotein antibody-associated disease run by UCB. Dr. Flanagan is a site principal investigator and a member of the steering committee for a clinical trial of satralizumab for relapsing myelin oligodendrocyte glycoprotein antibody-associated disease run by Roche/ Genentech. Dr. Flanagan is a co-investigator on a study of ravulizumab for neuromyelitis optica spectrum disorder run by Alexion. Dr. Flanagan has given educational talks on neuromyelitis optica spectrum disorder funded by Alexion. Dr. Flanagan has received funding from the NIH (R01NS113828). Dr. Flanagan has received honoraria for for editing and writing articles for The Continuum Lifelong Learning in Neurology Journal which is a publication of the American Academy of Neurology. Dr. Flanagan is a member of the medical advisory board of the MOG project. Dr. Flanagan is an editorial board member of Neurology, Neuroimmunology and Neuroinflammation, The Journal of the Neurological Sciences and Neuroimmunology Reports. A patent has been submitted on DACH1-IgG as a biomarker of paraneoplastic autoimmunity. Dr. Gottlieb reports no disclosures. Dr. McCoy has received support from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health (NIH), the National Institute on Aging (NIA) of the NIH, Patient Centered Outcomes Research Institute (PCORI), the National Center for Advancing Translational Sciences (NCATS), and the American Diabetes Association. She served as a consultant to EmmiEducate (Wolters Kluwer) and to Yale-New Haven Health System's Center For Outcomes Research and Evaluation. She has also received speaking honoraria and travel support from the American Diabetes Association. Dr. Mitchel has received salary support for the Brain Medicine Program from the Azrieli foundation. Dr. Tosh does not have any relevant disclosures. Dr. Sinha does not have any relevant disclosures. Dr. Laughlin does not have any relevant disclosures. Dr. Kassardjian has received speaker's honoraria from Argenx, Alexion, Sanofi, and Astra Zeneca, and participated in advisory boards for Argenx, Alexion, UCB, and Takeda.
Data Availability Statement
This consensus statement on the management of corticosteroid complications in neuromuscular disease is based on a review of existing literature and expert consensus. No new data were generated or analyzed for this work. All data referenced in this statement are publicly available through the cited sources.
Muscle & Nerve, 2025; 0:1–8 (accepted December 10, 2024)
References
- D. B. Sanders, G. I. Wolfe, M. Benatar, et al., “International Consensus Guidance for Management of Myasthenia Gravis: Executive Summary,” Neurology 87 (2016): 419–425, https://doi.org/10.1212/WNL.0000000000002790.
- P. Narayanaswami, D. B. Sanders, G. Wolfe, et al., “International Consensus Guidance for Management of Myasthenia Gravis: 2020 Update,” Neurology 96 (2021): 114–122, https://doi.org/10.1212/WNL.0000000000011124.
- P. Y. K. van den Bergh, P. A. van Doorn, R. D. M. Hadden, et al., “European Academy of Neurology/Peripheral Nerve Society Guideline on Diagnosis and Treatment of Chronic Inflammatory Demyelinating Polyradiculoneuropathy: Report of a Joint Task Force—Second Revision,” European Journal of Neurology 28 (2021): 3556–3583, https://doi.org/10.1111/ene.14959.
- S. L. Cartwright and M. S. Cartwright, “Health Maintenance for Adults With Neuromuscular Diseases on Immunosuppression: Health Maintenance,” Muscle & Nerve 59 (2019): 397–403, https://doi.org/10.1002/mus.26382.
- L. Stepanian, R. S. Laughlin, C. Bacher, et al., “Chronic Glucocorticoid Management in Neuromuscular Disease: A Survey of Neuromuscular Neurologists,” Muscle & Nerve 70 (2024): 52–59, https://doi.org/10.1002/mus.28069.
- M. B. Humphrey, L. Russell, M. I. Danila, et al., “2022 American College of Rheumatology Guideline for the Prevention and Treatment of Glucocorticoid-Induced Osteoporosis,” Arthritis Care and Research 75 (2023): 2405–2419, https://doi.org/10.1002/acr.25240.
- L. Buckley, G. Guyatt, H. A. Fink, et al., “2017 American College of Rheumatology Guideline for the Prevention and Treatment of Glucocorticoid-Induced Osteoporosis,” Arthritis Care and Research 69 (2017): 1095–1110, https://doi.org/10.1002/acr.23279.
- B. Claytor and Y. Li, “Opinions on Pneumocystis Jirovecii Prophylaxis in Autoimmune Neuromuscular Disorders,” Muscle & Nerve 65 (2022): 278–283, https://doi.org/10.1002/mus.27481.
- T. Pike-Lee, S. Syed, M. A. Willis, and Y. Li, “Pneumocystis Jirovecii Pneumonia in Neurologic Disorders: Is Prophylaxis Necessary?,” Neurology Clinical Practice 11 (2021): 242–248, https://doi.org/10.1212/CPJ.0000000000000923.
- D. M. Shafran, P. E. Bunce, and W. L. Gold, “Reducing the Risk of Infection in a 74-Year-Old Man Who Is to Receive Prednisone,” Canadian Medical Association Journal 186 (2014): 1239–1240, https://doi.org/10.1503/cmaj.131430.
- A. Caplan, N. Fett, M. Rosenbach, V. P. Werth, and R. G. Micheletti, “Prevention and Management of Glucocorticoid-Induced Side Effects: A Comprehensive Review. Gastrointestinal and Endocrinologic Side Effects,” Journal of the American Academy of Dermatology 76 (2017): 11–16, https://doi.org/10.1016/j.jaad.2016.02.1239.
- R. R. MacGregor, J. N. Sheagren, M. B. Lipsett, and S. M. Wolff, “Alternate-Day Prednisone Therapy. Evaluation of Delayed Hypersensitivity Responses, Control of Disease and Steroid Side Effects,” New England Journal of Medicine 280 (1969): 1427–1431, https://doi.org/10.1056/NEJM196906262802601.
- G. I. Wolfe, H. J. Kaminski, I. B. Aban, et al., “Randomized Trial of Thymectomy in Myasthenia Gravis,” New England Journal of Medicine 375 (2016): 511–522, https://doi.org/10.1056/NEJMoa1602489.
- T. Sharshar, R. Porcher, S. Demeret, et al., “Comparison of Corticosteroid Tapering Regimens in Myasthenia Gravis: A Randomized Clinical Trial,” JAMA Neurology 78 (2021): 426–433, https://doi.org/10.1001/jamaneurol.2020.5407.
- F. L. Mastaglia, B. A. Phillips, and P. J. Zilko, “Inflammatory Myopathy,” Current Treatment Options in Neurology 1 (1999): 263–272, https://doi.org/10.1007/s11940-999-0008-6.
- K. Fitch, ed., The Rand/UCLA Appropriateness Method User's Manual (Santa Monica: Rand, 2001).
- D. Huscher, K. Thiele, E. Gromnica-Ihle, et al., “Dose-Related Patterns of Glucocorticoid-Induced Side Effects,” Annals of the Rheumatic Diseases 68 (2009): 1119–1124, https://doi.org/10.1136/ard.2008.092163.
- G. R. Burmester, F. Buttgereit, C. Bernasconi, et al., “Continuing Versus Tapering Glucocorticoids After Achievement of Low Disease Activity or Remission in Rheumatoid Arthritis (SEMIRA): A Double-Blind, Multicentre, Randomised Controlled Trial,” Lancet 396 (2020): 267–276, https://doi.org/10.1016/S0140-6736(20)30636-X.
- K. Briot, B. Cortet, C. Roux, et al., “2014 Update of Recommendations on the Prevention and Treatment of Glucocorticoid-Induced Osteoporosis,” Joint, Bone, Spine 81 (2014): 493–501, https://doi.org/10.1016/j.jbspin.2014.10.001.
- 20G. Adami and K. G. Saag, “Glucocorticoid-Induced Osteoporosis Update,” Current Opinion in Rheumatology 31 (2019): 388–393, https://doi.org/10.1097/BOR.0000000000000608.
- L. Buckley and M. B. Humphrey, “Glucocorticoid-Induced Osteoporosis. Solomon CG, Editor,” New England Journal of Medicine 379 (2018): 2547–2556, https://doi.org/10.1056/NEJMcp1800214.
- S. H. Yale and A. H. Limper, “Pneumocystis Carinii Pneumonia in Patients Without Acquired Immunodeficiency Syndrome: Associated Illnesses and Prior Corticosteroid Therapy,” Mayo Clinic Proceedings 71 (1996): 5–13, https://doi.org/10.4065/71.1.5.
- K. L. Winthrop and J. W. Baddley, “Pneumocystis and Glucocorticoid Use: To Prophylax or Not to Prophylax (And When?); That Is the Question,” Annals of the Rheumatic Diseases 77 (2018): 631–633, https://doi.org/10.1136/annrheumdis-2017-212588.
- H. Green, M. Paul, L. Vidal, and L. Leibovici, “Prophylaxis of Pneumocystis Pneumonia in Immunocompromised Non-HIV-Infected Patients: Systematic Review and Meta-Analysis of Randomized Controlled Trials,” Mayo Clinic Proceedings 82 (2007): 1052–1059, https://doi.org/10.4065/82.9.1052.
- C. D. Kassardjian, J. Widdifield, J. M. Paterson, et al., “Serious Infections in Patients With Myasthenia Gravis: Population-Based Cohort Study,” European Journal of Neurology 27 (2020): 702–708, https://doi.org/10.1111/ene.14153.
- O. Etzion and M. G. Ghany, “Screening for Hepatitis B Virus to Prevent Viral Reactivation—Who and When?,” Clinics in Liver Disease 5 (2015): 47–50, https://doi.org/10.1002/cld.458.
- J. W. Park, J. R. Curtis, M. J. Kim, H. Lee, Y. W. Song, and E. B. Lee, “Pneumocystis Pneumonia in Patients With Rheumatic Diseases Receiving Prolonged, Non-High-Dose Steroids—Clinical Implication of Primary Prophylaxis Using Trimethoprim–Sulfamethoxazole,” Arthritis Research & Therapy 21 (2019): 207, https://doi.org/10.1186/s13075-019-1996-6.
- D. E. Prior, E. Nurre, S. L. Roller, et al., “Infections and the Relationship to Treatment in Neuromuscular Autoimmunity,” Muscle & Nerve 57 (2018): 927–931, https://doi.org/10.1002/mus.26032.
Creation of New Guidelines, Consensus Statements, or Position Papers
AANEM members are encouraged to submit ideas for papers that can improve the understanding of the field. The AANEM will review nominated topics on the basis of the following criteria:- Members’ needs
- Prevalence of condition
- Health impact of condition for the individual and others
- Socioeconomic impact
- Extent of practice variation
- Quality of available evidence
- External constraints on practice
- Urgency for evaluation of new practice technology
