Electrodiagnostic Reference Values for Upper and Lower Limb NCS in Adult Populations
ABSTRACT: Introduction: To address the need for greater standardization within the field of electrodiagnostic medicine, the Normative Data Task Force (NDTF) was formed to identify nerve conduction studies (NCS) in the literature, evaluate them using consensus-based methodological criteria derived by the NDTF, and identify those suitable as a resource for NCS metrics. Methods: A comprehensive literature search was conducted of published peer-reviewed scientific articles for 11 routinely performed sensory and motor NCS from 1990 to 2012. Results: Over 7,500 articles were found. After review using consensus-based methodological criteria, only 1 study each met all quality criteria for 10 nerves. Conclusion: The NDTF selected only those studies that met all quality criteria and were considered suitable as a clinical resource for NCS metrics. The literature is, however, limited and these findings should be confirmed by larger, multicenter collaborative efforts. A literature search was conducted on all studies published in English or other languages translated into English from 1990 to 2012 using the words “nerve conduction” or “nerve conduction studies,” and the names of the 11 sensory and motor nerves routinely tested in the upper and lower extremities in the following databases: PubMed/Medline; EMBASE; Web of Science; and Scopus. Specifically, the search terms for the studied nerves included “radial sensory,” “median sensory,” “ulnar sensory,” “median motor,” “ulnar motor,” “medial antebrachial cutaneous,” “lateral antebrachial cutaneous,” “sural,” “superficial peroneal,” “peroneal motor,” and “tibial motor.” *Studies of median and ulnar comparison analyses from the primary studies, yet published separately. Findings were derived from the primary sample using the same methodology, inclusion criteria, and statistical analyses. Over 7,500 studies were found dealing with 11 sensory and motor nerves (Table 1), and a total of 401 met the sample size criterion of >100 healthy subjects. An initial evaluation of the articles led to a recommendation that 83 undergo detailed review. Studies that met all NDTF criteria were identified, and results for each sensory or motor nerve are described in Tables 2–5. *Values for the entire sample for each nerve encompassing all ages. †Upper limit of normal is the 97th percentile of the observed differences distribution for the onset latency. There were age effects, thus cut-offs are shown by age subgroups. Differences in motor latencies are shown with wrist stimulation over each nerve at 8 cm from recording electrodes over abductor pollicis brevis for median and abductor digiti minimi for ulnar. After review of >7,500 studies, 401 had the required sample sizes of >100, and 10 studies were identified for the 11 nerves (a single acceptable study for each nerve). The reasons that so few studies met these criteria are likely multifactorial. Conducting large-scale normative studies is time-consuming and requires significant resources, meeting a sample size of >100 subjects is daunting, and funding sources are limited. Many studies obtained reference data in the context of studying a target disorder and used healthy subjects as a control. Data from many studies did not address the non-Gaussian distribution of NCS parameters and often derived cut-off values using the mean and standard deviations rather than percentiles. The NDTF used consensus criteria to systematically review published studies on NCS on 11 commonly tested nerves and identified only 1 study that met all criteria for each of the 10 nerves. This limited set of reference metrics may be suitable for consideration for use by EDx practitioners.
SHAN CHEN, MD, PhD,1 MICHAEL ANDARY, MD, MS,2 RALPH BUSCHBACHER, MD,3 DAVID DEL TORO, MD,4 BENN SMITH, MD,5 YUEN SO, MD,6 KUNO ZIMMERMANN, DO, PhD,7 and TIMOTHY R. DILLINGHAM, MD8
Muscle Nerve 54: 371–377, 2016
Electrodiagnostic (EDX) testing is used extensively to diagnose neuromuscular disorders but a universal standard for nerve conduction studies (NCS) is not available.1,2 Individual laboratories have been encouraged to use their own techniques for performing NCS and develop their own reference data, “despite inherent methodological and statistical challenges with this approach.” Other EDX physicians and laboratories have relied on reference data in textbooks or values passed along by academic teaching laboratories. However, many published studies2 do not meet contemporary statistical and methodological standards. Nerve conduction testing can be challenging and is dependent upon the skill of the EDX practitioners,2 instrumentation, and testing circumstances that have been discussed.1,2 The American Association of Neuromuscular & Electrodiagnostic Medicine (AANEM) formed the Normative Data Task Force (NDTF) to establish a set of evidence-based criteria to screen the peer-reviewed published literature.1,2 The NDTF’s report details the results of the review and selection of suitable articles regarding 11 routinely studied nerves.METHODS
All studies identified by the initial search were reviewed by an AANEM administrative staff member or an NDTF member (Table 1) to determine whether there was a sample size of >100 healthy subjects.2 Abstracts that met the sample size inclusion criteria were then reviewed by an NDTF member assigned to that particular nerve. Full articles were obtained and reviewed in detail to determine whether they were focused on deriving normative data and if they appeared to meet NDTF criteria. Articles that appeared to meet most of the NDTF criteria were circulated to all members for review. The members discussed each review either in person or through e-mail. A standardized grading form was used to grade each article. The techniques, statistical methods, instrumentation, and study design were rated based on 7 NDTF criteria as defined in an accompanying article.2
Table 1. Identification process for selecting studies meeting the Normative Data Taskforce (NDTF) criteria from the published literature spanning 1990–2012. Number of articles identified Search results Initial review NDTF review Final selected studies (first author and year) for reference values [other studies with useful information] Upper extremity nerves Superficial radial sensory 418 18 5 Evanoff 20063 [Benatar 20099] Median sensory 1,326 101 9 Buschbacher 19994 [Grossart 2006,20* Falco 199221] Ulnar sensory 940 40 12 Buschbacher 19995 [Grossart 2006,20* Benatar 20099] Medial antebrachial cutaneous sensory 65 11 3 Prahlow 20066 Lateral antebrachial cutaneous sensory 91 10 6 Buschbacher 20007 Median motor 1,111 43 25 Buschbacher 199911 (to the abductor pollicis brevis) [Grossart
2006,20* Foley 200612 (to the pronator quadratus), Foley
200613 (to the pronator teres/flexor carpi radialis)]Ulnar motor 1,211 47 5 Buschbacher 199911 [Grossart 2006,20* Ehler 2013,22
Falco 199221]Lower extremity nerves
Sural sensory nerve1,512 23 7 Buschbacher 20038 [Falco 199423] Superficial fibular (peroneal) sensory 157 33 2 No primary article was found that sufficiently met the criteria for quality [Kushnir 2005,24 Falco 199423] Fibular (peroneal) motor 161 65 5 Buschbacher 199915 [Mathis 201116 (to the accessory peroneal)] Tibial motor 539 10 4 Buschbacher 199917 (to the abductor hallicus), Buschbacher
199919 (to the flexor digiti minimi brevis)Total 7,531 401 83 RESULTS
Sensory Nerves. Among sensory nerves, 1 article met all NDTF criteria for: (1) superficial radial sensory nerve3; (2) median sensory nerve4; (3) ulnar sensory nerve5; (4) medial antebrachial cutaneous sensory nerve6; (5) lateral antebrachial cutaneous sensory nerve7; and (6) sural sensory nerve.8 The superficial fibular (peroneal) sensory nerve was the only sensory nerve for which no studies met NDTF criteria. The articles, their specific testing conditions, and EDX parameters are outlined in Tables 1–3.
In the sural nerve study chosen by the NDTF, nerve responses were absent bilaterally in 4 persons and were unilaterally absent in 4 others, yielding recordable sural responses on both sides in 97% of subjects.8 Sensory nerve conduction velocities were not calculated in the study selected, and another study was cited that examined conduction velocity but did not meet all NDTF criteria.9,10 Quantile regression was used by this group to provide reference values (cut-offs) for velocities. The third percentiles (lowest cut-off for normality) were 43m/s, 45m/s, and 50m/s for median, ulnar, and radial sensory nerves, respectively. The lower limit of normal for the sural sensory nerve was 40m/s. Median and ulnar sensory nerve amplitudes were influenced by age and body mass index (BMI) and these subgroups are shown in table 3.
Motor Nerves. For the median motor nerve, 1,111 articles were initially identified, and 25 studies were sent for NDTF review; only 3 met most of the NDTF criteria, and 1 article met all criteria.11 This study included 249 subjects and considered the effects of age, gender, and height on the NCS parameters; separate reference data were provided if the effect of the relevant variable was significant at P < 0.01. For amplitude, age but not gender was found to be relevant, and these reference values are shown in Table 4. For both latencies and conduction velocities, gender and age were found to have small but significant effects, and these subgroups are shown in Table 4. Height had no significant effect on the median motor NCS parameters.11 Two other articles that met all criteria examined median motor nerve conduction to the pronator quadratus12 and to the pronator teres and flexor carpi radialis muscles.13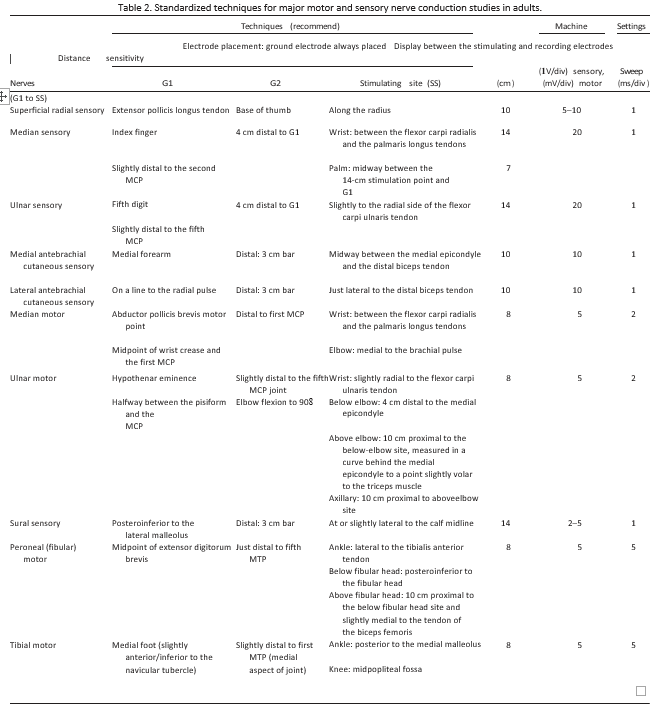
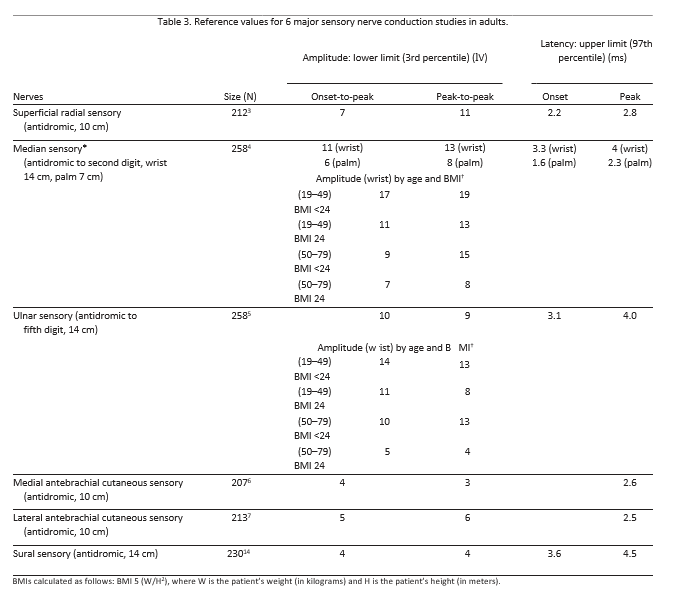
*Median sensory NCS data shown were recorded at digit 2. Normative data recorded at digit 3 are also available in the same article.4 The digit 3 findings are similar in magnitude to data derived from digit 2. †The lower limits of onset-to-peak and peak-to-peak amplitudes are shown as mean – 2 SD, showing the statistically significant effects of age and BMI on the amplitudes of the median and ulnar sensory nerves at the wrist (P < 0.01). Data sets normalized by square-root transformation.
The fibular (peroneal) motor nerve literature review revealed 161 studies, and 1 article that studied the fibular (peroneal) motor nerve to the extensor digitorum brevis muscle was selected.15 This study of 242 subjects considered the influence of age and height as well as side-to-side and segmental differences. Increasing height was found to correlate with decreasing conduction velocity, and increasing age was found to correlate with decreases in both conduction velocity and amplitude (Table 4). The upper limit (at the 97th percentile) of normal drop in velocity from the lower leg to the across-knee segment was 6m/s or 12%, and the upper limit of normal drop in amplitudes from below to above the fibular head was 25%.15 Of note, the amplitude in the older age category was less than half that of the younger age group (Table 4).
One study16 examined both the accessory deep fibular (peroneal) motor nerve [ADPN, a branch of superficial fibular (peroneal) motor nerve] and the deep fibular (peroneal) motor nerve conduction to the extensor digitorum brevis muscle in 200 subjects. This article is mentioned because it contains information regarding the prevalence of the ADPN in normal individuals, which is 13.5%.
For the tibial motor nerve, 539 studies were initially identified, and 2 met all NDTF criteria. One article that studied tibial motor nerve conduction to the abductor hallucis was selected.17 This study of 250 subjects considered the influence of independent variables of age, gender, and height on the NCS parameters and included side-to-side and segmental differences. Similar to the fibular motor nerve,15 increasing height was found to correlate with decreasing conduction velocity, and increasing age was found to correlate with decreases in velocity and amplitude (Table 4).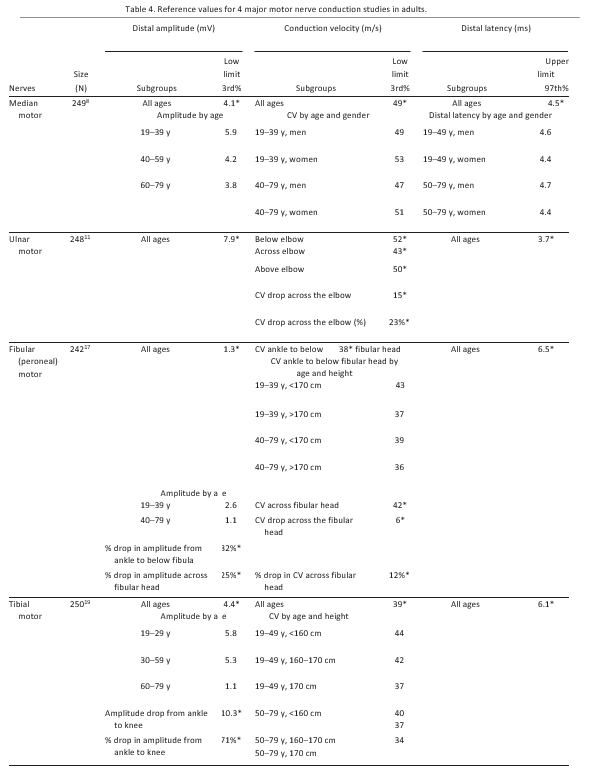
The upper limit of normal drop in amplitude from the ankle to the knee was 10.3 mV, or 71% (larger than the fibular motor segmental drop).17 This degree of amplitude drop is unusual and surprising to some clinicians. It can be misinterpreted to represent conduction block due to demyelinating neuropathy. This amplitude drop in normal subjects is most likely due to temporal dispersion and phase cancellation between the multiple distal tibial innervated foot muscles recorded by the reference electrode.18 One other article also met all the criteria and evaluated the lateral tibial motor nerve conduction to the flexor digit minimi brevis muscle, a less commonly used technique for testing this nerve.19
Median-to-Ulnar and Ulnar-to-Median Motor and Sensory Nerve Comparisons. Comparisons of median and ulnar motor nerve conduction across the wrist, (intra-hand comparisons) are helpful in minimizing the confounding effects of age, height, and limb temperature. A comparison of these latency comparisons provides reference values and utilizes the same methodology, sample, and non-parametric statistics as in the main articles (Table 5).20 The distribution of median-to-ulnar motor latency comparisons differed from ulnar-to-median motor latency comparisons. 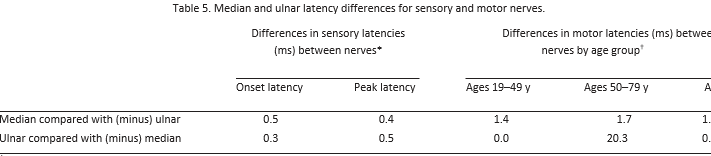
*Upper limit of normal is the 97th percentile of the observed differences distribution. There were no age effects, thus the data are combined. Differences in sensory latencies are shown with wrist stimulation over the median nerve at 14 cm recording over digit 3, and stimulation over the ulnar nerve at 14 cm recording over digit 5.
For the median-to-ulnar motor comparisons, when the median nerve was investigated, the maximal difference (97th percentile) in onset latency for persons age <50 years was 1.4 ms and for patients age >50 years it was 1.7 ms. In contrast, when the ulnar nerve was the nerve of interest, the ulnar-to-median latency comparison was 0.0 ms for the younger group and –0.3 ms for the older group. This means that the ulnar motor latency should not be longer than the median motor latency. If it is, then ulnar nerve pathology across the wrist may be present.20 Median and ulnar sensory nerve latency comparisons, in contrast to the motor nerve comparisons, did not show a substantial age influence. For the entire group, the median-to-ulnar peak latency comparison had an upper (97th percentile) limit of 0.4 ms, whereas the ulnar-to-median upper limit comparison was similar at 0.5 ms (Table 5).20DISCUSSION
The NDTF first developed standardized criteria and then applied the criteria to screen and review the published literature dealing with normative results for 11 routinely performed sensory and motor NCS in the upper and lower extremities. The techniques and instrument settings used in these studies are readily programmed into modern EDX equipment and are easily duplicated.
The final selected studies emanated from a single research group and have both strengths and limitations. Sample sizes were all >200 subjects and provided statistical power to the analyses. These analyses included multiple covariates known to influence NCS parameters: age; gender; body mass index; and height. The studies, however, reflect findings from a single regional population of healthy adults and a single EDX laboratory. Future studies from other laboratories that sample subjects from other geographical regions will be necessary to validate these data and fully confirm the level of generalizability for the results. Until such data are available, EDX physicians may use these normative data now in their clinical practices.
Future studies of this type or a laboratory wishing to develop its own set of metrics should utilize the NDTF criteria to carefully address testing methods and study design. These NDTF selection criteria can assist journal editors and reviewers when evaluating manuscripts submitted for publication.
The NDTF limited the scope of the work to commonly tested nerves in adult populations. Future efforts should address reference values for less commonly tested nerves and should include late responses (F-waves and H-reflexes) and studies on pediatric populations.
In the future, a multicenter study with a larger and more geographically and ethnically diverse sample would be useful to better clarify the generalizability of these studies and more precisely examine the important influences of age, gender, height, and body mass index on clinical NCS parameters.CONCLUSIONS
The NDTF gratefully acknowledges the assistance of the AANEM Practice Issue Review Panel for review and critique of the manuscript. The NDTF also acknowledges Carrie Winter, Shirlyn Adkins, Seng Vang, Catherine French, and Adam Blaszkiewicz for their tireless administrative support of this project. The authors thank Larry Robinson, MD, and William Litchy, MD, for their thoughtful input in the early stages of this project. We also thank Katie McCausland, DO, for assistance with the ulnar and fibular (peroneal) motor nerves.
References
- American Association of Electrodiagnostic Medicine. Guidelines in electrodiagnostic medicine. Muscle Nerve 1999;22(suppl):S3–S300.
- Dillingham T, Chen S, Andary M, Buschbacher R, Del Toro D, Smith B, et al. Establishing high quality reference values for nerve conduc- tion studies: a report from the Normative Data Task Force of the AANEM. Muscle Nerve 2016;XX:000–000.
- Evanoff V Jr, Buschbacher RM. Radial versus dorsal ulnar cutaneous sensory studies. J Long Term Eff Med Implants 2006;16:349–357.
- Buschbacher RM. Median 14-cm and 7-cm antidromic sensory studies to digits two and three. Am J Phys Med Rehabil 1999;78(suppl):S53– S62.
- Buschbacher RM. Ulnar 14-cm and 7-cm antidromic sensory studies to the fifth digit: reference values derived from a large population of normal subjects. Am J Phys Med Rehabil 1999;78(suppl):S63–S68.
- Prahlow ND, Buschbacher RM. An antidromic study of the medial antebrachial cutaneous nerve, with a comparison of the differences between medial and lateral antebrachial cutaneous nerve latencies. J Long Term Eff Med Implants 2006;16:369–376.
- Buschbacher R, Koch J, Emsley C, Katz B. Electrodiagnostic reference values for the lateral antebrachial cutaneous nerve: standardization of a 10-cm distance. Arch Phys Med Rehabil 2000;81:1563–1566.
- Buschbacher RM. Sural and saphenous 14-cm antidromic sensory nerve conduction studies. Am J Phys Med Rehabil 2003;82:421–426.
- Benatar M, Wuu J, Peng L. Reference data for commonly used sen- sory and motor nerve conduction studies. Muscle Nerve 2009;40:772– 794.
- Peng L, Wuu J, Benatar M. Developing reference data for nerve con- duction studies: an application of quantile regression. Muscle Nerve 2009;40:763–771.
- Buschbacher R. Median motor nerve conduction to the abductor pol- licis brevis. Am J Phys Med Rehabil 1999;78(suppl):S1–S8.
- Foley B, Roslonski E, Buschbacher R. Reference values for median motor nerve conduction to the pronator quadratus. Arch Phys Med Rehabil 2006;87:88–91.
- Foley B, Buschbacher R. Establishing normal values of the proximal median motor nerve—a study of the pronator teres and flexor carpi radialis in healthy volunteers. J Long Term Eff Med Implants 2006; 16:341–347.
- Buschbacher RM. Ulnar nerve motor conduction to the abductor digiti minimi. Am J Phys Med Rehabil 1999;78(suppl):S9–S14.
- Buschbacher RM. Peroneal nerve motor conduction to the extensor digitorum brevis. Am J Phys Med Rehabil 1999;78(suppl):S26–S31.
- Mathis S, Ciron J, du Boisgu,eheneuc F, Godene`che G, Hobeika L, Larrieu D, et al. Study of accessory deep peroneal nerve motor con- duction in a population of healthy subjects. Neurophysiol Clin 2011; 41:29–33.
- Buschbacher RM. Tibial nerve motor conduction to the abductor hallucis. Am J Phys Med Rehabil 1999;78(suppl):S15–S20.
- Barkhaus PE, Kincaid JC, Nandedkar SD. Tibial motor nerve conduc- tion studies: an investigation into the mechanism for amplitude drop of the proximal evoked response. Muscle Nerve 2011;44:776–782.
- Buschbacher RM. Tibial nerve conduction to the flexor digit minimi brevis. Am J Phys Med Rehabil 1999;78(suppl):S21–S25.
- Grossart E, Prahlow N, Buschbacher R. Acceptable differences in sen- sory and motor latencies between the median and ulnar nerves. J Long Term Eff Med Implants 2006;16:395–399.
- Falco FJ, Hennessey WJ, Braddom RL, Goldberg G. Standardized nerve conduction studies in the upper limb of the healthy elderly. Am J Phys Med Rehabil 1992;71:263–271.
- Ehler E, RidzoA P, Urban P, Mazanec R, Nakl,adalov,a M, Proch,azka B, et al. Ulnar nerve at the elbow—normative nerve conduction study. J Brachial Plex Peripher Nerve Inj 2013;8:2.
- Falco FJ, Hennessey WJ, Goldberg G, Braddom RL. Standardized nerve conduction studies in the lower limb of the healthy elderly. Am J Phys Med Rehabil 1994;73:168–174.
- Kushnir M, Klein C, Kimiagar Y, Pollak L, Rabey JM. Medial dorsal superficial peroneal nerve studies in patients with polyneuropathy and normal sural responses. Muscle Nerve 2005;31:386–389.
Document History
Approved by the American Association of Neuromuscular & Electrodiagnostic Medicine: May 2016
This guideline is greater than 5 years old. Every 5 years, an interim literature search is performed and the guideline is reviewed. While new studies have been published since this guideline was last reviewed, the Practice Issue Review Panel Committee of the AANEM has determined that these studies are not sufficient to mandate a revision of this guideline at the present time. The information contained in this guideline and the recommendations offered are still relevant to current practice.
Reaffirmed by the Practice Issue Review Panel: October 2022
Creation of New Guidelines, Consensus Statements, or Position Papers
AANEM members are encouraged to submit ideas for papers that can improve the understanding of the field. The AANEM will review nominated topics on the basis of the following criteria:- Members’ needs
- Prevalence of condition
- Health impact of condition for the individual and others
- Socioeconomic impact
- Extent of practice variation
- Quality of available evidence
- External constraints on practice
- Urgency for evaluation of new practice technology
