Practice Parameter for EDX Studies in CTS: Summary Statement (including literature review)
*Approved by the American Association of Electrodiagnostic Medicine: January 2002, original document approved April 1993. Approved by the American Academy of Neurology: February 2002, original document endorsed, February 1993. Endorsed by the American Academy of Physical Medicine and Rehabilitation: February 2002, original document endorsed, March 1993. *For each EDX technique to summarize results across studies, sensitivities were pooled from individual studies by calculating a weighted average. In calculating the weighted average, studies enrolling more patients received more weight than studies enrolling fewer patients. Specificities were similarly pooled by calculating the weighted average. The data in the parentheses below the sensitivity and specificity values represent the lower and upper 95% confidence limits of the weighted average, respectively. Data analysis courtesy of Dr. Gary Gronseth. †There was heterogeneity between some of the studies (the 95% confidence intervals of the sensitivities and specificities do not overlap). This disparity may be related to differences in case definition of CTS, the use of different cut-points to define an abnormal value, and differences in the average severity of the CTS patients in the different studies. ‡Results based on a single study. REFERENCES INTRODUCTION AAEM CTS LITERATURE INCLUSION CRITERIA Description of the Review Process DESCRIPTION OF DATA PRESENTATION REVIEWER OBSERVATIONS REVIEW OF EDX STUDIES RESULTS Median Motor Nerve Conduction Studies Martin-Gruber Anastomosis. The Martin-Gruber anastomosis describes the anomalous communication in the forearm of nerve fibers from the median nerve to the ulnar nerve, and its presence may affect the results of median motor NCSs in CTS. Stimulation
of the median nerve at the elbow ordinarily results in the selective activation of median innervated intrinsic hand muscles. In the presence of a Martin-Gruber anomaly, however, ulnar and median innervated hand muscles are simultaneously activated
by stimulation of the median nerve at the elbow.93,107,129,141 Median-Thenar to Ulnar-Thenar Latency Difference. The TTLD method was unusual because the CMAP is recorded over the thenar eminence (active electrode over the APB) with sequential stimulation at the wrist of first the median and then the
ulnar nerves and one calculates the difference (TTLD) between the distal latency with median and ulnar nerve stimulation. The CMAP recorded over the thenar eminence with ulnar nerve stimulation at the wrist begin with an initial positive deflection
because the CMAP was in part volume conducted from the hypothenar muscles (Sander220). There are no studies of this method that meet all 6 AAEM CTS LIC. In a study that met 5 of the 6 AAEM CTS LIC, Sander220 noted the
sensitivity of the TTLD study approached the sensitivity of median mixed nerve palmar studies because 95% of CTS patients with abnormal median mixed nerve palmar studies showed abnormal TTLD. lateral to the midpoint of the third metacarpal) with stimulation at the wrist for both the median and ulnar nerves. The median nerve CMAP is recorded from the dorsal interosseus deep to the second lumbrical in the palm with the same set
of recording electrodes.200 In contrast to the TTLD methodology described above, both CMAPs have an initial negative deflection. Median Sensory NCSs Needle EMG of the Thenar Muscle in CTS Sympathetic Skin Response in CTS AAEM CTS LIC, reported that 24% (33/139) of symptomatic hands of CTS patients had a prolonged SSR latency (>1.72 s). However, Sener,223 in a study that met all 6 AAEM CTS LIC, reported that none of the 44 symptomatic limbs in CTS
patients showed a SSR latency greater than limbs of 20 normal subjects (Table 21). Sener223 used sternal stimulation to avoid the potential effect of afferent dysfunction in a limb on the SSR results. These results indicate that CTS
is an unlikely cause of median nerve SSR abnormalities. Furthermore, the SSR study, like the F-wave study, does not localize the abnormality to the CTS segment of the median nerve. Interestingly both Verghese259 and Sener
223 noted over half of the CTS patients complained of at least 1 symptoms in the affected hand that may indicate autonomic dysfunction: swelling of the hand or fingers, dryness, excessive perspiration, pallor, red or purple discoloration,
and coolness. However, for the reasons noted above, SSR studies are not recommended as an EDX study to diagnose CTS patients. The Effect of Limb Ischemia, Dynamic Hand Exercises, and Brief and Sustained Wrist Positioning on Median NCSs in CTS Effect of Limb Ischemia on Median Nerve Conduction in Carpal Tunnel Syndrome. In 1953, Gilliatt and Wilson86 described the production of paresthesia in limbs of CTS patients with a pneumatic tourniquet. As noted above, in
1963, Fullerton76 evaluated the effect of upper extremity ischemia on median motor conduction in the forearm and hand and suggested that transient nocturnal symptoms were due to median nerve ischemia. Limb ischemia caused the median
thenar CMAP amplitude to fall to less than 40% of the initial value after 25 minutes in 7 out of 15 CTS patients whereas the median thenar CMAP amplitude in normal subjects remained above 50% of the initial value after 30 minutes of ischemia. In 1981, Gelberman and colleagues78 made direct measurements of the intracarpal tunnel pressure with a wick catheter and noted that (1) intracarpal tunnel pressure with the wrist in the neutral position is increased in patients with CTS
compared to control subjects (2) intracarpal tunnel pressureincreases in CTS and control subjects with wrist flexion and extension and (3) intracarpal pressure changes in CTS patients (greater than 50 mm Hg for several minutes) were sufficient
to cause rapidly reversible (ischemic) nerve conduction block. Gelberman79 recently reviewed these findings and subsequent supporting literature on intracarpal tunnel measurements. Other EDX Studies in CTS Several other variations on median sensory and motor NCSs have been reported to be useful for the evaluation of patients with CTS. The review of the literature through 2000 indicated that the value of these tests for the clinical EDX evaluation of
patients with CTS still remains to be established and these studies are considered investigational. These EDX studies include the following: (1) measurement of the refractory period of the median nerve,84,190,249 (2) anterior
interosseus latency measurements,231 (3) anterior interosseous/median nerve latency ratio,215 (4) temporal dispersion of the SNAP,98 and (5) distal stimulation of the “pulp” of digits.229 Several
investigators have used CTS patients to evaluate EDX studies, not from the standpoint of using the EDX study to diagnose CTS, but from the standpoint that CTS is a model of focal nerve compression.8,11,51,126,208,260 Statistical Considerations: Normal Values, Normal Distributions, Use of Multiple Tests, Receiver-Operating Curves Comparison of Sensitivity of Different EDX Studies Based on the data reviewed in the Results, median sensory and motor nerve CV studies including comparison of median sensory conduction to ulnar and radial sensory conduction in the same hand are more sensitive and specific for the diagnosis
of CTS than measurements of (1) median SNAP amplitudes and amplitude ratios, (2) motor CMAP amplitudes and amplitude ratios, (3) F-wave parameters, and (4) sympathetic skin responses. The recommendations below are identical to those made and endorsed in 19937 by the AAN, the AAPMR, and the 2. Definition Of Practice Recommendation Strengths The strength of a recommendation or conclusion is based on the quality and consistency of supporting evidence. The following rating system is used: RECOMMENDATIONS FOR FUTURE RESEARCH STUDIES IN CTS The AAEM recommends that future clinical research studies of the usefulness of EDX studies to confirm the diagnosis of CTS meet 3 clinical study criteria: The first and second AAEM CTS Literature Reviews1,2 used 6 CTS LIC. The second CTS Literature Review2 recommended (1) the addition of criterion 3 and (2) that future AAEMCTS Literature Reviews use all 7 CTS LIC to review reports of the usefulness of EDX studies in the evaluation of CTS patients. The second AAEM CTS Literature Review2 also provided a set of specific criteria to make a clinical diagnosis of
CTS based on expert opinion (Table 2). DISCUSSION This report includes 2 recommendations in addition to those in the 1993 CTS Literature Review to improve future clinical research studies of the usefulness of EDX studies to confirm the clinical diagnosis of CTS. In the 1993 AAEM CTS Literature Review, it was recommended that an outcome study be performed to assess the harms, benefits, and costs of performing NCSs and needle EMG in patients with symptoms suggestive of CTS. In 1994, Boniface and colleagues20 published
a prospective study from England which demonstrated that NCS/EMG studies were useful and cost effective in management of patients suspected of CTS.20 In addition, the AAEM has encouraged additional outcome studies including the publication
of guidelines for outcome studies in neuromuscular diseases including CTS.108 The AAEM Research and Education Foundation has recently funded a prospective outcome study of 400 patients to evaluate the usefulness of EDX studies in the
evaluation and management of patients with symptoms suggestive of CTS. It is recommended that outcome studies continue to be a priority for future clinical research in the diagnosis and management of CTS and other neuromuscular diseases. INTERFACE W ITH AAEM GUIDELINES SUMMARY OF HARMS, BENEFITS, AND COSTS FOR INTERVENTIONS CONSIDERED
DISCLAIMER
Carpal tunnel syndrome (CTS) is a common clinical problem and frequently requires surgical therapy. The results of electrodiagnostic (EDX) studies have been found to be highly sensitive and specific for the diagnosis of CTS. This document defines the standards, guidelines, and options for EDX studies of CTS based on a critical review of the literature published in 19931 and recently updated by a review of the literature through the year 2000.2 The reader is referred to the updated review2 for a detailed discussion of the literature and the EDX techniques for the assessment of CTS which are summarized here. Both reviews addressed the following key clinical questions:
1. In patients clinically suspected of having CTS, what are the best EDX studies to confirm the diagnosis? 2. How can future clinical research studies be improved to evaluate the usefulness of laboratory studies, including EDX studies, to confirm the diagnosis of CTS?
Reviewed and revised in 2001 by the American Association of Electrodiagnostic Medicine (AAEM) CTS Task Force: Charles K Jablecki, MD, Chair; Michael T. Andary, MD, MS; Mary Kay Floeter MD, PhD; Robert G. Miller, MD; Caroline A. Quartly, MD, FRCP(C); Michael J. Vennix, MD; John R. Wilson, MD. American Academy of Neurology (AAN) Quality Standards Subcommittee: Gary M. Franklin, MD, Co-chair; Catherine A. Zahn, MD, FRCP(C), MHSc, Co-chair; Milton Alter, MD, PhD; Stephen Ashwal, MD; Rose M. Dotson, MD; Richard M. Dubinsky, MD; Jacqueline French, MD; Gary H. Friday, MD; Michael Glantz, MD; Gary S. Gronseth, MD; Deborah Hirtz, MD; James Stevens, MD; David J. Thurman, MD, MPH; William Weiner, MD. American Academy of Physical Medicine and Rehabilitation (AAPM&R) Practice Guidelines Committee: John C. Cianca, MD; Gerard E. Francisco, MD; Thomas L. Hedge, Jr., MD; Deanna M. Janora, MD; Ajay Kumar, MD; Gerard A, Malanga, MD; Jay M. Meythaler, MD, JD; Frank J. Salvi, MD; Richard D. Zorowitz, MD.
Authors had nothing to disclose.
Original document developed in 1993 by the AAEM Quality Assurance Committee: Charles K. Jablecki, MD, Chair; Michael T. Andary, MD, MS; Richard D. Ball, MD, PhD; Michael Cherington, MD; Morris A Fisher, MD; Lawrence H. Phillips II, MD; Yuen T. So, MD, PhD; John W . Tulloch, MD; Margaret A. Turk, MD; David O. Wiechers, MD, MS; Asa J. Wilbourn, MD; Dennis E. W ilkins, MD; Faren H. Williams, MD; Roy G. Ysla, MD. American Academy of Neurology (AAN) Quality Standards Subcommittee: Jay H. Rosenberg MD, Chair; Milton Alter, MD, PhD; Jasper R. Daube, MD; Gary Franklin, MD, MPH; Benjamin M. Frishberg, MD; Michael K. Greenberg, MD; Douglas J. Lanska, MD; George Paulson, MD; Richard A. Pearl, MD; Cathy A. Sila, MD. American Academy of Physical Medicine and Rehabilitation (AAPM&R) Practice Parameters Committee: Carl V. Granger, MD, Chair; Joel A. DeLisa, MD; Myron M. LaBan, MD; James S. Lieberman, MD; Mark A. Tomski, MD; Margaret A. Turk, MD.
Key words: carpal tunnel syndrome; electromyography; literature review; nerve conduction study; reference values; sensitivity; specificity.
Correspondence to: American Association of Electrodiagnostic Medicine; e-mail: aaem@ aaem.net
© 2002 American Association of Electrodiagnostic Medicine.
Published by Wiley Periododicals, Inc.
Published online May 7, 2002 in Wiley InterScience (www.interscience. wiley.com). DOI 10.1002/mus.10185
DESCRIPTION OF THE REVIEW PROCESS
The source of the articles for the first CTS Literature Review1 published in 1993 was a Medline search for literature in English from January 1, 1986, through May 1991.
The Medical Subject Headings (MeSH) searched were (1)
wrist injuries or wrist joint, (2) nerve compression syndrome, and (3) carpal tunnel syndrome. The search identified 488 articles. Based on a review of the abstracts, 81 articles describing EDX studies were chosen for review. An additional 78 reports
were identified from the bibliographies of the 81 articles, and AAEM consultants recommended 6 others for a total of 165 articles. Of the 165 articles reviewed, 20 were classified as background references. The source of the articles for the second CTS
Literature Review2 was a Medline search for literature in English through December 2000. The MeSH searched were (1) carpal tunnel syndrome and diagnosis or (2) carpal tunnel syndrome and neural conduction. The search generated 497 article titles
with abstracts published since 1990. Based on a review of the abstracts, the AAEM CTS Task Force chose 92 articles for review. An additional 5 articles were identified from the bibliographies of the articles, and 16 from AAEM members who have current
research interests in CTS, for a total of 113 articles. Of the 113 articles reviewed, 24 were classified as background references.
DESCRIPTION OF THE REVIEWERS
In 1997, the AAEM President appointed Dr. Charles K.
Jablecki to Chair the AAEM CTS Task Force. The Chair selected the members of the AAEM CTS Task Force from the AAEM membership with the assistance of the AAEM staff and the AAEM President to include neurologists (Floeter, Jablecki, Wilson) and
physiatrists (Andary, Quartly, Vennix) in both academic (Andary, Floeter, Quartly, Vennix) and clinical practice (Jablecki, Wilson) with interests in the use of EDX studies in CTS. The AAEM CTS Task Force included three members who authored the first
CTS Literature Review published in 1993 (Jablecki, Andary, Wilson). In 1999, the AAEM President appointed Dr. Robert G. Miller to the AAEM CTS Task Force to provide an interface and full collaboration with the AAN Quality Standards Subcommittee in the
development of the second CTS Literature Review and the Summary Statement.
LITERATURE INCLUSION CRITERIA
In the fall of 1991, the AAEM Quality Assurance Committee adopted six literature inclusion criteria (LIC)
of scientific methodology to evaluate CTS literature describing EDX procedures. The AAEM CTS Task Force used the same six AAEM CTS LIC when reviewing the literature. The first two criteria apply to all studies of diagnostic tests and deal with the quality
of evidence and reducing bias; the remaining four criteria deal with technical and analytic issues that are critical to the use of nerve conduction studies (NCSs) to document nerve pathology. All of these criteria are important for a study to determine
whether or not a NCS is useful to diagnose CTS. The six LIC used were as follows:
1. Prospective study design. 2. Diagnosis of CTS in patient population based on clinical criteria independent of the EDX procedure under evaluation. 3. EDX procedure described in sufficient detail to permit replication of the procedure. 4. Limb temperature monitored (measured continuously) during nerve conduction procedures and minimum (or range) of limb temperatures reported for both CTS patients and the reference population. 5. Reference values for the EDX test obtained either: a. with concomitant studies of a reference population, or b. with previous studies of a reference population in the same laboratory. 6. Criteria for abnormal findings clearly stated and, if the measurement is a quantitative one, the abnormal value is defined in statistically computed terms, e.g., range and mean ± 2 standard deviations, from data derived from the reference
population.
REVIEW OF ELECTRODIAGNOSTIC STUDIES
A total of 22 of the 278 articles reviewed met all 6 AAEM CTS LIC. There were nine additional articles (eight using surface electrodes and one using needle electrodes) that studied median
motor and sensory nerve conduction across the carpal tunnel (amplitude, latency, and velocity) in normal subjects only and otherwise fulfilled the AAEM CTS LIC.
The first and second CTS Literature Reviews1,2 provide convincing,
scientific evidence that median sensory and motor NCSs:
1. are valid and reproducible clinical laboratory studies; and 2. confirm a clinical diagnosis of CTS with a high degree of sensitivity (>85%) and specificity (95%).
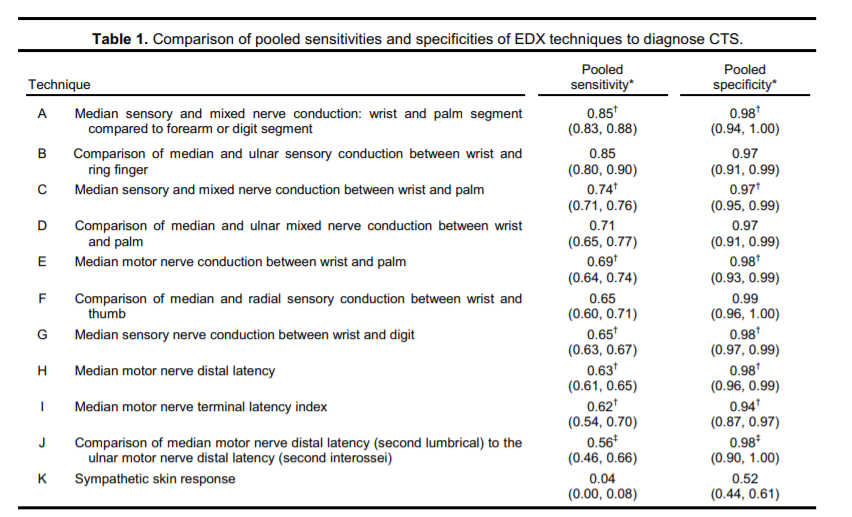
Table 1 provides a summary of pooled sensitivities and specificities from studies that met all six AAEM CTS LIC for EDX techniques used to diagnose CTS. In these studies, hand temperatures were monitored continuously and the majority of the studies
maintained the hand temperature at 32°C or greater. Details of techniques and the specific studies pooled are provided in the second CTS Literature review.2
DEFINITION OF PRACTICE RECOMMENDATION STRENGTHS
The strength of a recommendation or conclusion is based on the quality and consistency of supporting evidence. The following rating system is used:
Practice standards: generally accepted principles for patient
management that reflects a high degree of clinical certainty.
Practice guidelines: recommendations for patient management that reflect moderate clinical certainty.
Practice options: other strategies for
patient management for which the clinical utility is uncertain.
RECOMMENDATIONS REGARDING EDX STUDIES TO CONFIRM A CLINICAL DIAGNOSIS OF CTS
The recommendations below are identical to those made and endorsed in 1993 by the American Academy of Neurology,3 the American Academy of Physical Medicine and Rehabilitation,4 and the American Association of Electrodiagnostic Medicine5 with the clarification of recommendation 1 and 2a and the addition of 2c based on new evidence reviewed in the second CTS Literature Review.2
In patients suspected of CTS, the following EDX studies are recommended (See Table I for sensitivity and specificity of Techniques A–K):
1. Perform a median sensory NCS across the wrist with a conduction distance of 13 cm to 14 cm (Technique G). If the result is abnormal, comparison of the result of the median sensory NCS to the result of a sensory NCS of one other adjacent sensory nerve in the symptomatic limb (Standard). 2. If the initial median sensory NCS across the wrist has a conduction distance greater than 8 cm and the result is normal, one of the following additional studies is recommended: a. comparison of median sensory or mixed nerve conduction across the wrist over a short (7 cm to 8 cm) conduction distance (Technique C) with ulnar sensory nerve conduction across the wrist over the same short (7 cm to 8 cm) conduction distance (Technique D) (Standard), or b. comparison of median sensory conduction across the wrist with radial or ulnar sensory conduction across the wrist in the same limb (Techniques B and F) (Standard), c. comparison of median sensory or mixed nerve conduction through the carpal tunnel to sensory or mixed NCSs of proximal (forearm) or distal (digit) segments of the median nerve in the same limb (Technique A) (Standard). 3. Motor NCS of the median nerve recording from the thenar muscle (Technique H) and of one other nerve in the symptomatic limb to include measurement of distal latency (Guideline). 4. Supplementary NCS: comparison of the median motor nerve distal latency (second lumbrical) to the ulnar motor nerve distal latency (second interossei) (Technique J); median motor terminal latency index(Technique I); median motor nerve conduction between wrist and palm (Technique E); median motor nerve compound muscle action potential (CMAP) wrist-to-palm amplitude ratio to detect conduction block; median sensory nerve action potential (SNAP) wristto-palm amplitude ratio to detect conduction block; short segment (1 cm) incremental median sensory nerve conduction across the carpal tunnel (Option). 5. Needle electromyography (EMG) of a sample of muscles innervated by the C5 to T1 spinal roots, including a thenar muscle innervated by the median nerve of the symptomatic limb (Option).
Based on the second AAEM CTS Literature Review,2 the following EDX studies are not recommended to confirm a clinical diagnosis of CTS either because the EDX studies recommended above have greater sensitivity and specificity or the test is best described as investigational at this time.
1. Low sensitivity and specificity compared to other EDX studies: multiple median F-wave parameters, median motor nerve residual latency, and sympathetic skin response (Technique K). 2. Investigational studies: evaluation of the effect on median NCS of limb ischemia, dynamic hand exercises, and brief or sustained wrist positioning.
RECOMMENDATIONS FOR FUTURE RESEARCH STUDIES IN CTS
The AAEM recommends that future clinical research studies of the usefulness of EDX studies to confirm the diagnosis of CTS meet three clinical study criteria:
1. Prospective study. 2. Clinical diagnosis of CTS independent of EDX studies. For example, a diagnosis of probable CTS as defined in the second CTS Literature Review2 which is based on a consensus recommendation by Rempel and colleagues.6 3. A uniform protocol for data collection and measurement with the physicians performing and interpreting the EDX studies under investigation blinded to the clinical diagnosis of all the human subjects (normal, CTS, disease control) in the study at least until the data collection and measurements are completed.
The AANEM recommends that future clinical research studies of the usefulness of EDX studies to confirm the diagnosis of CTS meet four additional methodological study criteria:
1. Description of EDX technique sufficient to permit replication of the study. 2. Monitor limb temperature continuously during the EDX study. 3. Normal values for EDX technique obtained with concomitant studies or with previous studies in the same laboratory. 4. Criteria of EDX abnormality obtained from normal population and defined in statistical terms.
The first and second AAEM CTS Literature Reviews1,2 used six CTS LIC. The second CTS Literature Review2 recommends (1) the addition of criterion 3, and (2) that future AAEM CTS Literature Reviews use all seven CTS LIC to review reports of the usefulness of EDX studies in the evaluation of CTS patients. The second AAEM CTS Literature Review2 also provides a set of specific criteria to make a clinical diagnosis of CTS based on expert opinion.
Both the first and second AAEM CTS Literature Reviews recommend that outcome studies should be performed to assess the harms, benefits, and costs of performing NCSs and needle EMG in patients with symptoms suggestive of CTS.
The AAEM CTS Task Force has addressed future research principles over future research topics (except for outcome studies) because the Task Force concluded that future research studies need to meet these principles (1) to provide reliable and reproducible data to evaluate the usefulness of EDX studies to confirm the clinical diagnosis of CTS, and (2) to permit comparison of the relative utility of different EDX studies for that purpose.
DISCLAIMER
This report is provided as an educational service of the AAEM, AAN, and AAPM&R. It is based on an assessment of the current scientific and clinical information. It is not intended to include all possible methods of care of a particular clinical problem, or all legitimate criteria for choosing to use a specific procedure. Neither is it intended to exclude any reasonable alternative methodologies. The AAEM recognizes that specific patient care decisions are the prerogative of the patient and his/her physician and are based on all of the circumstances involved.
ABSTRACT: The first AAEM Carpal Tunnel Syndrome (CTS) Literature Review (1993) evaluated the sensitivity and specificity of nerve conduction studies (NCSs) and needle electromyography (EMG) to confirm a clinical diagnoses of (CTS) based upon a critical review of 165 articles from the literature through May 1991. This new report includes all of the information from the first review and 113 additional articles from the literature through December 2000. The authors concluded that median sensory and motor NCSs are valid and reproducible clinical laboratory studies that confirm the clinical diagnoses of CTS with a high degree of sensitivity (>85%) and specificity (>95%) and that the clinical practice recommendations published in 1993 remain valid. Needle EMG studies were not as sensitive or specific as NCSs to diagnose CTS although they are useful to document axonal nerve pathology. In future research studies to evaluate the usefulness of NCSs and needle EMGs to diagnose CTS, the authors recommend that (1) the physician performing and interpreting the NCS and needle EMGs be blinded to the diagnosis of the subjects (normal, CTS patient, or disease control) to avoid observer bias and (2) the clinical diagnosis of CTS be made according to a new set of consensus clinical diagnostic criteria presented in this report to provide a more uniform population of CTS patients.
SECOND AAEM LITERATURE REVIEW OF THE USEFULNESS OF NERVE
CONDUCTION STUDIES AND NEEDLE ELECTROMYOGRAPHY FOR THE EVALUATION OF PATIENTS WITH CARPAL TUNNEL SYNDROME
Charles K. Jablecki MD, Michael T. Andary, MD, MS, Mary Kay Floeter, MD, PhD, Robert G. Miller, MD,
Caroline A. Quartly, MD, FRCP(C) Michael J. Vennix, MD, John R. Wilson, MD
Most physicians agree that the accuracy of the diagnoses and the care and management of patients with symptoms and signs of CTS are improved by the performance of EDX studies which increases the likelihood of the correct diagnosis of CTS.20,29,55,56,95,139,205 Those physicians believe that a definite diagnosis of CTS cannot be based solely on subjective complaints (e.g., pain, paresthesia), subjective findings, (e.g., Tinel’s sign, Phalen’s sign, sensory deficit) and voluntary effort (e.g., weakness) because there are other common disorders (e.g., cervical radiculopathy, tendonitis) which have similar signs and symptoms or that may coexist with CTS. In addition, there is a high incidence (20% or greater) of Tinel’s sign and Phalen’s sign in normal subjects.227,230,246 The accuracy of the diagnosis of CTS is important because the diagnosis often leads to surgical release of the carpal ligament in patients whose symptoms are refractory to non-operative therapy. If the symptoms are not due to CTS, then the patient is unlikely to benefit from surgery.
This review was developed for the AAEM by the CTS Task Force the members of which are listed as the authors of this review. The 1993 document was developed by the members of the AAEM Quality Assurance Committee: Chair Charles K. Jablecki, MD; Members: Michael T. Andary, MD, MS; Yuen T. So, MD, PhD; Dennis E. Wilkins, MD; and Faren H. Williams, MD.
Key Words: carpal tunnel syndrome • diagnosis • neural conduction • electromyography • literature review • reference values • sensitivity • specificity
Address correspondence to CK. Jablecki;, jablecki@post.harvard.edu
To purchase the document contact AAEM; aaem@aaem.net.
The sensitivity and specificity of nerve conduction studies (NCSs) and needle electromyography (EMG) for the diagnosis of CTS were evaluated by a critical review of the medical literature
published in 1993.109 The 1993 CTS Literature Review109 provided the evidence base for the Practice Parameters for Electrodiagnostic Studies in CTS7 which was endorsed by the American Association of Electrodiagnostic
Medicine (AAEM), the American Academy of Neurology (AAN), and the American Academy of Physical Medicine and Rehabilitation (AAPMR). Furthermore, the recommendation that future clinical research studies should meet the 6 AAEM CTS literature classification
criteria (hereafter referred to as the literature inclusion criteria [LIC]) published in 1993 has been described as a goal of several subsequent studies of EDX tests in CTS.59,75,91,140,188,189,221,237,254
In the
1993 report, it was recommended that the report be reviewed and updated periodically. The AAEM formed a Practice Parameter: Carpal Tunnel Syndrome second CTS Task Force in 2000 to update the 1993 report and to provide a single reference
for EDX studies in CTS by including the information from the 1993 publication along with the additional information from a systematic review of articles published in English through December 2000.
Based on a systematic review of the literature,
this document addresses the following key clinical questions:
1. In patients clinically suspected of having CTS, what are the best EDX studies to confirm the diagnosis? 2. What improvements can be made to future clinical research studies to evaluate the usefulness of laboratory studies, including EDX studies, to confirm the diagnosis of CTS?
CTS LIC to update this report. The first 2 criteria apply to all studies of diagnostic tests and deal with the quality of evidence and reducing bias; the remaining 4 criteria deal with technical and analytic issues
that are critical to the use of NCS to document nerve pathology. All of these criteria are important for a study to determine whether or not an NCS is useful to diagnose CTS.
1. Prospective study design. A prospective study design permits uniform collection and analysis of data. 2. Diagnosis of CTS in patient population based on clinical criteria independent of the EDX procedure under evaluation. Use of clinical criteria for the diagnosis of CTS permits identification of a defined population in which to test the sensitivity
of the EDX procedure to confirm the diagnosis of CTS. The clinical criteria include a history of nocturnal and activity-related pain and paresthesia in the affected hand, reproduction of the paresthesia with maneuvers that stress the median
nerve in the carpal tunnel (Phalen’s sign/wrist flexion, reverse Phalen’s sign/wrist extension, Tinel’s sign/percussion of the wrist, carpal tunnel compression test), sensory deficit limited to the distribution of the
median nerve passing through the carpal tunnel, and weakness and/or atrophy limited to the median innervated muscles in the thenar eminence.1,12,244 3. EDX procedure described in sufficient detail to permit replication of the procedure. Specific details of the EDX procedure are necessary (1) to verify the results and (2) to use the procedure in other clinical laboratories. 4. Limb temperature monitored (measured continuously) during nerve conduction procedures and minimum (or range) of limb temperatures reported for both CTS patients and the reference population. The speed of sensory and motor nerve conduction
is temperature dependent. The use of temperature correction factors to adjust nerve conduction velocity (CV) measurements made in cool limbs of CTS patients to a reference temperature is controversial and not recommended.10,14,18 5. Reference values for the EDX test obtained either a. with concomitant studies of a reference population, or b. with previous studies of a reference population in the same laboratory. The results of the EDX procedure in a reference population are necessary to determine the specificity of the results of the EDX procedure in CTS
patients.
6. Criteria for abnormal findings clearly stated and, if the measurement is a quantitative one, the abnormal value is defined in statistically computed terms, e.g., range and mean ± 2 standard deviations, from data derived from the reference
population. Use of standard statistical terms permits computation of the sensitivity and specificity of the EDX procedure and comparison of the procedure to other EDX and non-EDX tests for CTS.
EDX studies of only normal subjects could meet a maximum of 5 of the 6 AAEM CTS LIC because these studies do not contain CTS patients (criterion 2).
Table 1. Literature Classification of EDX Studies. Normal Subjects and Patients W ith CTS 6 of 6 Literature Inclusion Criteria Met Surface Electrodes Subdermal Electrodes Carroll38 Kimura130 Scelsa and colleagues221 Buchthal and colleagues31 Casey and LeQuesne39 Kuntzer140 Sener223 Buchthal and Rosenfalck30 Cioni and colleagues47 Nathan and colleagues181 Simovic and colleagues237 Tackmann and colleagues248 Clifford and Israels48 Nathan and colleagues182 Uncini and colleagues254 DeLean57* Padua and colleagues188 Werner and colleagues262 Di Guglielmo and
colleagues59 Padua and colleagues189 Jackson and Clifford110 Rosecrance and colleagues213 5 of 6 Literature Inclusion Criteria Met Surface Electrodes Subdermal Electrodes Andary and colleagues9 Lew and colleagues145 Preston and colleagues200 Lauritzen and colleagues143 Felsenthal and Spindler71 Logigian and colleagues146 Robinson and colleagues211 Pease and colleagues193 Fitz and colleagues74 Loong and Seah148 Sander and colleagues220 Smith239 Hansson and Nilsson97 Marin and colleagues158 Seror228 Thomas252 Imaoka and colleagues106 Melvin and colleagues167 Shafshak and El-Hinawy231 Kimura128 Merchurt and colleagues168 Trojaborg and colleagues253 Kothari and colleagues135 Monga and colleagues174 Verghese and colleagues259 Lesser and colleagues144 Palliyath and Holden190 Wang and colleagues260 4 of 6 Literature Inclusion Criteria Met Surface Electrodes Subdermal Electrodes Chang and colleagues44 Kiernan and colleagues126 Rosen214 Plajal199 Charles and colleagues45 Kim127 Rosenberg215 Preswick202 Eisen and colleagues64 Kimura and Ayyar131 Rossi and colleagues216 Felsenthal69 Kraft137 Seror224 Felsenthal70 Macleod157 Seror226 Fisher and Hoffen73 Marinacci159 Seror229 Gilliatt and colleagues84 Melvin and colleagues166 Sheean and colleagues233 Gunnarsson and colleagues91 Mills171 Tackmann and Lehman249 Joynt117 Monga and Laidlow173 Uncini and colleagues255 Kabiraj and colleagues119 Pease and colleagues192 Valls-Solé and colleagues257 Kemble125 Pease and colleagues194 Normal Subjects Only 5 of 6 Literature Inclusion Criteria Met (criteria met: 1,3,4,5,6; criterion 2 relates to CTS patients only) Surface Electrodes Subdermal Electrodes Buschbacher32 Buschbacher35 Stetson and colleagues242 Nielsen185 Buschbacher33 Buschbacher36 Wiederholt265 Buschbacher34 Di Benedetto and colleagues58 * Surface electrodes for motor studies, subdermal needle electrodes for sensory studies.
The source of the articles reviewed in the 1993 report was a Medline search for literature in English from January 1, 1986, through May 1991. The Medical Subject Headings (MeSH) searched were (1) wrist injuries or wrist joint, (2)
nerve compression syndrome, and (3) CTS. The search generated 488 article titles with abstracts. Two AAEM 1991 to 1993 QA Committee members reviewed the abstracts. Of the 488 articles, 81 reports referred to electrodiagnosis and other laboratory
studies to evaluate CTS; these were reviewed. The bibliographies of the 81 reports were examined and an additional 78 reports published prior to 1986 were identified and reviewed. The AAEM QA Committee members and 12 additional AAEM members, who have
current research interests in CTS, were contacted to provide bibliographies of EDX studies in CTS. Six additional references were identified from these AAEM consultants. Of the total of 165 (81+78+6) articles reviewed, 20 were classified as background
references.
The source of the articles for this second report was a Medline search for literature in English through December 2000. The MeSH searched were CTS and diagnosis or carpal tunnel and neural conduction. The search generated 497 article titles
with abstracts published since 1990. Based on a review of the abstracts, the AAEM CTS Task Force chose 92 articles for review. An additional 5 articles were identified from the bibliographies of the articles and 16 from AAEM members who have current
research interests in CTS. Of the total of 113 (92+5+16) articles reviewed, 24 were classified as background references.
At the start of the second review process, the AAEM CTS LIC for limb temperature monitoring during an NCS was
clarified: the published paper must report the limb temperature was measured continuously during the NCS. To be certain that all of the papers reported in the second CTS Literature Review met this criterion, the papers reviewed for the first
CTS Literature Review were re-examined. As a result of the re-examination, there was no change in the classification of papers that previously met 6 of 6 AAEM CTS LIC; several papers that previously met 5/6 (9),50,113,125,157,161,162,171,202,204 4/6 (6),15,112,222,243,264,271 3/6 (4),62 ,88,114,134 and 1/6(1)111 were reclassified as not meeting the AAEM CTS LIC for limb temperature monitoring.
Tables were constructed to display the data from the articles that met all 6 AAEM CTS LIC unless the studies used subdermal (needle) stimulating and/or recording electrodes
for the NCS or the studies were considered to be investigational. Abstracts of articles that met 4, 5, or 6 AAEM CTS LIC or had historical interest are included in the references.
The tables describing the results of NCSs with surface
recording and stimulating electrodes were to include the following information:
1. Author: a. Publication date. 2. Control subjects: a. Number of control hands (number of control subjects). b. Mean (range) age of control subjects. 3. CTS Patients: a. Number of CTS hands (number of CTS patients). b. Mean (range) age of CTS patients. 4. Test parameters: a. Conduction distance in centimeters. b. Stimulation site. c. Recording site. 5. Range or minimum hand temperature. 6. Mean ± standard deviation of test results in normal hands. 7. Criteria for abnormal value, e.g., mean ± 2 standard deviations. 8. Abnormal value. 9. Specificity of the test defined as the percentage of normal hands with normal test results (calculated or actual). 10 Sensitivity of the test defined as the percentage of CTS hands with abnormal test results.
If an article chosen for a table did not contain all the data required for the table, the author(s) of the article were contacted to provide the missing information and the data was added to the table with a notation of the source as being
written communication.
131,148,199,243 3,110,117,118,167 this is
not always the case. Furthermore, damage to the median nerve fibers in the brachial plexus or proximal portions of the median nerve can produce changes in the amplitude of median nerve responses in the hand similar to changes caused by
damage to the median nerve fibers in the carpal tunnel.266 On the other hand, focal slowing or block of nerve conduction across the carpal tunnel has localizing pathologic significance.82,83 For this reason, the 1991 to 1993
AAEM QA Committee agreed to focus on the results of EDX techniques to measure the speed of median nerve conduction across the carpal tunnel in CTS rather than the results of techniques to measure the amplitude of median sensory and motor responses.
Since 1991, additional articles have been published which support that decision.26,32,33 This current report is more inclusive and contains new tables with data on median sensory and motor nerve amplitude changes in CTS patients from the
1991 to 2000 literature search to permit the reader to verify the conclusions of the AAEM CTS Task Force.
While reviewing the articles, it became clear that the selection criteria for the clinical diagnosis of CTS was not always described
in sufficient detail to determine whether the patient group was representative of the CTS population. In 1989, Jackson and Clifford110 demonstrated that the incidence of EDX abnormalities increased according to the severity of the median
nerve compression as determined by the clinical history of persistent sensory symptoms and the clinical findings of thenar muscle weakness and atrophy. Thus, selection of more advanced cases would increase the yield of EDX abnormalities. A report
by Buchthal and colleagues31 in 1974 illustrated this point because they reported a 91% incidence of abnormal findings on the needle EMG examination of the abductor pollicis brevis (APB) muscle in CTS patients. Subsequent studies of needle
EMG findings in CTS243 and the consensus of members of the 1991 to 1993 AAEM QA Committee and the AAEM CTS Task Force was that the incidence of abnormal needle EMG findings in the thenar muscles of CTS patients is much less than were reported
by Buchthal and colleagues31 whose studies were conducted at a national clinical research center.
To balance the authority of a publication meeting the 6 AAEM CTS LIC in a controlled academic setting with the reality of
clinical experience, the 1991 to 1993 QA Committee decided to report data in tables only if the maximum incidence of any EDX abnormality in all the CTS patients in the study was less than 90%. If over 90% of the patients with a clinical diagnosis
of CTS demonstrate a test abnormality, the results suggest that the patient population was heavily screened and, therefore, biased with patients with advanced CTS. For this reason, the studies of Casey and LeQuesne39 and Cioni and colleagues,47 which
met the 6 literature classification criteria, were not included in the table data of the 1993 publication. This convention was eliminated from the current review. Data from all studies that met 6 AAEM CTS LIC are displayed in tables regardless of
how high or low the sensitivity and specificity of the test results so readers can draw their own conclusions.
The AAEM CTS Task Force identified 2 possible sources of investigator bias in the CTS literature: selection bias and observer
bias.
Selection bias might increase the incidence of EDX test abnormalities due to inclusion of CTS patients with more severe CTS than usually encountered in a clinical practice. To address prospectively the issue of selection bias in
CTS research studies as described above, the AAEM CTS Task Force developed a set of criteria for the clinical diagnosis of CTS to provide a more uniform population of CTS patients for use in future research studies of the usefulness of EDX studies
to diagnose CTS (see Table 2).
Observer bias might increase the incidence of EDX test abnormalities due to the desire of the researcher to document the usefulness of the EDX test. To address prospectively the issue of observer bias,
Sackett and colleagues217 have recommended that clinical research studies of diagnostic tests be performed with the physician performing and interpreting the diagnostic tests blinded to the diagnosis of the subject. At the recommendation
of the AAN, the AAEM recently endorsed that principle and recommends that physicians performing and interpreting the EDX test as part of a clinical research study be blinded to the clinical classification of the research subjects (normal, CTS, disease
control).
In 1949,
Dawson and Scott54 reported the reproducible recording of nerve action potentials with surface electrodes in arms of healthy human subjects after electric stimulation of the nerves and suggested that the technique may be useful in detecting
nerve damage. In 1956, Simpson238 reported the observation that the median motor distal latency was prolonged across the carpal tunnel in CTS and this was confirmed by other investigators: Thomas252 in 1960 and Lambert141 in
1962. In 1956, Dawson53 described a technique for measuring median sensory nerve conduction across the carpal tunnel. In 1958, Gilliatt and Sears85 demonstrated slow median sensory nerve conduction across the carpal tunnel in
patients with CTS. Casey and LeQuesne39 confirmed the finding of Buchthal and Rosenfalck30 that the median nerve conduction abnormalities in CTS were focal and localized to the segment of the median nerve in the carpal tunnel.
Brown
28 confirmed the localization of the median nerve conduction abnormalities in CTS patients to be under the carpal ligament with intraoperative NCSs. Other studies have verified these reports and median sensory and motor NCSs have become
the mainstay for the laboratory evaluation of CTS.243
Over the past 40 years, clinical research efforts have refined the techniques of median sensory and motor NCSs across the carpal tunnel to make
the tests more sensitive and specific for the detection of compression of the median nerve in the carpal tunnel.110,181 To make the NCSs more sensitive, investigators have developed techniques to exclude the normal segment of the median
nerve distal to the flexor retinaculum of the carpal tunnel,30,52,59,65,104,143,265 compared the speed of median nerve conduction to the speed of ulnar or radial nerve conduction from the same hand,31,200,216,220,233,253 performed sequential short segment (1 cm) sensory and motor NCSs,106,132,224 ,226 and compared the median nerve conduction across the carpal tunnel to median nerve conduction in the forearm or digit.131,188,189,236,237 Table 2. Clinical Diagnostic Criteria for CTS Research. To assist in the research evaluation of EDX studies to confirm the clinical diagnosis of CTS, the following criteria are provided to make a clinical diagnosis of CTS. The criteria are based on symptoms alone; the findings on the physical
examination are not necessary for the clinical diagnosis of CTS.205 The findings on the physical examination should be used with the medical history to diagnose (1) alternative causes of the sensory symptoms in the hand(s)
and (2) concomitant disorders that may confound the laboratory diagnosis of CTS. This document incorporates criteria originally proposed by the AAN Quality Standards Subcommittee in 1993.1 Note that the first inclusion criterion
is based on the presence of numbness and tingling, not pain, because numbness and tingling are more specific for nerve injury whereas pain is commonly found in soft-tissue injuries and musculoskeletal disorders in addition to CTS.272 The terms “numbness and tingling” were chosen over the term “paresthesia” because the terms “numbness and tingling” are generally understood by patients and the term “paresthesia” is
foreign to most patients.
INCLUSION CRITERIA
EXCLUSION CRITERIA
CERTAINTY DIAGNOSIS OF CTS FOR RESEARCH STUDIES
It is recommended that clinical research studies use a combination of clinical and EDX findings to define the highest level of certainty (definite) of the diagnosis of carpal tunnel syndrome, while clinical
criteria alone are used to define probable and possible CTS as follows:
Definite CTS: Patients (1) satisfy all inclusion and exclusion criteria, and (2) have nerve conduction
abnormalities consistent with pathology exclusive to the median nerve and localized in the carpal tunnel segment of the median nerve.
Probable CTS: Patients satisfy all clinical inclusion and exclusion
criteria.
USE OF CLINICAL DIAGNOSTIC CRITERIA FOR CTS RESEARCH
To evaluate the specificity of NCSs for the diagnosis of CTS, investigators have used clinical criteria for the diagnosis of CTS independent of EDX findings, performed prospective studies, and included concomitant evaluation of normal
control subjects.110 The results of these clinical research efforts have found rapid application in the clinical laboratory. Physicians in several specialties, including neurology, physical medicine and rehabilitation, orthopaedics, neurosurgery,
plastic surgery, rheumatology, and occupational medicine have concluded that NCSs and needle EMG are of value for the laboratory diagnosis of CTS.77,80,110,121,243 In a multidiscipline consensus forum, Rempel and colleagues205 concluded
that NCSs, combined with the clinical history and clinical findings, provide a better basis for the diagnosis of CTS than the clinical history and clinical finding alone.
Several investigators have studied the relationship between the abnormalities on NCSs and the duration and severity of symptoms and signs of CTS. Patients with weakness and/or sensory deficits frequently have low amplitude motor and/or sensory
potentials, respectively.85,251 Although the incidence of abnormalities of median sensory and motor conduction is greater when the duration of the symptoms of CTS is longer, there are definite exceptions.251 Furthermore, in 1963,
Fullerton
76 demonstrated that the susceptibility of median motor nerve conduction across the wrist to ischemia correlated with the frequency and severity of intermittent attacks of pain and paresthesias in the affected hand; slowing of motor nerve
conduction (prolonged distal latency) did not correlate with pain and paresthesias. Fullerton76 suggested that there were 2 mechanisms responsible for the symptoms and signs of CTS: (1) a rapidly reversible change in the nerve fibers associated
with ischemic attacks, and (2) a slowly developing structural change in the nerve fibers resulting from pressure on the nerve under the flexor retinaculum. In 1980, Gilliatt82 reviewed additional evidence to support Fullerton’s hypothesis
which provides an explanation for the prompt relief of some symptoms of CTS with surgical decompression of the carpal tunnel.
Motor and sensory NCSs can be performed in the clinical laboratory setting with surface stimulating and
recording electrodes.85,141,252 The technical factors that influence the results of these studies have been identified to include the following: amplifier gain and filter settings; electrode size, shape, and material; distance between stimulating
and recording electrodes; distance between recording electrodes; and limb temperature. Pathologic conditions which cause nerve damage also alter the results of NCSs by slowing or blocking nerve conduction. NCSs provide a unique and reliable method
for assessing directly the integrity of sensory and motor nerve fibers.82,83
Needle EMG is performed by inserting a sterile needle Practice Parameter: Carpal Tunnel Syndrome
electrode through
the skin into the belly of a muscle and evaluating the spontaneous and voluntary electrical activity in the muscle. The technical factors that influence the results of these studies have been identified and include amplifier gain and filter settings
and electrode size, shape, and material. After injury of a nerve to a muscle, abnormal electrical activity can be recorded in the muscle, which serves to provide objective evidence of motor nerve injury.
NCSs and needle EMG are complementary
but distinctly different EDX techniques although they are often performed sequentially for the evaluation of clinical problems. Because the use of NCSs and needle EMG requires (1) the formulation of a differential diagnosis based on the clinical history
and physical examination, (2) interpretation of the data during the examination, and (3) a change in the direction of the examination during the study based upon that interpretation integrated with clinical information, NCSs and EMG are the practice
of medicine and should be performed by a physician qualified by education, training, and experience.6
A total of 22 of the 320 articles
and abstracts reviewed met all 6 AAEM CTS LIC (see Table 1) and 16 of these 22 articles were selected as the source of the data displayed in Tables 3 through 22.38,39,47,57,59,110,130,140,181,182,188,189,221,223,237 ,254
The
16 articles selected for the tables: (1) met all 6 CTS LIC, (2) used surface recording electrodes for NCSs, (3) used a technique that evaluated median nerve conduction with the wrist in a neutral position and the hand in a rested state, and (4) reported
median nerve conduction abnormalities in a total of 1812 CTS patients and a total of 678 normal subjects. The data from the remaining 6 articles are discussed in the text but were not used as a source of Table data30,31,48,213,248,262 because: (1)
3 investigators30,31,248 used subdermal needle electrodes for stimulating and/or recording electrodes for all of the NCSs (1 used needle recording electrodes for the median sensory NCS and surface electrodes for the median motor NCS29),
and needle electrodes are not generally used for NCS,239 and (2) 3 additional articles48,213,262 reported the effect of wrist positioning and/or hand movements on median NCS and these studies are best viewed as investigational
techniques since there is conflicting information on their usefulness to diagnose CTS.
There were 9 additional articles listed in Table 1 (8 using surface electrodes and 1 using needle electrodes) that studied median motor and sensory nerve conduction across the carpal tunnel (amplitude, latency, and velocity) in normal subjects
only and otherwise fulfilled the AAEM CTS LIC. The 9 articles are referenced in the text that accompanies the appropriate numbered tables. The 8 articles that used surface electrodes provide measurements of median nerve conduction in a total of 425
normal subjects.
There were 21 studies
of the median motor distal latency in CTS that met 4 or 5 of the 6 AAEM CTS LIC with the following incidence of prolonged median motor distal latency measurements in CTS: Rosen214 (1993), 20%; Macleod157 (1987), 29%; Mills171 (1985), 33%; Kothari135 (1995), 33%; Gunnarsson91 (1997), 37%; White and colleagues264 (1988), 46%; Preston and Logigian200 (1992), 54%; Seror228 (1994), 55%, Kimura and Ayyar83 (1985),
56%; Trojaborg and colleagues253 (1996), 60%; Preswick202 (1963), 62%; Thomas252 (1960), 63%; Bhala and Thoppil15 (1981), 67%; Merchut and colleagues168 (1990), 68%; Kemble125 (1968), 69%; Marinacci159 (1964), 69%; Fitz74 (1990), 72%; Sheean and colleagues233 (1995), 78%; Melvin and colleagues167 (1973), 79%; Schwartz and colleagues222 (1980), 80%; Monga and colleagues174 (1985), 81%. Interestingly, the median motor conduction may be slightly slowed in the forearm segment above the carpal tunnel in CTS when the median motor distal latency is prolonged.131,194,252 The cause of the slowing of median motor
conduction in the forearm of CTS patients is not clear. Chang43,44 provided evidence that the slowing is due to retrograde degeneration of median motor nerve fibers in the forearm segment of the median nerve. However, Wilson268 provided evidence that the measured slowing is due to the block of conduction of the faster conducting fibers at the wrist.
Median Motor Nerve Conduction between Wrist and Palm. Table 4 presents the results of 2 studies
that met 6 AAEM CTS LIC and calculated the median motor CV over a short conduction distance (5 cm to 6 cm) between the wrist and palm stimulation sites.59,130 Compared to the studies in Table 3 of median distal motor latency, the calculated
median motor CV across the carpal tunnel was a more sensitive test for CTS.
Median Motor Nerve Compound Muscle Action Potential Amplitude. Table 5 presents the results of a study of median motor nerve compound muscle action
potential (CMAP) amplitude changes in CTS by Kuntzer140 that met all 6 AAEM CTS LIC. The study demonstrated that measurements of median motor distal latency is more often abnormal in CTS patients than the measurement of median motor CMAP
amplitude, 47% versus 15% (compare Table 3 and Table 5). The criterion of abnormality (mean –2 standard deviation [SD]) chosen by Kuntzer140 (1994) of the CMAP <5 mV lies between the mean –2 SD of 2 studies of normal subjects
that met 5 of the 6 AAEM CTS LIC: the mean ± SD for the thenar CMAP was 10.2 ± 3.6 mV, mean –2 SD = 3.0 mV (Buschbacher34) and 12.5 ± 3.1 mV, mean –2 SD = 6.3 mV
(Stetson242 )
Median Motor Nerve Wrist to Palm CMAP Amplitude Ratio. The ratio of the amplitude of the median motor CMAP recorded over the APB with (1) stimulation of the median nerve at the wrist and (2) stimulation in the palm makes it possible to
identify median motor nerve conduction block across the carpal tunnel. The technique is technically difficult because it is necessary to take steps to avoid simultaneous stimulation of the ulnar nerve in the palm which, if undetected, results in a
factitious increase in the APB CMAP with palm stimulation compared to the APB CMAP with wrist stimulation (Di Guglielmo59). Pease193 and Gordon89 evaluated this technique for the diagnosis of CTS and the results were
inconclusive.
Table 6 presents the results of the study by Di Guglielmo59 that met all 6 AAEM CTS LIC; the incidence of motor conduction block was low (7%) with the criteria of a greater than 30% reduction in CMAP amplitude with less
than a 15% increase in the duration of the proximal CMAP, criteria which take into account temporal dispersion and phase cancellation. Lesser and colleagues,144 in a study that met 5 of the 6 AAEM CTS LIC, reported that a higher incidence
of abnormalities (39% of CTS patients showed evidence of motor conduction block across the carpal tunnel) but did not provide data on temporal dispersion and phase cancellation which would give the appearance of conduction block (Di Guglielmo).59
Table 3. Median Motor Nerve Distal Latency in CTS. Author DeLean57 Jackson and
Clifford110Kimura130 Padua and colleagues188 Padua and colleagues189 Kuntzer140 Cioni and colleagues47 Year 1988 1989 1979 1996 1997* 1994 1989 Number of
Normal Hands
(subjects) 80 (43) 38 (38) 122 (61) 40 (36) 70 (70)† 56 (54) Normal
Subject’s Age:
Mean (range) 33 (20 to
73)42 (21 to 69) 43 (15 to 60) 44 (19 to 79) 43 (25 to 70) 38 (18 to 68) Number of CTS
Hands (patients) 253 (150) 131 (123) 172 (105) 50 (43) 500 (379) 100 (100)† 375 (370) CTS Subjects
Age: Mean
(range) 47 (20 to
84)53 (21 to 85) 48 (20 to 78) 45 (23 to 80) 51 (20 to 88) 51 (26 to 85) 46 (20 to 72) Technique:
Conduction
Distance 6 cm to 8 cm 8 cm Anatomical landmarks 6 cm to 8 cm‡ Anatomical landmarks 6 cm Stimulation Site Wrist Wrist 3 cm proximal to wrist crease Wrist Distal wrist crease Wrist Recording Site APB APB APB APB APB APB Minimum Hand
Temperature 32°C 31°C 34°C 31°C 32°C 33°C Median Motor
Distal Latency ±
SD3.2 ± 0.4 ms 3.18 ± 0.27 ms 3.60 ± 0.36 ms 3.2 ± 0.4 ms§ 3.66 ± 0.38 ms 3.3 ± 0.5 ms Criteria for
Abnormal Value Mean + 2
SDMean + 2 SD Mean + 2
SDMean + 2 SD Mean + 2 SD Mean + 2 SD Abnormal Value >4.2 ms >3.71 ms >4.4 ms 3.2 ± 0.4 ms§ >4.5 ms >4.3 ms Specificity of
Abnormal Value 99%
(estimate)95%‡
(actual)97.5%
(estimate)97.5% (estimate) 98.6%
(actual)97.5%
(estimate)Sensitivity of
Abnormal Value 60% 74%‡ 61% 44% 55% 47% 80% The median nerve motor conduction studies cited in Table 3 were performed by fastening surface recording electrodes over the thenar eminence (G1 or E1) and thumb (G2 or E2) and supramaximal stimulation of the median nerve with surface
electrodes above the wrist crease. With these anatomic landmarks, the conduction distance is usually 6 to 8 cm in normal adults. The time (latency) from the stimulus artifact to the initial negative deflection of the compound muscle
action potential (CMAP) was measured in ms and recorded as the median motor distal latency (MDL). Slowing of median motor nerve conduction in the carpal tunnel with nerve injury will result in prolongation of the median MDL. Because
cooling of the nerve fibers and increasing the conduction distance also result in prolongation of the median nerve MDL, it is important that the limb temperature and the conduction distance be controlled.
* 1997 Padua and colleagues
paper
189 cites reference population studies performed in the same laboratory in 1996.188 † For each reference subject, only one hand was tested; for each CTS patient, only the most symptomatic hand was tested.
‡ Written communication.
§ Written communication: the SD of the normal value was misprinted in the 1996 paper, Table 1 (page 50), 3.2 ± 0.8 ms, and should have been 0.4 ms. The abnormal value (4.0 ms) was published
correctly.Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
APB = Abductor Pollicis Brevis CTS = Carpal Tunnel Syndrome SD = Standard Deviation Table 4. Median Motor Nerve Conduction Between Wrist and Palm in CTS. Author Kimura130 Di Guglielmo and colleagues59 Year 1979 1997 Number of Normal Hands (subjects) 122 (61) 88 (69) Normal Subject’s
Age: Mean (range) 43 (15 to 60) 40 (20 to 86) Number of CTS
Hands (patients) 172 (105) 294 (198) CTS Subjects Age: Mean (range) 48 (20 to 78) 46 (13 to 84) Technique Anatomical landmarks Anatomical landmarks Proximal Stimulation Site Wrist crease 1-2 cm proximal to wrist crease Distal Stimulation Site Palm 3 cm distal to wrist crease Recording Site APB APB Minimum Hand
Temperature 34°C 32°C Median Motor CV ±
SD49.0 ± 5.7 46.7 ± 5.8 Criteria for Abnormal Value Mean – 2 SD Mean – 2 SD Abnormal Value <38 m/s <35 m/s Specificity of
Abnormal Value 97.5%
(estimate)97.5% (estimate) Sensitivity of
Abnormal Value 84% 23% (61%)* * In the Di Guglielmo and colleagues paper,59 measurement of median motor conduction in the carpal tunnel segment was performed only in
146 CTS hands with normal median sensory conduction from wrist to D2 (SCV >45 m/s)
and normal median motor distal latency (<4.2 ms). Therefore, the percentage (33/146 = 23%) of abnormal median motor conduction across the carpal tunnel segment was reported for a subset of all the CTS hands. From the data in the
paper, the maximum possible percentage of abnormal median motor conduction in the carpal tunnel segment for all the CTS hands was calculated to be 61%.Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
CTS = Carpal Tunnel Syndrome CV = Conduction Velocity SD = Standard Deviation APB = Abductor Pollicis Brevis
SCV =
Sensory Conduction Velocity
Median Motor Short-segment Incremental Studies. Kimura128,130 performed short-segment incremental stimulation of the median nerve across the carpal tunnel at 1-cm intervals and noted that, unlike the median sensory nerve fibers
(see below), the median motor nerve fibers are difficult to activate sequentially in steps of 1 cm because of the recurrent course of the motor branch of the median nerve to the thenar muscle and the proximity of the stimulating electrodes to the
thenar muscle. The technique can be time consuming because it is often difficult to eliminate the stimulus artifact from therecording.128,130,243 In addition, it is difficult to choose a limit for normal results that provide both sensitivity
and specificity. For example,although White and colleagues264 in 1988 reported a very high test sensitivity (89% in mild CTS), the same authors reported a very high incidence (72%) of abnormalities in asymptomatic hands, which suggests
that this test has an unacceptable high rate of false positive results. For these reasons, the technique of segmental (1 cm) median motor nerve stimulation has not been widely accepted for evaluation of patients with CTS. Table 5. Median Motor Nerve CMAP Amplitude in
CTS.Author Kuntzer140 Year 1994 Number of Normal Hands
(subjects) 70 (70)* Normal Subject’s Age: Mean (range) 43 (25 to 70) Number of CTS hands (patients) 100 (100)* Normal Subject’s Age: Mean (range) 51 (26 to 85) Stimulation Site Wrist Recording Site APB Minimum Hand Temperature 32°C Normal CMAP amplitude ± SD 7.8 ± 1.4 mV Criteria for Abnormal Value Mean – 2 SD Abnormal Value <5 mV Specificity of Abnormal Value 100% (actual) Sensitivity of Abnormal Value 15% * For each reference subject, only 1 hand was tested; for each CTS patient, only the most symptomatic hand was tested. Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
APB = Abductor Pollicis Brevis CTS = Carpal Tunnel Syndrome
CMAP = Compound Muscle Action Potential SD = Standard Deviation
Table 6. Median Motor Nerve CMAP Wrist to Palm Amplitude Ratio in CTS. Author Di Guglielmo and colleagues59 Year 1997 Number of Normal Hands
(subjects) 88 (69) Normal Subject’s Age: Mean (range) 40 (20 to 86) Number of CTS Hands (subjects) 294 (198) CTS Subjects Age: Mean (range) 46 (13 to 84) Technique: Conduction
Distance Anatomical landmarks Wrist Stimulation Site 1 cm to 2 cm proximal to wrist crease Palm Stimulation Site 3 cm distal to wrist crease Recording Site APB Minimum Temperature 32°C Amplitude (wrist) ± SD 10.2 ± 2.9 mV Amplitude (palm) ± SD 10.5 ± 2.9 mV Wrist to palm amplitude ratio ± SD 0.9 ± 0.1 Abnormal Value <0.7 Criteria for Abnormal Value Lowest value of range of normal values* Specificity of Abnormal Value 100% (actual) Sensitivity of Abnormal Value 7% * Written communication. Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
ABP = Abductor Pollicis Brevis CMAP = Compound Muscle
Action Potential CTS = Carpal Tunnel Syndrome SD = Standard Deviation
The Martin-Gruber anomaly does not affect the measurement of the median motor distal latency with stimulation of the median nerve at the wrist.243 If
the median nerve conduction in the carpal tunnel is sufficiently slower than the ulnar nerve conduction at the wrist, then stimulation of the median nerve at the elbow in the presence of the Martin-Gruber median to ulnar anastomosis in the forearm
may result in 2 temporally separate CMAPs recorded over the thenar muscle, the normal ulnar response and delayed median response.92,93,129 More often the occurrence of CTS in a patient with an underlying Martin-Gruber anastomosis results
in (1) a change in the waveform of the thenar muscle action potential with proximal median nerve stimulation (initial positive deflection and increased amplitude) compared to distal median nerve stimulation (initial negative deflection)93 and
(2) an erroneously fast median nerve forearm CV measurement.129,267 Gutmann92,93 suggested that the presence of an initial positive deflection of the CMAP recorded over the thenar muscle with stimulation of the median nerve
at the elbow which was not present with stimulation of the median nerve at the wrist was evidence of median nerve pathology at the wrist. However, more proximal median nerve pathology in the forearm could result in the same phenomenon.
Comparison of Distal Median Nerve Conduction to Proximal Median Nerve Conduction. Investigators have recommended formulae (residual latency [RL] and terminal latency index [TLI]) to permit comparison of distal median nerve conduction
through the carpal tunnel to more proximal median nerve conduction through the forearm with the goal of eliminating intersubject variability of motor nerve conduction and thereby improving the diagnostic usefulness of motor NCSs to diagnose CTS.137,232
Median Motor Nerve RL. Kraft and Halvorson137 proposed the concept and formula for RL measurements. The RL is equal to the difference between the measured distal latency and the predicted distal latency, the latter
computed as the quotient of the distal conduction distance and the proximal CV of the same nerve. Kuntzer,140 in a report that met 6 AAEM CTS LIC, confirmed that the measurements of median motor RL is more often abnormal in CTS patients
than the measurement of median motor distal latency, 64% Practice Parameter: Carpal Tunnel Syndrome
versus 47%, but with lower specificity, 89% versus 99% (Table 7 and Table 3). The latter results suggest that if the criteria for
an abnormal RL were adjusted for comparable specificity, that the increased incidence of abnormalities would fall. Evidence to support this conclusion is found in the study by Trojaborg,253 which met 5 of the 6 AAEM CTS LIC. Trojaborg253 noted
a lower incidence of abnormal RL values (48%) compared to abnormal distal latency values (60%) in CTS patients with comparable specificity and that the RL was normal in CTS patients with normal median motor distal latencies. The interested reader
is also referred to studies of median motor nerve RL previously reviewed in the 1993 AAEM CTS Literature Review.66,116,137,204
Median Nerve Terminal Latency Index. Simovic and Weinberg236,237 provide
a summary of the reported studies on the usefulness of the median motor TLI to diagnose CTS. In 1979, Shahani described the potential usefulness of the TLI ratio to diagnose CTS. In 1988, Lissens reported similar findings in the Dutch literature.
The TLI is calculated from the conventional median motor NCS measurements that adjusts the median motor distal latency for the terminal motor conduction distance and the proximal median motor nerve CV. The TLI is calculated as follows: terminal
conduction distance / [proximal CV × distal latency]. The ratio decreases as the conduction time increases across the carpal tunnel.
Table 8 presents the results of 2 studies of the TLI that met 6 AAEM CTS LIC. The study by Simovic
and Weinberg237 concluded that 81.5% of CTS patients demonstrate a TLI less than 0.34. However, Donahue and colleagues60 noted that the presence of the Martin-Gruber anastomosis in CTS patients could create an artificially
high median motor forearm CV measurement. The study by Kuntzer140 noted that 10% of the control group and 7% of the CTS group showed a median-to-ulnar crossover. Kuntzer140 excluded those normal subjects and CTS patients
from his analysis of the value of the TLI to identify CTS and noted that only 50% of the CTS group showed a TLI less than 0.34 with a specificity of 91%. Simovic and Weinberg237 provided a summary of the published normative data on
242 hands and noted that only 6 had a TLI under 0.34 to yield a specificity of 97.5%. These interesting findings need to be confirmed in other laboratories to determine the usefulness of the TLI to diagnose CTS.
Comparison of Median Motor Nerve Conduction to Ulnar Motor Nerve Conduction in the Same Limb. There
are 3 different published methods to confirm the diagnosis of CTS by calculating the difference between the median and ulnar nerve distal motor latencies: the median-thenar to ulnar-hypothenar latency difference (THLD),167 the medianthenar
to ulnar-thenar latency difference (TTLD),220 and the median-lumbrical to ulnar-interossei latency difference (LILD).146 These studies approach the sensitivity of median sensory NCSs in the diagnosis of CTS and may also
be useful in localizing median nerve pathology to the wrist (1) when the median sensory response is absent and (2) when CTS occurs in the presence of a polyneuropathy. 220,253Table 7. Median Motor Nerve RL in CTS. Author Kuntzer140 Year 1994 Number of Normal Hands
(subjects) 70 (70)* Normal Subject’s Age: Mean (range) 43 (25 to 70) Number CTS hands
(patients) 100 (100)* CTS Subject Age 51 (26 to 85) Technique: Conduction
Distance Anatomical landmarks Stimulation Site Distal wrist crease Recording Site APB Minimum Hand
Temperature 32°C Normal RL ± SD 1.96 ± 0.32 ms Criteria for Abnormal Value Mean + 2 SD Abnormal Values >2.6 ms Specificity of Abnormal
Value 88.5% (actual) Sensitivity of Abnormal
Value 64% * For each reference subject, only 1 hand was tested: for each CTS patient, only the most symptomatic hand was tested. Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
APB = Abductor Pollicis Brevis CTS = Carpal Tunnel Syndrome RL = Residual Latency SD = Standard Deviation
Median-Thenar to Ulnar-Hypothenar Latency Difference. The THLD method is straightforward and calculates the difference (THLD) between (1) the distal latency of the CMAP recorded over the APB with median nerve stimulation at the
wrist (thenar latency) and (2) the distal latency of the CMAP recorded over the abductor digiti minimi (ADM) with ulnar nerve stimulation at the wrist (hypothenar latency).167,220 There are no studies of this method that meet all 6
AAEM CTS LIC. In a study that met 5 of the 6 AAEM CTS LIC, Sander220 noted the sensitivity of the THLD study approached the sensitivity of median mixed nerve palmar studies for the diagnosis of CTS because 85% of CTS patients with
abnormal median mixed nerve palmar studies showed abnormal THLD. In a study that met 4 of the 6 AAEM CTS LIC, Rosen214 also noted that median mixed nerve palmar conduction studies (100%) were much more sensitive than THLD studies (36%).
Table 8. Median Motor Nerve Terminal Latency Index in CTS. Author Simovic and colleages237 Kuntzer140 Year 1999 1994 Number of Normal Hands (subjects) 38 (19) 63 (63)* Normal Subject’s Age: Mean (range) 40 (25 to 68) 45 (32 to 72)* Number of CTS Hands (patients) 54 (54) 93 (93)* CTS Subjects Age: Mean (range) 50 (18 to 86) 50 (35 to 85)* Technique Motor conduction study Motor conduction study Stimulation Site Wrist Wrist Stimulation Site Elbow Elbow Recording Site APB APB Minimum Hand Temperature 32°C 32°C Terminal Latency Index ± SD 0.43 ± 0.045 0.427 ± 0.043 Criteria for Abnormal Value Mean – 2 SD Mean – 2 SD Abnormal Value <0.34 <0.34 Specificity of Abnormal Value 97.5% (estimate) 91.4% (actual) Sensitivity of Abnormal Value 82% 50% * For each reference subject, only 1 hand was tested; for each CTS patient, only the most symptomatic hand was tested. Terminal latency index data from 7 (10%) of 70 normal subjects and 7 (7%) of the 100 CTS subjects were excluded because
of the presence of a median to ulnar crossover in the forearm and median nerve conduction velocity calculations may not be accurate in those cases. The crossover was identified by a compound muscle action potential with an initial
negative (upgoing) deflection recorded over the abductor digiti minimi (gain 200 µV/div) with median nerve stimulation at the elbow. The mean and range of the ages of the remaining 63 normal subjects and 93 CTS patients
were provided by the author by written communication. Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
APB = Abductor Pollicis Brevis CTS = Carpal Tunnel Syndrome SD = Standard Deviation
Median-Lumbrical to Ulnar-Interossei Latency Difference. The
LILD method is also unusual because the CMAP is recorded over the distal medial palm (active electrode Practice Parameter: Carpal Tunnel Syndrome place slightly
In a study that met all 6 AAEM CTS LIC, Uncini254 demonstrated that
the LILD identified a small number of additional CTS patients with normal median motor distal latency values (Table 9). Because Uncini254 did not simultaneously evaluate median mixed nerve palmar conduction studies in CTS patients, his
results are not inconsistent with the results of Sander220 which showed the median mixed nerve palmar conduction studies to be more sensitive than the THLD and TTLD studies to identify CTS patients.
There were 4 studies of the LILD
in CTS that met 4 or 5 of the 6 AAEM CTS LIC with the following incidence of abnormal LILD measurements in CTS: Sheean and colleagues233 (1995), 73%; Trojaborg253 (1996), 84%; Preston and Logigian200 (1992),
95%; and Resende207 (2000), 100%. Sheean and colleagues233 noted that the computation of the LILD was identical in sensitivity to computation of the difference in median and ulnar mixed nerve palmar CV to confirm
the diagnosis of CTS; in 48 of 66 hands with suspected CTS, 48 (72%) showed abnormalities with each test and there was a close correlation between the 2 tests.
Median F-Wave Latency Studies. Table 10 presents
the results of a study of 7 different F-wave parameters in CTS. The study by Kuntzer140 met 6 AAEM CTS LIC and demonstrated that none of the F-wave parameters achieved the specificity and sensitivity for the diagnosis of CTS
of direct measurements of distal median motor conduction across the carpal tunnel segment of the median nerve. Sander and colleagues,220 in a study that met 5 of the 6 AAEM CTS LIC, evaluated the calculated difference (FWLD:
F-wave latency difference) between the minimum median F-wave latency recorded from the APB and the minimum ulnar F-wave latency recorded from the ADM to identify CTS patients. In the Sander and colleagues220 study, the sensitivity
of the FWLD to identify CTS was less than (1) comparison of median and ulnar distal motor latencies across the carpal tunnel and (2) comparison of median and ulnar mixed nerve latencies across the carpal tunnel. Macleod,157 in
a study that met 4 of the 6 AAEM CTS LIC, noted that there was a high percentage of repeater F waves in CTS, which are identical recurring F waves with the same latency, configuration, and amplitude. However,
abnormalities of median F-wave parameters can be caused by pathology not only in the carpal tunnel segment of the median nerve, but also by pathology along the length of the median motor nerve fibers to the APB from the spinal cord to the
wrist. For all these reasons, measurements of F-wave latencies and other F-wave parameters are not recommended for the diagnosis of CTS.
Buschbacher,35 in a study that met 5 of the 6 AAEM LIC, reported the results of F-wave parameter in 195 reference subjects. Fisher73 (1997) used CTS as a model for analyzing the effects of focal nerve injury
on F-wave parameters.Table 9. Comparison of the Median Motor Nerve
Distal Latency (2nd Lumbrical) to the Ulnar Motor Nerve Distal Latency (Interossei) in CTS. Author Uncini and colleagues254 Year 1993 Number of Normal Hands
(subjects) 72 (47) Normal Subject’s Age: Mean (range) 45 (18 to 78) Number of CTS Hands (patients) 95 (70) CTS Subject’s Age: Mean
(range) 49 (26 to 78) Technique: Conduction
Distance Anatomical landmarks Stimulation Site (median) Wrist crease Stimulation Site (ulnar) Wrist crease Recording Site Palm* Minimum Hand Temperature 32°C Difference Median-Ulnar Onset Latency ± SD 0.10 ± 0.19 ms Criteria for Abnormal Value Mean + 2 SD Abnormal Value Difference in
Median and Ulnar Latency >0.5 ms Specificity of Abnormal Value 97.5% (estimate) Sensitivity of Abnormal Value 10% (56%)† * Lateral to midpoint 3rd metacarpal bone † In the Uncini and colleagues paper,254 comparison of median motor conduction (lumbrical) and ulnar motor conduction (interossei) was done only in the CTS patients with
(1) normal median sensory conduction from D2 to wrist (SCV >45 ms) and (2) normal median motor conduction from wrist to APB (MDL <4.3 ms) so that the percentage (10%) of abnormal comparison studies of median/ulnar motor conduction
was reported for a subset of the CTS patient population; from the data in the paper, the maximum possible percentage of abnormal comparison studies of median/ulnar motor conduction for the whole CTS patient population was calculated
to be 56%. Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
CTS = Carpal Tunnel Syndrome SD = Standard Deviation
APB = Abductor Pollicis Brevis MDL = Motor Distal Latency SCV =Sensory
Conduction Velocity
There are 4 studies listed in Table 1 that provide median sensory nerve conduction data in normal subjects which support the choice of abnormal values in the 6 studies in Table 11 for median sensory peak latency,
median sensory onset latency, and median sensory CV (calculated from the onset latency and conduction distance).34,58,110,242
There were 19 other median sensory NCSs of the peak latency, onset latency, and CV with conduction
between the wrist and a digit (conduction distance of 13 to 14 cm) that met 4 or 5 of the AAEM CTS LIC with the following incidence of abnormal findings (absent response, prolonged peak or onset latency, or reduced CV) in patients with CTS: Andary
and colleagues9 (1996), 27%; Kothari and colleagues135 (1995), D2 42% and D3 54%; White and colleagues264 (1988), 44%, if a response could be elicited; Rosen214 (1993), 48%; Mills171 (1985), 53%;
Sheean and colleagues233 (1995), 55%; Stevens243 (1987), 64%; Seror228 (1994), peak latency 61%, CV 66%; Preston and Logigian200 (1992), 67%; Felsenthal71 (1979), 70%; Trojaborg253 (1996),
D2 70% and D3 72%; Gunnarsson91 (1997), 77%; Melvin and colleagues167 (1973), 79%; Marinacci159 (1964), 83%; Monga and colleagues174 (1985), 86%; Kimura and Ayyar131 (1985), 92%; Kemble125 (1968), 93%; Plaja199 (1971), 98%; Merchut and colleagues168 (1990), 100%.
While most authors used the index finger (Digit 2 or D2) for stimulation or recording, some prefer to use the middle finger (Digit 3
or D3) instead of the index finger to evaluate median sensory conduction in CTS.31,117,118,173,181,192,271 The studies that evaluated median digit-wrist sensory conduction with several digits noted abnormalities in CTS patients more often
with evaluation of the middle finger compared to the index finger, and evaluation of the thumb and sometimes the ring finger studies were more often abnormal than both the index and middle finger studies.135,188,189,253
There are 2 studies of median sensory conduction from digit to wrist in normal subjects that met 5 of the 6 AAEM CTS LIC: Stetson242 (1994) D2 onset latency (3.0 ± 0.2 ms) and D2 sensory CV (SCV) (60.2 ± 4.9 m/s); Buschbacher36 onset
(D2 = 2.6 ± 0.3 ms, D3 = 2.7 ± 0.3 ms) and peak (D2 and D3 = 3.4 ± 0.3 ms) latencies, the Buschbacher36 data presents mean + 2 SD values higher than most of the reference values in the 7 studies in Table 11.
Median Sensory Conduction from the Palm to the Wrist. Table 12 presents the results of 7 studies of median sensory and/or mixed NCSs of an 8-cm length of the median nerve passing through the carpal tunnel. These 7 studies that met
all 6 AAEM CTS LIC determined that between 67% and 84% of patients with CTS demonstrate a prolonged median peak latency, onset latency, or CV with a conduction distance of 8 cm.
In Table 1, there are 4 studies of median sensory and/or
mixed nerve conduction between the wrist and palm in normal subjects. Using a technique to study the conduction of the wrist-palm median nerve segment similar to Kimura,130 Di Benedetto and colleagues58 reported a difference
in peak latency in healthy subjects of less than 2.2 ms, and a difference in onset latency in healthy subjects of less than 1.8 ms, the latter value almost identical to the finding of Kimura130 in Table 12. Cruz Martinez and colleagues50 calculated the CV in palm-to-wrist segments of the median nerve from the onset latency in 47 normal subjects, aged 21 to 77 Under the age of 50, the median sensory CV was 55 ± 5 m/s, and over the age of 50, the median sensory CV was 51 ±
5 m/s. Stetson242 in a study of 105 normal subjects noted an onset latency of 1.8 ± 0.2 ms. Buschbacher33 in a study of 248 normal subjects reported an onset latency of 1.6 ± 0.2 ms and a peak latency of 2.1 ±
0.2 ms.
There were 15 additional studies that report median mixed nerve conduction over a 7 cm to 8 cm distance across the carpal tunnel that met 4 or 5 of the 6 AAEM CTS LIC with the following incidence of abnormal findings in patients
with CTS: Kimura121 (1978), 45%; Andary and colleagues9 (1996), 57%; White and colleagues264 (1988), 65%, a study that ignored cases with absent responses; Mills171 (1985), 67%; Robinson and colleagues211 (1998)
70%; Sheean and colleagues233 (1995), 73%; Seror228 (1994), 76%; Preston and Logigian200 (1992), 82%; Stevens243 (1987), 87%; Monga and colleagues174 (1985), 88%; Felsenthal and Spindler71 (1979),
100%; Wongsam271 (1983), 100%;Rosen214 (1993), 100%; Rossi and colleagues216 (1994), 100%.Table 10. Median Motor Nerve F-W ave Studies in CTS. Author Kuntzer140 Year 1994 Number of Normal
Hands (subjects) 70 (70)* Normal Subject’s Age: Mean (range) 43 (25 to 70) Number of CTS Hands
(patients) 100 (100)* CTS Subjects Age: Mean (range) 51 (26 to 85) Stimulation Site Wrist Recording Site APB Minimum Hand
Temperature 32°C F-W ave Parameter Persistence Chronodispersion Minimal latency Minimal ulnarmedian F-wave latency difference Mean duration Mean amplitude Mean
amplitude ratio†Normal ± SD 92.8 ± 9.2% 1.42 ± 0.37 ms 27.6 ± 2.1 ms 0.59 ± 0.91 ms 10.67 ± 1.62 ms 0.297 ± 0.124 mV 2.97 ± 1.21 Criteria for Abnormal
Value Mean – 2 SD Mean + 2 SD Formula + 2 SD‡ Mean + 2 SD Mean + 2 SD Mean + 2 SD Mean + 2 SD Abnormal Value <70% >2.2 ms SD = 1.4 72.4 >14 ms >0.545 mV >5.39 Specificity of Abnormal Value 91% (actual) 80% (actual) 86% (actual) 90% (actual) 10% (actual) 10% (actual) 70% (actual) Sensitivity of Abnormal Value 35% 69% 16% 48% 2% 2% 15% * For each reference subject, only 1 hand was tested; for each CTS patient, only the most symptomatic hand was tested. † Mean F-wave amplitude as a percentage of the median CMAP.
‡ Formula: minimum F-wave
latency (ms) equals 0.12 × height (cm) + 6.8.Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
CTS = Carpal Tunnel Syndrome SD = Standard Deviation APB = Abductor Pollicis Brevis CMAP = Compound Muscle Action PotentialTable 11. Median Sensory Nerve Conduction Between Wrist and Digit in CTS. Author Casey and
LeQuesne39Kimura130 Carroll38 Jackson and Clifford110 Cioni and colleagues47 Kuntzer140 Padua and colleagues188 Padua and colleagues189 Scelsa and colleagues221 Year 1972 1979 1987 1989 1989 1994 1996 1997* 1998 Number of Normal Hands (subjects) 75 (75) 122 (61) 100 (50) 38 (38) 56 (54) 70 (70)† 40 (36) 30 (25) Normal Subject’s Age: Mean (range) 51 (30 to 70) 43 (15 to 50) 47 (16 to 82) 42 (21 to 69) 38 (18 to 68) 43 (25 to 70) 44 (19 to 79) 42 (23 to 63) Number of CTS Hands (patients) 16 (16) 172 (105) 161 (101) 131 (123) 375 (370) 100 (100)† 50 (43) 500 (379) 67 (42) CTS Subject’s Age: Mean (range) 56 (35 to 70) 48 (20 to 78) 45 (22 to 82) 53 (21 to 85) 46 (20 to 72) 51 (26 to 85) 45 (23 to 80) 51 (20 to
88)50 (25 to 85) Technique: Conduction Distance Anatomical landmarks Anatomical landmarks 13 cm 14 cm Anatomical landmarks 14 cm Anatomical landmarks‡ Anatomical landmarks Stimulation Site Middle finger (D3) 3 cm proximal to wrist crease Index finger (D2) Wrist Index finger (D2) Middle finger (D3) Middle finger (D3) Index finger (D2) Recording Site Wrist Index finger (D2) Wrist Index finger (D2) Wrist Wrist Wrist Wrist Minimum Hand Temperature 35°C 34°C 30°C 31°C 30°C 32°C 31°C 32°C Median Sensory Peak Latency ± SD Not reported Not reported 2.68 ± 0.16 ms age 16 to 39
2.91 ± 0.24 ms age 40 to 59
3.03 ± 0.23 ms age 60 to 823.16 ± 0.16 ms Not reported Not reported Not reported Not reported Median Sensory Onset Latency ± SD Not reported 2.82 ± 0.28 ms Not reported 2.47 ± 0.12 ms Not reported Not reported Not reported Not reported Median Sensory Conduction Velocity
(calculated from onset latency*) ± SD 54.8 ± 7.3 m/s Not reported Not reported Not reported 58.4 ± 4.1 m/s 49.6 ± 2.8 m/s D3: 53.8 ± 5.1 m/s 58 ± 5 m/s# Criteria for Abnormal Value Mean - 2 SD Mean + 2 SD Mean + 2 SD Mean + 2 SD Mean – 2 SD Mean – 2 SD Mean – 2 SD Mean – 2.5 SD Abnormal Value <40 m/s Sensory latency Onset >3.4 ms Sensory peak latency
>3.0 ms age 16 to 39
>3.4 ms age 40 to 59
>3.5 ms age 60 to 82Sensory latency
Peak >3.48 ms
Onset >2.72 ms<50 m/s SNCV
D3: <44 m/sSNCV
D3: <44 m/sSNCV
D2: <46 m/sSpecificity of Abnormal Value 97.5% (estimate) 97.5% (estimate) 100% (actual) 97.5% (actual) 97.5% (estimate) 100% (actual) 97.5% (estimate) 98% (actual) Sensitivity of Abnormal Value 43% 63% 49% 66% 80% (96%)§ 49% D3: 64% D3: 67% 40% The antidromic median nerve sensory conduction studies cited in Table 9 were performed by securing surface recording ring electrodes on the index or middle finger and stimulating the median nerve in the wrist proximal to the carpal tunnel.
With these anatomic landmarks, the conduction distance is usually 13 to 14 cm in normal adults. The time (latency) from the stimulus artifact to the onset or peak of the negative deflection of the biphasic or triphasic waveform was
measured in milliseconds and recorded as the median sensory peak latency. Studies have shown that the orthodromic median nerve sensory conduction study can be performed by stimulating the digit and recording from the wrist and the
latency measurements results are essentially identical though the amplitude of the sensory nerve action potential (SNAP) is less.147 Slowing of median nerve sensory conduction in the carpal tunnel with nerve injury will
result in prolongation of the median sensory peak latency and slowing of the conduction velocity.
* 1997 paper cites reference population studies performed in the same laboratory published in 1996.
† For each reference
subject, only 1 hand was tested; for each CTS patient, only the most symptomatic hand was tested. ‡ Written communication. § In the Cioni and colleagues paper,47 measurement of the median SNCV from digit to wrist
was done only in a CTS patient’s hand with normal median motor distal latency (≤4.3 ms) so that the percentage (80%) of abnormal median SNCV was reported for a subset of the CTS population; from the data in the paper, the
maximum possible percentage of abnormal median SNCVs for the whole CTS population was calculated to be 96%. # Written communication: calculated form the onset latency.Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
CTS = Carpal Tunnel Syndrome SD = Standard Deviation SNCV = Sensory Nerve Conduction VelocityTable 12. Median Sensory and Mixed Nerve Conduction Between Wrist and Palm in CTS. Author Jackson and
Clifford110Kimura130 Scelsa and colleagues221 Kuntzer140 Di Guglielmo and colleagues59 Padua and colleagues188 Padua and colleagues189 Year 1989 1979 1998 1994 1997 1996 1997* Number of Normal Hands (subjects) 38 (38) 122 (61) 30 (25) 70 (70)† 88 (69) 40 (36) Normal Subject’s Age: Mean (range) 42 (21 to 69) 43 (15 to 50) 42 (23 to 63) 43 (25 to 70) 40 (20 to 86) 44 (19 to 79) Number of CTS Hands (patients) 131 (123) 172 (105)‡ 67 (42) 100 (100)† 294 (198) 50 (43) 500 (379) CTS Subject’s Age: Mean (range) 53 (21 to 85) 48 (20 to 78)‡ 50 (25 to 85) 51 (26 to 85) 46 (13 to 84) 45 (23 to 80) 51 (20 to 88) Technique: Conduction Distance 8 cm 8 cm Anatomical landmarks Anatomical land– marks (6-8 cm) Anatomical landmarks Anatomical landmarks Stimulation Site Palm Wrist crease: 3 cm proximal, 5 cm distal Palm Palm Wrist crease: 1-2 cm proximal, 3 cm distal D3 Recording Site(s) Wrist D2 Wrist Wrist D2 Palm and wrist Minimum Hand Temperature 31°C 34°C 32°C 32°C 32°C 31°C Median Sensory Onset Latency ± SD 1.54 ± 0.12 ms Not reported Not reported Not reported Not reported Not reported Median Sensory Peak Latency ± SD 2.03 ± 0.12 ms Not reported Not reported Not reported Not reported Not reported Difference Median Sensory Onset Latency ± SD Not reported 1.41 ± 0.18 ms Not reported Not reported Not reported Not reported Median Sensory Conduction Velocity ± SD Not reported Not reported 58.5 ± 5.2 m/s§ 54.2 ± 3.1 m/s 58.1 ± 6.4 m/s 58.3 ± 6.4 m/s Criteria for Abnormal Value Mean + 2 SD Mean + 2 SD Mean – 2.5 SD Mean – 2 SD Mean – 2 SD Mean – 2 SD Abnormal Value Onset >1.78 ms Peak >2.27 ms Difference >1.8 ms <46 m/s <48 m/s <45 m/s <45 m/s Specificity of Abnormal Value 97% (actual) 97.5% (estimate) 98% (actual) 97% (estimate) 97.5% (estimate) 97.5% (estimate) Sensitivity of Abnormal Value 69% 84%‡ 67% 83% 13% (56%)# 76% 20% (81%)* The nerve conduction studies of the carpal tunnel segment of the median nerve described in Table 8 were obtained in 3 different ways. (1) To study median mixed nerve conduction, Jackson and Clifford,110 Kuntzer,140 and Scelsa and colleagues,221 placed recording disc electrodes over the median nerve above the wrist and stimulated the median nerve in the palm between the 2nd and 3rd metacarpal heads with measurement of the conduction
distance. Measurements of the time (ms) from the stimulus artifact to the onset and negative peak of the potential were recorded as the onset and peak latencies, respectively. (2) To study median sensory nerve conduction, Kimura130 and Di Guglielmo and colleagues59 placed recording ring electrodes on the index finger and stimulated the median nerve in 2 locations, 3 cm proximal to the wrist crease and 5 cm distal to the wrist crease. Measurements of
the time (ms) from the stimulus artifact to the onset of the sensory nerve action potential or SNAP (onset latency) were made for each site and the difference calculated and (a) reported as the conduction time of the sensory
fibers in the median nerve segment in the carpal tunnel or (b) used to calculate the sensory conduction velocity (SCV) of the carpal tunnel segment. (3) To study median nerve sensory conduction, Padua and colleagues188,189 placed stimulating ring electrodes on the middle finger and a bipolar bar electrodes on the palm and wrist. The palm wrist conduction velocity was calculated the (palm-wrist distance) / [(digit-wrist onset latency) – (digit palm
onset latency)].
* The 1997 Padua and colleagues paper189 references studies of normal subjects published in the 1996 Padua and colleagues paper.188 In the 1997 Padua and colleagues paper,189 measurement of median sensory conduction in the carpal tunnel segment was done only in CTS patients with normal (1) median sensory conduction from D1 to wrist (SCV >42 m/s), (2) normal median sensory conduction from D3 to wrist
(SCV >44 m/s, and (3) and normal median motor distal latency (<4 ms) so that the percentage (20%) of abnormal median sensory conduction across the wrist was reported for a subset of the CTS population; from the data in the paper,
the maximum possible percentage of abnormal median sensory conduction in the carpal tunnel segment for the whole CTS patient population was calculated to be 81%.
† For each reference subject, only 1 hand was tested; for
each CTS patient, only the most symptomatic hand was tested. ‡ Written communication. § Calculated from onset latency (written communication).
# In the Di Guglielmo and colleagues paper,59 measurement
of median sensory conduction in the carpal tunnel segment was done only in CTS patients with normal median sensory conduction from wrist to D2 (SCV >45 m/s) and normal median motor distal latency (<4.2 ms) so that the percentage
(13%) of abnormal median sensory conduction across the wrist was reported for a subset of the CTS population; from the data in the paper, the maximum possible percentage of abnormal median sensory conduction in the carpal tunnel segment
for the whole CTS patient population was calculated to be 56%.Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
CTS = Carpal Tunnel Syndrome SD = Standard Deviation
In a study that met 4 of the 6 AAEM CTS LIC, Rossi216 reported a variation on the orthodromic median and ulnar palmar conduction studies with a slightly longer conduction distance (about 10 cm) to enable selective stimulation of the palmar
branches to the adjacent surfaces of the digits at the metacarpophalangeal joints. Rossi216 concluded that stimulation of the palmar branch to the adjacent surfaces of the middle and ring fingers demonstrated a measurable abnormal response
when the orthodromic median sensory response with stimulation of the fourth digit was absent and when the response with stimulation of the palmar branch of the median nerve to the adjacent surfaces of the index and middle fingers was normal.
Median SNAP Amplitude Studies. Kuntzer,140 in a report that met all 6 AAEM CTS LIC, confirmed that the measurements of median sensory conduction from digit to wrist is more often abnormal in CTS patients than the measurement
of median SNAP amplitude, 49% versus 30% (Table 13). In a study that met 5 of the 6 AAEM CTS LIC, Sander220 noted that median sensory conduction from digit to wrist is more abnormal in CTS than measurement of median SNAP amplitude, 64%
versus 48%. In a study that met 4 of the 6 AAEM CTS LIC, Sheean and colleagues233 (1995) also noted that median sensory conduction from digit to wrist is more often abnormal in CTS patients than measurement of median SNAP amplitude, 55%
versus 41%. Two recent studies (Seror228 and Nesathurai184) and several earlier studies (Cioni,47 Felsenthal,68,70 Jackson and Clifford,110 Redmond and Rivner204 ) that compared the
diagnostic sensitivity of median sensory conduction from digit to wrist to measurements of median SNAP amplitudes reached the same conclusion with the exception of Loong and Seah,148 who computed the ratio of the median SNAP amplitude to
the ulnar SNAP amplitude in the same hand.
Two studies of normal subjects that met 5 of the 6 AAEM CTS LIC noted values slightly greater than the values reported by Kuntzer140 in Table 13 for normal subjects for the mean
and SD of the median SNAP amplitude: 32.7 ± 11.4 µV by Stetson242 (1995) and 41 ± 20 µV by Buschbacher.33
Median Sensory Nerve Wrist to Palm SNAP Amplitude Ratio. The ratio
of the amplitude of the median SNAP recorded from a digit with (1) stimulation of the median nerve at the wrist and (2) stimulation in the palm makes it possible to identify median sensory nerve conduction block across the carpal tunnel.
Table 13. Median SNAP Amplitude in CTS. Author Kuntzer140 Year 1994 Number of Normal Hands (subjects) 70 (70)* Normal Subject’s
Age: Mean (range) 43 (25 to 70) Number CTS Hands
(patients) 100 (100)* CTS Subject Age 51 (26 to 85) Stimulation Site Digit‡ Recording Site Wrist Minimum Hand
Temperature 32°C Normal SNAP
Amplitude ± SD 12 ± 2.5 µV Criteria for
Abnormal Value Mean – 2 SD Abnormal Values <7 µV Specificity of
Abnormal Value* 100% (actual) Sensitivity of
Abnormal Value†30% * For each reference subject, only 1 hand was tested; for each CTS patient, only the most symptomatic hand was tested.
† Stimulation of the most symptomatic finger or third digit.Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
CTS = Carpal Tunnel Syndrome SD = Standard Deviation SNAP = Sensory Nerve Action Potential
Table 14 presents the results of a study by Di Guglielmo59 that met all 6 AAEM CTS LIC; the incidence of sensory conduction block was low (13%) with the criteria of a greater than 50% reduction in SNAP amplitude. Lesser
and colleagues,144 in a study that met 5 of the 6 AAEM CTS LIC, reported that 36% of CTS patients showed evidence of sensory conduction block across the carpal tunnel but did not provide data on temporal dispersion and phase cancellation
which would give the appearance of conduction block as did Di Guglielmo.59
In a study of 258 normal subjects listed in Table 1, Buschbacher36 noted up to a 50% to 55% increase in the SNAP amplitude
between wrist and palm stimulation in normal subjects, a finding similar to that reported by Di Guglielmo.59
Table 14. Median SNAP
Wrist to Palm Amplitude Ratio in CTS. Author Di Guglielmo and colleagues59 Year 1997 Number of Normal Hands
(subjects) 88 (69) Normal Subject’s Age: Mean (range) 40 (20 to 86) Number of CTS Hands (subjects) 294 (198) CTS Subject’s Age: Mean
(range) 46 (13 to 84) Technique: Conduction
Distance Anatomical landmarks Wrist Stimulation Site 1 cm to 2 cm proximal to wrist crease Palm Stimulation Site 3 cm distal to wrist crease Recording Site D2 Minimum Temperature 32°C Amplitude (wrist) ± SD 42 ± 19 µV Amplitude (palm) ± SD 45 ± 21 µV Wrist to Palm Amplitude Ratio ± SD 0.8 ± 0.2 Criteria for Abnormal Value Lowest value of range of normal values* Abnormal Value <0.5 Specificity of Abnormal Value 100% (actual) Sensitivity of Abnormal Value 13% * Written communication. Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
CTS = Carpal Tunnel Syndrome SD = Standard Deviation SNAP = Sensory Nerve Action Potential
Median Sensory Short-segment Incremental Studies. Table 15 presents the results of sequential antidromic stimulation of the median sensory nerve at 1-cm intervals across the carpal tunnel recording from the middle
finger
Table 15. Short-segment Incremental Median Sensory Nerve Conduction Across the Carpal Tunnel in CTS. Author Nathan and colleagues181 Year 1988 Number of Normal Hands
(subjects) 70 (38) Normal Subject’s Age: Mean (range) 38 (16 to 69)* Number of CTS Hands
(patients) 54 (30) CTS Subject’s Age: Mean
(range) 43 (23 to 70)* Technique: Conduction Distance 1-cm intervals Stimulation Site 9 points Referenced to the Wrist Crease Start 2 cm proximal End 6 cm distal Recording Site Middle finger Minimum Hand Temperature 30°C Maximum Difference between Consecutive Segments ± SD 0.29 ± 0.8 ms Criteria for Abnormal Value Calculated range of normal 0.1 to 0.3 ms Abnormal Value >0.4 ms / >0.5 ms Specificity of Abnormal Value 81% / 97% (actual) Sensitivity of Abnormal Value 81% / 54% The median sensory conduction study was performed by placing the recording ring electrodes on the middle finger and stimulating the median nerve at 9 points separated by 1-cm intervals beginning 2 cm proximal to the wrist crease and ending
6 cm distal to the wrist crease. The time (ms) from the stimulus artifact to the peak of the SNAP was measured for each stimulation site and the difference between the peak latency for successive SNAPs calculated. Two years later,
Nathan and colleagues,182 in a study that also met 6/6 AAEM CTS LIC, localized the slowing of conduction most commonly to the an area 3 to 4 cm distal to the wrist crease.
*Written communication.Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
CTS = Carpal Tunnel Syndrome SD = Standard Deviation
SNAP = Sensory Nerve Action Potential
by Nathan and colleagues,181 a short-segment incremental stimulation technique (antidromic inching test or AIT) initially described by Kimura.130 Though time consuming, the landmark studies by Kimura128,130 localized
the Practice Parameter: Carpal Tunnel Syndrome abnormality of median sensory conduction in most CTS patients to the distal edge of the carpal ligament, and this finding has been confirmed by Nathan and colleagues,182 White
and colleagues,264 Imaoka and colleagues,106 and Seror.226 Because a frequency distribution of the segmental latency differences in the normal subjects showed a skewed distribution of data, Nathan181 used
a contingency table to evaluate the sensitivity and specificity of 2 different criteria of abnormality (0.4 ms and 0.5 ms). Although Nathan181 recommends use of the 0.4 ms criterion of abnormality, only the 0.5 ms criterion provides specificity
(97%) comparable to the other tests presented in this review.
Imaoka and colleagues106 in a study that met 5 of the 6 AAEM CTS LIC, used a special linear grid of 9 surface electrodes at 15 mm intervals (a total of 8 neighboring
pairs of electrodes) to record the median SNAP simultaneously across the wrist with stimulation of the median nerve at the elbow. With a criterion of deviation by 0.6 ms or more from a predicted peak latency value based on measurements of peak
latencies recorded proximal to the wrist crease, Imaoka106 and colleagues (1992) reported a specificity of 99% compared to normal subjects (mean + 3 SD) and a high test sensitivity (87% in mild CTS).
Seror,226 in a study that met 4 of the 6 AAEM CTS LIC, used an orthodromic inching test (OIT) with stimulation of the third digit and measuring the peak latency of the SNAP recorded with a bipolar fixed distance (22 mm) surface electrode moved centimeter by
centimeter from a point 4 cm proximal to the distal wrist crease to a point 6 cm distal to the distal wrist crease to provide 11 measurements; an abnormality was defined as a conduction delay greater than 0.36 ms based on control studies with a range
of 0.20 to 0.34 ms. Seror226 concluded that most CTS patients can be diagnosed with other methods and that the more time consuming “inching” technique is needed to confirm the diagnosis in only about 5% of all CTS patients.
Seror,224 in a study that met 4 of the 6 AAEM CTS LIC, concluded that the OIT was superior to the AIT because the OIT was more sensitive than the AIT, the stimulation site and intensity was unchanged during the study which
ensures that the same nerve fibers are evaluated, and the stimulation intensity is less and better tolerated by the patient compared to AIT.
Comparison of Carpal Tunnel Segment Median Mixed Nerve Conduction to More Proximal (Forearm) Mixed Nerve Conduction or Distal (palm to digit) Median Sensory Nerve Conduction. The
possible usefulness of comparing CVs of different segments of the same nerve to demonstrate focal conduction slowing to minimize intersubject variability has been evaluated with median sensory and mixed nerve conduction in CTS patients. The results
of 2 studies that met all 6 AAEM CTS LIC are presented in Table 16. The first by Scelsa221 concluded that comparison of the median palm to index finger sensory CV to the median carpal tunnel mixed nerve CV demonstrated a sensitivity to
detect CTS (87%) that was significantly greater than the sensitivity (61%) of comparison of the median forearm CV to the median carpal tunnel CV with similar specificities (98% and 96%, respectively). The second by Kuntzer140 demonstrated
an intermediate sensitivity (69%) with similar specificity (99%) by comparison of the peak latency of the mixed nerve median palm to wrist segment to the peak latency of the median sensory palm to D2 segment. There are also 2 studies that meet all
6 AAEM CTS LIC by Padua and colleagues188,189 that described the usefulness of a ratio of the orthodromic sensory CV for 2 segments of the median sensory nerve (D3 to palm/palm to wrist) to diagnose CTS with high sensitivity: 1996, 98%
and 1997, 97%.
In 1985, Kimura and Ayyar131 reported a 100% incidence of abnormalities in CTS patients if the ratio of the median antidromic sensory CV across the wrist to the median sensory CV across the forearm was calculated.
However, in a study that met 4 of the 6 AAEM CTS LIC, Rosen214 noted that the quotient of the median antidromic mixed nerve CV in the carpal tunnel segment to the antidromic median sensory CV in the forearm segment (70%) was less sensitive
than median mixed nerve palm to wrist conduction (100%).
Buschbacher,33 in a study of 258 normal subjects listed in Table 1, noted that 50% of the wrist to digit median sensory peak latency is attributable to the wrist-palm
segment, a finding that agrees well with the ratio of the peak latency for the 2 segments reported by Kuntzer:140 0.98 ± 0.17 in Table 16.
Comparison of Median Sensory Nerve Conduction to Ulnar or Radial Sensory Nerve Conduction in the Same Limb. In
theory, the biologic variation in speed of nerve conduction from person to person due to age and genetic differences can be controlled by comparison of the speed of nerve conduction in 1 nerve to another nerve in the same limb.69,243 This
comparison principle underlies the basis for development of the sensory NCSs reported in Tables 17, 18, 19, and 20.
Comparison of Median and Ulnar Sensory Nerve Conduction Between Wrist and Digit. Table 17 presents
the results of a study that met all 6 AAEM CTS LIC by Kuntzer140 who determined the difference between the median and ulnar nerve peak latency measurements with orthodromic stimulation (14-cm conduction distance) in CTS patients and normal
control subjects and found the percentage of CTS patients with abnormal values was 61%. Stetson,242 in a study of 105 normal subjects listed in Table 1, noted a value (mean + 2 SD = 0.5ms) identical to that reported by Kuntzer.140 A
study that met 5 of the 6 AAEM CTS LIC showed a slightly lower sensitivity for the same test in CTS patients: Andary9 (1996), 42%.
Table 16. Median Sensory and Mixed Nerve Conduction in CTS: Wrist and Palm Segment Compared to Forearm or Digit Segment. Author Scelsa and colleagues221 Kuntzer140 Padua and colleagues188 Padua and colleagues189 Year 1998 1994 1996 1997* Number of Normal Hands (subjects) 30 (25) 70 (70)‡ 40 (36) Normal Subject’s Age: Mean (range) 42 (23 to 63) 43 (25 to 70) 44 (19 to 79) Number of CTS Hands (patients) 67 (42) 100 (100)‡ 50 (43) 500 (379) CTS Subject’s Age: Mean
(range) 50 (25 to 85) 51 (26 to 85) 45 (23 to 80) 51 (20 to 88) Technique: Conduction
Distance Anatomical landmarks Anatomical landmarks Anatomical landmarks Carpal Tunnel Segment Stimulation Site Palm Palm Palm D3 Recording Site Wrist Wrist Wrist Wrist Other Segment Stimulation Site Palm Elbow Palm D3 Recording Site D2 Wrist D2 Palm Minimum Hand Temperature 32°C 32°C 32°C 31°C Difference Between Median SCV ± SD of CTS Segment and
of Other Segment 2.7 ± 3.1 m/s† 5.7 ± 4.3 m/s† Not reported Not reported Ratio of Onset Latencies:
Palm to Wrist/Palm to D2 Not reported Not reported 0.98 ± 0.17 Not reported Ratio of Conduction Velocities: D3 to Palm/Palm to Wrist Not reported Not reported Not reported 0.82 ± 0.08 Criteria for Abnormal Value Mean + 2.5 SD Mean
+ 2.5 SDMean + 2 SD Mean + 2 SD Abnormal Value >10 m/s >16 m/s >1.32 ≥1.0 Specificity of Abnormal Value* 98% (actual) 96%
(actual)99% (actual) 97.5 % (estimate) Sensitivity of Abnormal Value† 87% 61% 69% 98% 87% (97%)* * The 1997 Padua and colleagues paper189 references studies of normal subjects published in the 1996 Padua and colleagues paper.188 The D3-palm segment SNCV was measured directly. The SNCV of the palm-wrist segment
was computed from the palm-wrist distance (mm) divided by [D3 to wrist latency (ms) minus D3 to palm latency (ms)] In the 1997 Padua and colleagues paper,189 measurement of the ratio of SNCV of the distal (D3 to palm) to
proximal (palm to wrist) segments, defined as the distoproximo ratios, was done only in CTS patients with normal (1) median sensory conduction from D1 to wrist (SCV >42 m/s), (2) normal median sensory conduction from D3 to wrist
(SCV >44 m/s, and (3) and normal median motor distal latency (<4 ms) so that the percentage (87%) of abnormal median distoproximo ratios was reported for a subset of the CTS population; from the data in the paper, the maximum
possible percentage of abnormal distoproximo ratios for the whole CTS patient population was calculated to be 97%.
Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
CTS = Carpal Tunnel Syndrome SD = Standard Deviation SNCV = Sensory Nerve Conduction Velocity SCV = Sensory Conduction VelocityTable 17. Comparison of Median and Ulnar Sensory Nerve Conduction Between Wrist and Digit in CTS. Author Kuntzer140 Year 1994 Number of Normal Hands
(subjects) 70 (70)* Normal Subject’s Age: Mean (range) 43 (25 to 70) Number of CTS Hands (patients) 100 (100)* CTS Subject’s Age: Mean
(range) 51 (26 to 85) Technique: Conduction Distance 14 cm Stimulation Site Median: Digit 3† Ulnar: Digit 5 Recording Site Wrist Minimum Hand
Temperature 32°C Difference Median-Ulnar
Peak Latency ± SD 0.14 ± 0.16 ms Criteria for Abnormal Value Mean + 2 SD Abnormal Value Difference in Median and Ulnar Peak Latency >0.50 ms Specificity of Abnormal Value 100% (actual) Sensitivity of Abnormal
Value 61% * For each reference subject, only 1 hand was tested and for each CTS patient, the most symptomatic hand was tested.
† D3 or the most symptomatic digit was tested.Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
CTS = Carpal Tunnel Syndrome SD = Standard Deviation
Comparison of Median and Ulnar Sensory (Mixed) Nerve Conduction between Wrist and Palm. Table
18 presents the results of 2 studies that met all 6 AAEM CTS LIC. Both Jackson and Clifford110 and Uncini254 determined the difference between the median and ulnar nerve latency measurements with palmar stimulation (8 cm conduction
distance to recording electrodes over the wrist) in CTS patients and normal subjects. Jackson and Clifford110 found the percentage of CTS patients with abnormal values was 66% and Uncini254 reported abnormalities in 56% of CTS
patients with normal median sensory conduction from D2 to wrist (SCV >45 m/s). Jackson and Clifford110 and Uncini254 reported values for the median-ulnar palmar latency difference for normal hands (96% <0.4 ms) and (97%
<0.4 ms), respectively, similar to the findings of 3 independent studies of normal hands: Redmond and Rivner204 (92% <0.5 ms), Stetson and colleagues242 (95% <0.5 ms) and Buschbacher36 (97% <0.5 ms). Six
studies that met 4 or 5 of the 6 AAEM CTS LIC showed similar sensitivity of the comparison study of median and ulnar mixed NCSs between wrist and palm in CTS patients: Kim127 (1983), 57%; Mills171 (1985), 60%; Andary9 (1996),
61%; Robinson211 (1998) 70%; Sheean and colleagues233 (1995) 73%; and Preston and Logigian200 (1994), 94%.
Comparison of Median and Ulnar Sensory Conduction between Wrist and Ring Finger. Table
19 presents the results of 2 studies which compared the speed of sensory conduction in the branches of the median and ulnar nerves to the ring finger and found between 77% to 82% showed abnormalities. Stetson,242 in a study of normal hands,
noted a similar mean and slightly greater standard deviation for the median-ulnar difference (0.1 ± 0.25 ms) than the 2 studies in Table 19. Cioni and colleagues,47 in a study that met all 6 AAEM CTS LIC, found 100% of CTS patients
showed abnormal median sensory conduction compared to ulnar sensory conduction in the ring finger. These findings are similar to the findings of 7 studies that met 4 or 5 of the 6 AAEM CTS LIC Robinson and colleagures211 (1998), 74%; Uncini
and colleagues255 (1989), 78%; Lauritzen and colleagues143 (1991), 87%; Monga and Laidlow173 (1982), 93%; Seror228 (1994), 97%; Johnson and colleagues66 (1981), 100%; Charles and colleagues45 (1990), 100%.
Table 18. Comparison of Median and Ulnar Mixed Nerve Conduction Between Wrist and Palm in CTS. Author Jackson and
Clifford110Uncini and colleagues254 Year 1989 1993 Number of Normal Hands (subjects) 38 (38) 72 (47) Normal Subject’s Age: Mean (range) 42 (21 to 69) 45 (18 to 78) Number of CTS Hands (patients) 131 (123) 95 (70) CTS Subject’s Age: Mean
(range) 53 (21 to 85) 49 (26 to 78) Technique: Conduction Distance 8 cm 8 cm Stimulation Site Palm Palm Recording Site Wrist Wrist Minimum Hand
Temperature 31°C 32°C Difference Median -Ulnar
Onset Latency ± SD 0.08 ± 0.12 ms 0.10 ± 0.14 ms Difference Median-Ulnar
Peak Latency ± SD 0.10 ± 0.11 ms Not reported Criteria for Abnormal
Value Mean + 2 SD Mean + 2 SD Abnormal Value
Difference in Median and Ulnar Latency Onset >0.32 ms Peak >0.31 ms Onset >0.4 ms Peak (not reported) Specificity of Abnormal Value 95% (actual) 97.5%
(estimate)Sensitivity of Abnormal
Values 66% 56% (78%)* The technique for palmar stimulation of the median nerve described by Jackson and colleagues110 in Table 8 was adapted to study the ulnar nerve by placement of the recording electrodes over the ulnar nerve at the wrist and stimulating
in the palm between the 4th and 5th metacarpal heads (see Table 4). The difference in the latency of the median and ulnar mixed nerve latencies was evaluated. * In the Uncini and colleagues paper,254 comparison of median
and ulnar sensory conduction across the palm-wrist segment was done only in the CTS patients with (1) normal median sensory conduction from D2 to wrist (SCV >45 ms) and (2) normal median motor conduction (MDL <4.3 ms) from wrist
to APB so that the percentage (56%) of median/ulnar sensory conduction abnormalities was reported for a subset of the CTS patient population; from the data in the paper, the maximum possible percentage of median/ulnar sensory conduction
abnormalities for the whole CTS patient population was calculated to be 78%. Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
APB = Abductor Pollicis Brevis CTS = Carpal Tunnel Syndrome MDL = Motor Distal Latency SD = Standard Deviation SCV = Sensory Conduction
Velocity
When performing the antidromic median and ulnar sensory conduction study from wrist to D4 (conduction distance of 14 cm), Laroy142 recommended simultaneous recording of SNAPs from another median (D3) and ulnar
(D5) innervated digit to detect inadvertent co-stimulation of the median and ulnar nerves in the wrist. In the same study, Laroy142 found no evidence of mononeural (median or ulnar) innervation of D4 in 2047 hands of 1260 patients.
Comparison of Median and Radial Sensory Conduction Between Wrist and Thumb. Table 20 presents the results of 3 studies which met all 6 AAEM CTS LIC and evaluated sensory conduction in the branches of the median and radial
nerves to the thumb over equal conduction distances. Both Carroll38 and Jackson and Clifford110 determined the difference between the median and radial nerve latency measurements; the findings in the normal control subjects in
both studies were similar (less than 0.3 to 0.4 ms difference was normal). Carroll38 compared the median and radial nerve latency measurements to the thumb in the CTS patients in his study if the median sensory response was normal over
the wrist-digit segment (see Table 11) and estimated a total incidence of abnormal median-radial sensory comparison studies in symptomatic hands of CTS patients to be 60%. Carroll’s estimate is similar to the finding of Jackson and Clifford110 (69%) who compared the median and radial sensory latency in all of their CTS patients (Table 20). Padua188,189 computed the ratio of the radial to median sensory conduction velocity measured from the thumb to the wrist and found 76% of
CTS patients showed abnormalities. Cioni and colleagues,47 in a study that met 6 AAEM CTS LIC found 96% of CTS patients showed abnormal median/radial comparison conduction studies. These findings are similar to the findings of 5 other studies
that met 4 or 5 of the 6 AAEM CTS LIC: White and colleagues264 (1988), 58% (of mild CTS); Robinson and colleagues211 (1998) 76%; Pease and colleagues192 (1989), 87% (of mild CTS); Andary9 (1996),
90%; Johnson and colleagues114 (1987), 100%.
About 30 years ago, Buchthal and colleagues30 reported a 91% incidence of abnormal findings on the needle EMG examination of the APB muscle in patients with CTS:
50% fibrillation activity, 50% decreased recruitment, 66% abnormalities of motor unit action potential (MUAP) configuration. These findings were similar to an earlier study by Marinacci,159 which also reported a very high (96%) incidence
of APB needle EMG abnormalities. The high incidence of needle EMG abnormalities in the APB noted by Buchthal and colleagues31 and by Marinacci,159 may be related to a combination of patient selection,31,159 number
of different sites examined in the APB,31 and the use of quantitative measurements of MUAP parameters.31
Table 19.
Comparison of Median and Ulnar Sensory
Conduction Between Wrist and Ring Finger in CTS.Author Jackson and Clifford110 Uncini and colleagues254 Year 1989 1993 Number of Normal Hands (subjects) 38 (38) 72 (47) Normal Subject’s Age: Mean (range) 42 (21 to 69) 45 (18 to 78) Number of CTS Hands (patients) 131 (123) 95 (70) CTS Subject’s Age: Mean (range) 53 (21 to 85) 49 (26 to 78) Technique: Conduction Distance 14 cm Identical for each subject Range: 12 cm to 14 cm Stimulation Site Wrist Ring finger Recording Site Ring finger Wrist Minimum Hand Temperature 31°C 32°C Difference Median and Ulnar Onset Latency ± SD 0.13 ± 0.15 ms 0.14 ± 0.13 ms Difference Median and Ulnar Peak Latency ± SD 0.09 ± 0.13 ms Not reported Criteria for Abnormal Value Mean + 2 SD Mean + 2 SD Abnormal Value Onset >0.43 ms Peak >0.35 ms Onset >0.4 ms
Peak (not reported)Specificity of Abnormal Value 95% (actual) 97.5% (estimate) Sensitivity of Abnormal Value 82% 77% (89%)* Nerve conduction of the branches of the median and ulnar nerves to the ring finger can be measured by securing surface ring electrodes on the ring finger and surface disc electrodes over both the median and ulnar nerves proximal to the
wrist crease with identical conduction distances (14 cm). The conduction time (ms) from the stimulus artifact to the onset (onset latency) or peak (peak latency) of the SNAP is determined and the medianulnar latency difference calculated.
* In the Uncini and colleagues paper,254 comparison of orthodromic median and ulnar sensory conduction from D4 along an identical distance to the wrist (range 12-14 cm for all tests) was done only in the CTS patients with
(1) normal median sensory conduction from D2 to wrist (SCV >45 ms) and (2) normal median motor conduction (MDL <4.3 ms) from wrist to APB so that the percentage (77%) of median/ulnar sensory conduction abnormalities was reported
for a subset of the CTS patient population; from the data in the paper, the maximum possible percentage of median/ulnar sensory conduction abnormalities for the whole CTS patient population was calculated to be 89%.Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
APB = Abductor Pollicis Brevis CTS = Carpal Tunnel Syndrome Potential MDL = Motor Distal Latency SD = Standard Deviation SCV = Sensory Conduction Velocity SNAP = Sensory Nerve Action
Table 20. Comparison of Median and Radial Sensory Conduction Between Wrist and Thumb in CTS. Author Carroll38 Jackson and Clifford110 Padua and colleagues188 Year 1987 1989 1996 Number of Normal Hands
(subjects) 100 (50) 38 (38) 40 (36) Normal Subject’s Age: Mean (range) 47 (16 to 82) 42 (21 to 69) 44 (19 to 79) Number of CTS Hands (patients) 161 (101) 131 (123) 50 (43) CTS Subject’s Age: Mean (range) 45 (22 to 82) 53 (21 to 85) 45 (23 to 80) Technique: Conduction Distance
(range) 8.7 (6.7 to 10.5) cm 10 cm Anatomic landmarks Stimulation Site Thumb Wrist Thumb Recording Site Wrist Thumb Wrist Minimum Hand Temperature 30°C 31°C 31°C Difference Median and Radial
Onset Latency ± SD Not reported 0.08 ± 0.12 ms Not reported Difference Median and Radial
Peak Latency ± SD 0.09 ± 0.10 ms aged 16 to 39
0.15 ± 0.12 ms aged 40 to 590.13 ± 0.08 ms aged 60 to 82
Not reported Ratio of Radial to Median SCV Not reported Not reported 1.01 ± 0.09 Criteria for Abnormal Value Mean + 2 SD Mean + 2 SD Mean + 2 SD Abnormal Value Difference in latencies age 16 to 39 >0.3 ms age 40 to 59 >0.4 ms age 60 to 82 >0.3 ms Difference in latencies
Onset >0.32 ms
Peak >0.37 msRatio of SVC >1.2 Specificity of Abnormal Value 99% (actual) 100% (actual) 97.5% (estimate) Sensitivity of Abnormal Value 21% (60%)* 69% 74% Nerve conduction of the branches of the median and radial nerves to the thumb can be measured by securing surface ring electrodes on the thumb and surface disk electrodes over both the median and radial nerves proximal to the wrist crease
with identical conduction distances (10 cm). The conduction time (ms) from the stimulus artifact to the onset (onset latency) or peak (peak latency) of the SNAP is determined and reported as the onset or peak latency. Carroll38 and Jackson and Clifford110calculated the difference between the median and radial latencies. Padua and colleagues188 computed the SCV for the median and radial nerve segments and calculated the ratio of the radial
SCV to the median SCV.
* In the Carroll38 paper, comparison of median and radial sensory conduction was done only in the CTS patients with normal median sensory conduction from D2 to wrist (13 cm conduction
distance in Table 3) so that the percentage of abnormal median/radial sensory conduction abnormalities was reported for a subset of the CTS patient population; from the data in the paper, the maximum possible percentage of abnormal
median/radial sensory comparison studies for the whole CTS patient population was calculated to be 60%.Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of test data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on the CTS population.
CTS = Carpal Tunnel Syndrome SD = Standard Deviation SNAP = Sensory Nerve Action Potential SCV = Sensory Conduction Velocity
In a retrospective review of 480 CTS patients, Werner and Albers261 (1995)
reported that the median motor and sensory latencies were the most important predictors of an abnormal needle examination of the APB muscle of 480 CTS patients: 48% abnormalities of MUAP configuration and/or fibrillation activity and 21% fibrillation
activity. Vennix258 noted that 95% of CTS with evidence of denervation on needle EMG had APB CMAP amplitudes less than 7 mV but agreed with Werner and Albers261 that these models are not applicable in the clinical setting
to predict denervation in individual CTS patients.
In 1999, Gnatz and Conway87 debated the issue of the performing needle EMG of the APB muscle and other hand and limb muscles in CTS patients. Gnatz87 concluded that the needle EMG is important in all CTS suspects because
the discomfort and expense of the exam was outweighed by the diagnostic information obtained. Conway87 recommended that needle EMG be performed only when pathology proximal to the carpal tunnel was suspected.13,184 Gnatz
and Conway87 agreed that more studies are needed to evaluate the question of performing needle EMG in every patient suspected of CTS. There are a few other studies which address this issue.176
Effect of Dynamic Hand Exercise on Median Nerve Conduction in CTS. In 1994, Clifford,48 in a study that met all 6 AAEM CTS LIC, evaluated the effect of 4 minutes of repetitive wrist and finger movements on median
sensory nerve conduction to D4 and found a significant difference between a group of CTS patients and normal subjects. However, the difference was of insufficient magnitude to discriminate individual CTS patients from control subjects. Therefore,
the effects of repetitive wrist and finger movements on median NCS in CTS patients are classified as investigational at this time.
Effect of Sustained Wrist Positioning on Median Nerve Conduction in CTS. The effect of sustained
(1 minute or greater) active or passive wrist and finger positioning (maximal flexion or extension) on median sensory and motor nerve conduction in normal subjects and CTS patients has been evaluated by several investigators: Schwartz,222 Marin,158 Dunnan,62 Werner,262 Hansson
and Nilsson,
97 Rosecrance,213 and Kiernan.126
Initial studies which focused on the effect of sustained wrist positioning on the median distal sensory latency and the median motor distal latency produced conflicting
results: Schwartz,222 Marin,158 and Dunnan.62 More recent studies have focused on the effect of prolonged positioning on the amplitude of the median SNAP and reported more promising results: Hansson and Nilsson,97 Rosecrance,213 and
Kiernan.126 Hansson and Nilsson,97 in a study that met 5 of the 6 AAEM CTS LIC, evaluated the effect of prolonged (up to 45 minutes) passive wrist flexion on the median SNAP amplitude and determined the time (T50) it takes
for the SNAP amplitude to fall to one-half the baseline value. Rosecrance and colleagues,213 in a study that met all 6 AAEM CTS LIC, evaluated the recovery time for the SNAP amplitude to return to baseline after 5 minutes of active
extreme wrist and fingers flexion. In both reports, the changes in the SNAP amplitude during (Hansson and Nilsson97) or after (Rosecrance and colleagues213 ) sustained wrist positioning distinguished CTS patients
from normal subjects. Because others have not yet confirmed these results, the effects of sustained wrist positioning on median nerve conduction in CTS patients are classified as investigational at this time.
Hansson and Nilsson96,97 also
provided evidence that the effect of prolonged extreme wrist flexion was due to ischemia and not to compression of the nerve. The results of the recent studies by Hansson and Nilsson96,97 and Rosecrance and colleagues213 are consistent
with the effect of wrist positioning on intracarpal tunnel pressures and median nerve conduction; increased intracarpal tunnel pressures have a greater effect on the amplitude of the median sensory and motor response than on the CV (distal latency).
In 1982, Lundborg and colleagues152 demonstrated that compression of the median nerve in the carpal tunnel to pressures over 50 mm Hg caused a rapidly reversible block of median sensory and motor conduction.
Table 21. Sympathetic Skin Response in CTS. Author Kuntzer140 Sener223 Year 1994 2000 Number of Normal Hands (subjects) 30 (30)* 42 (21) Normal Subject’s Age: Mean (range) 45 (25 to 70) 38 (18 to 60) Number of CTS hands (patients) 30 (30)* 46 (31) CTS Subject’s Age: Mean (range) 48 (32 to 72) 46 (26 to 70) Stimulation Site Opposite wrist Sternum Recording Site D2 and D5 D2 and D5 Minimum Hand Temperature 32°C 32°C Calculation D2/D5 amplitude ratio × 100† Onset latency Normal ± SD 69.8 ± 16.9 D2: 1.42 ± 0.13 s‡
D5: 1.41 + 0.18 s‡Criteria for Abnormal Value Mean – 2 SD Mean + 2 SD Abnormal Value <36 D2: >1.68 s
D5: >1.77 sSpecificity of Abnormal Value 100% (actual) D2: 98% (actual) ‡
D5: 98% (actual) ‡Sensitivity of Abnormal Value 10% D2: 0%
D5: 0% * For each reference subject, only 1 hand was tested; for each CTS patient, only the most symptomatic hand was tested. † Written communication.
‡ Written communication: the data in Table 3 of the published
paper was mislabeled “ms” (the correct units were “s”) and the D2 and D5 SSR studies yield values greater than the abnormal values in 1 of the 42 control subjects and none of the CTS patients. Specificity equals the percentage of reference subjects’ hands with normal results and was either “actual” based on analysis of the test data from the reference population or an “estimate”
based on the statistical distribution of data from the reference population.
Sensitivity equals the percentage of CTS patients’ hands with abnormal results calculated from the test data on
the CTS population.
CTS = Carpal Tunnel Syndrome SD = Standard Deviation SSR = Sympathetic Skin Response
Effect of Brief Wrist Positioning on Median Nerve Conduction in CTS. A
phenomenon that takes place during wrist flexion and extension with limb positioning is longitudinal sliding of the median nerve in the carpal tunnel. In 1976, McLellan164 first reported sliding of the median nerve based on observations
of the effect of limb movements on the orientation of a needle placed in the median nerve proximal to the wrist. Because the nerve slides in the carpal tunnel, the length of median nerve between the stimulating electrodes proximal to the
wrist and the recording electrodes over the thenar muscle (motor study) or the digit (sensory study) is least with wrist flexion, intermediate in the neutral position, and greatest with wrist extension. The effect of longitudinal sliding on median
SNAP latency measurements in normal subjects was first described by McLellan and Swash164 and subsequently confirmed by Valls-Solé and colleagues.257 Valls-Solé and colleagues257 also noted that the
latency differences between flexion and extension wrist positions were significantly less in CTS patients compared to control subjects consistent with limited sliding of the median nerve in the carpal tunnel of CTS patients. Nakamichi and Tachibana177 provided
independent confirmation of the limited sliding of the median nerve in CTS patients with ultrasound measurements. Because the effect of brief positioning on median nerve latency measurements in CTS is less than that of normal subjects, it is unlikely
that these studies would be of value to distinguish CTS patients from normal subjects although there is 1 disputed report27 and a commentary203 to the contrary. For these reasons, studies on the effect of brief wrist postioning
on median nerve conduction in CTS are considered investigational.
Dorfman and Robinson61 reviewed the important principles governing the acquisition and use of normative data in electrodiagnostic medicine and the authors made several points worth restating: (1) EDX data from the disease-free population
may be skewed rather than having a Gaussian distribution and setting the abnormal value by calculating the mean ± 2 standard deviations may result in misclassification of data from the patients, (2) there are several alternative statistical
strategies for dealing with sample distributions which are non-Gaussian to permit identification of an abnormal value to maximize sensitivity and specificity of the test results, and (3) if multiple independent EDX tests are performed on a single
patient, the likelihood of finding an abnormal value on the basis of chance is significant.
Robinson and colleagures211 reported the use of a single summary variable (combined sensory index or CSI) based on the results of
3 different NCSs to assess median sensory conduction across the carpal tunnel: median-ulnar midpalmar orthodromic difference at 8 cm (palmdiff), medial-ulnar ring finger antidromic differences at 14 cm (ringdiff), and median-radial thumb antidromic
difference at 10 cm (thumbdiff). The CSI = palmdiff + ringdiff + thumbdiff. Theoretically random (nonsystematic) technical errors would be canceled out as more observations are collected and reliability would be enhanced. The possibility of making
a false-positive diagnosis by chance alone (i.e., chance observation of a single extreme value) is reduced when multiple observations are combined because it is unlikely that all observations in a healthy subject will have chance extreme values
in the same directions. Lew and colleagues145 confirmed that test-retest reliability of the CSI was superior to a single NCS and, in addition, the CSI was less affected by temperature changes than absolute latency values of individual
NCSs. Finally, combining measurements into a single variable avoids the additive risk of false positive results when making a diagnosis based on any 1 of many tests being “abnormal.”61 Based on results in 53 CTS patients
and 46 control subjects, Robinson and colleagues211 reported a CSI score greater than or equal to 1.0 yields a sensitivity of 83% and a specificity of 95%. The study also confirmed that doing more tests and requiring that only 1 of
many of the tests be abnormal for a diagnosis of CTS produced an excess of false-positive results (nearly 8%). Interestingly, the most recent report by Robinson and colleagues210 noted that there were endpoints for the 3 individual
tests that confidently predicted the results of the CSI without loss of specificity so that it was not necessary to do all 3 tests: palmdiff >0.3 ms, ringdiff >0.4 ms, or the thumbdiff >0.7ms.
McNeil165 recommended
the use of receiver-operating curve (ROC) analysis as a method to use the results of laboratory studies to calculate the percentage risk of patients having a disease. Two papers have used ROC analysis to determine the optimal cut-off value for
NCS abnormalities in patients with CTS.64,91 Limitation of ROC analysis for evaluating EDX studies in CTS patients include the absence of a highly specific diagnostic test for CTS independent of EDX studies (such as biopsy or autopsy),
the need for an estimate of the true prevalence of CTS, and difficulty in generalizing findings from 1 laboratory to another.
Several studies that met 4 or more of the 6 AAEM
CTS LIC compared the relative sensitivity of different tests of median sensory conduction, median motor conduction, and needle EMG in CTS patients.
In 4 of 4 recent (after 1980) studies of patients with CTS, NCSs showed abnormalities
more often than needle EMG of the APB muscle (Kimura and Ayyar,131 Jackson and Clifford,110 Seror,228 and Kuntzer.140)
In 23 of 29 studies of CTS patients, median sensory NCSs were abnormal
more frequently than Motor NCSs.31,47,57,91,110,125,128,131,135,140,159,167,171,174,188,189,200,206,214,220, 221,226,228,233,237,249,253,254,255 The 2 studies published before 1990 that were exceptions may reflect a small
sample of patients (20 hands of 13 patients),128 and a low threshold (3.7 ms) for an abnormal median motor distal latency,110 (the latter information was obtained by written communication from the author and was not included
in the original report). The 4 studies published since 1990 that were exceptions have suggested that computation of the median terminal latency index (Simovic and Weinberg237 ) and comparison of the second lumbrical (median) and interossei
(ulnar) distal motor latency difference has a test sensitivity equal or greater than median sensory conduction (Preston and Logigian,200 Sheean,233 and Trojaborg253). However, these latter median/ulnar lumbrical/interossei
test findings were not confirmed in the study by Uncini254 that met all 6 AAEM CTS LIC.
In 19 of 19 studies of patients with CTS, median mixed NCSs from the palm to the wrist (e.g., 8 cm conduction distance) were abnormal more frequently than median sensory NCSs from the digit to the wrist (e.g., 13 cm to 14cm conduction
distance).9,31,57,59,71,110,128,131,132,140,173,188,189,200, 214,221,228,233,237 These 19 studies included the 7 reports that met 6 AAEM CTS LIC by Jackson and Clifford,110 Kimura,132 Padua and colleagues,188,189 Scelsa
and colleagues,221 Di Guglielmo and colleagues,59 and Kuntzer140 which are summarized in Tables 11 and 12.
In 20 of 20 studies of patients with CTS, comparison of median
sensory/mixed nerve conduction to ulnar sensory/mixed nerve conduction or radial sensory nerve conduction in the same limb of CTS patients were abnormal more frequently than evaluation of median sensory NCSs from wrist to digit alone.9,38,45,47,57,63,110,116,140,143,148,171,173,174, 188,189,192,228,237,248,254,255 These
20 studies included the 6 reports that met 6 AAEM CTS LIC by Carroll,38 Jackson and Clifford,110 Kuntzer,140 Padua and colleagues,188,189 and Uncini and colleagues254 which are summarized
in Tables 9, 17, 18, 19, and 20.
The pooled sensitivity of the several tests evaluated is shown in Table 22 (data analysis by Gary Gronseth, MD). The data in the appropriate table for each study were subjected to a meta-analysis with 95% confidence limits to take
into account the fact that some of the studies included more CTS patients than other studies. CONCLUSIONS
This report provides convincing scientific evidence that median sensory and motor NCSs:
1. Are valid and reproducible clinical laboratory studies. 2. Confirm a clinical diagnosis of CTS with a high degree of sensitivity (>85%) and specificity (>95%).
The sensitivities of the several different median NCSs were compared. The comparison demonstrated that:1. Median sensory NCSs confirm the clinical diagnosis of CTS more often than median motor NCSs (63% to 69% versus 65% to 85%: Tables 3, 11, 12, 18, 19, 20, and 22). 2. The median sensory or mixed nerve conduction from wrist to digit (conduction distance 13 to 14 cm) is less sensitive (65%: Tables 11and 22) for confirmation of the clinical diagnosis of CTS compared to:
a. Techniques which evaluate median sensory or mixed nerve conduction over a short (7 to 8 cm) conduction distance across the carpal tunnel (e.g., palmar studies 74%: Tables 12 and 22); or b. Techniques which compare sensory or mixed nerve conduction of the median nerve through the carpal tunnel to sensory or mixed nerve conduction of the ulnar nerve (85%: Tables 18, 19, and 22) or radial nerve (65%:
Tables 20 and 22) in the same hand; or c. Techniques which compare sensory or mixed nerve conduction of the median nerve through the carpal tunnel to sensory or mixed NCSs of proximal (forearm) and distal (digit) segments of the median nerve in the same limb (85%:
Tables 16 and 22).
RECOMMENDATIONS REGARDING EDX STUDIES TO CONFIRM A CLINICAL DIAGNOSIS OF CTS
Table 22. Comparison of Pooled Sensitivities and Specificities of EDX Techniques to Diagnose CTS. Technique Pooled
Sensitivity* Pooled
Specificity* A Median sensory and mixed nerve conduction: wrist and palm segment compared to forearm or digit segment 0.85†
(0.83,0.88)0.98†
(0.94,1.00)B Comparison of median and ulnar sensory conduction Between wrist and ring finger 0.85
(0.80,0.90)0.97
(0.91,0.99)C Median sensory and mixed nerve conduction Between wrist and palm 0.74†
(0.71,0.76)0.97†
(0.95,0.99)D Comparison of median and ulnar mixed nerve Conduction between wrist and palm 0.71
(0.65,0.77)0.97
(0.91,0.99)E Median motor nerve conduction Between wrist and palm 0.69†
(0.64,0.74)0.98†
(0.93,0.99)F Comparison of median and radial sensory conduction Between wrist and thumb 0.65
(0.60,0.71)0.99
(0.96,1.00)G Median sensory nerve conduction Between wrist and digit 0.65†
(0.63,0.67)0.98†
(0.97,0.99)H Median motor nerve distal latency
0.63†
(0.61,0.65)0.98†
(0.96,0.99)I Median motor nerve terminal latency index
0.62†
(0.54,0.70)0.94†
(0.87,0.97)J Comparison of median motor nerve distal latency (second lumbrical) to the ulnar motor nerve distal latency (second interossei) 0.56‡
(0.46,0.66)0.98‡
(0.90,1.00)K Sympathetic skin response
0.04
(0.00,0.08)0.52
(0.44,0.61)* For each EDX technique to summarize results across studies, sensitivities were pooled from individual studies by calculating a weighted average. In calculating the weighted average, studies enrolling more patients received
more weight than studies enrolling fewer patients. Specificities were similarly pooled by calculating the weighted average. The data in the parentheses below the sensitivity and specificity values represent the lower
and upper 95% confidence limits of the weighted average, respectively. Data analysis courtesy of Dr. Gary Gronseth.
AAEM with the clarification of recommendation 1 and 2a and the addition of 2c based
on new evidence reviewed in the second CTS Literature Review.2 In patients suspected of positive CTS, the following EDX studies are recommended (see Table 22 for sensitivity and specificity of Techniques A –
K):1. Median sensory NCS across the wrist with a conduction distance of 13 to 14 cm
(Technique G). If the result is abnormal, comparison of the result of the median sensory NCS to the result of a sensory NCS of 1 other adjacent sensory
nerve in the symptomatic limb (Standard). 2. If the initial median sensory NCS across the wrist has a conduction distance greater than 8 cm and the result is normal, 1 of the following additional studies is recommended:
a. Comparison of median sensory or mixed nerve conduction across the wrist over a short (7 to 8 cm) conduction distance (Technique C) with ulnar sensory nerve conduction across the wrist over the same short (7 to 8 cm) conduction
distance (Technique D) (Standard), or b. Comparison of median sensory conduction across the wrist with radial or ulnar sensory conduction across the wrist in the same limb (Techniques B and F) (Standard), or c. Comparison of median sensory or mixed nerve conduction through the carpal tunnel to sensory or mixed NCSs of proximal (forearm) or distal (digit) segments of the median nerve in the same limb (Technique A) (Standard). 3. Motor conduction study of the median nerve recording from the thenar muscle (Technique H) and of 1 other nerve in the symptomatic limb to include measurement of distal latency (Guideline). 4. Supplementary NCS: Comparison of the median motor nerve distal latency (second lumbrical) to the ulnar motor nerve distal latency (second interossei) (Technique J), median motor terminal latency index (Technique I), median motor nerve
conduction between wrist and palm (Technique E), median motor nerve CMAP wrist to palm amplitude ratio to detect conduction block, median SNAP wrist to palm amplitude ratio to detect conduction block, short-segment (1 cm) incremental
median sensory nerve conduction across the carpal tunnel (Option). 5. Needle electromyography of a sample of muscles innervated by the C5 to T1 spinal roots, including a thenar muscle innervated by the median nerve of the symptomatic limb (Option).
Based on the second AAEM CTS Literature Review2 the following EDX studies are not recommended to confirm a clinical diagnosis of CTS either because the EDX studies recommended above have greater sensitivity
and specificity or the test is best described as investigational at this time.1. Low sensitivity and specificity compared to other EDX studies: multiple median F-wave parameters, median motor nerve RL, and sympathetic skin response (Technique K). 2. Investigational studies: evaluation of the effect on median NCS of limb ischemia, dynamic hand exercises, and brief or sustained wrist positioning.
Practice standards: generally accepted principles for patient management
that reflects a high degree of clinical certainty.
Practice guidelines: recommendations for patient management that reflect moderate clinical certainty.
Practice options: other strategies
for patient management for which the clinical utility is uncertain.1. Prospective study. 2. Clinical diagnosis of CTS independent of EDX studies: For example, a diagnosis of probable CTS as defined in the second CTS Literature Review2 which is based on a consensus recommendation by Rempel and colleagues.205 3. A uniform protocol for data collection and measurement with the physicians performing and interpreting the EDX studies under investigation blinded to the clinical diagnosis of all the human subjects (normal, CTS, disease control) in the
study at least until the data collection and measurements are completed.
The AAEM recommends that future clinical research studies of the usefulness of EDX studies to confirm the diagnosis of CTS meet 4 additional methodological study criteria:1. Description of EDX technique sufficient to permit replication of the study. 2. Monitor limb temperature continuously during the EDX study. 3. Normal values for EDX technique obtained with concomitant studies or with previous studies in the same laboratory. 4. Criteria of EDX abnormality obtained from normal population and defined in statistical terms.
The AAEM recommends that studies which compare the sensitivity and specificity studies of NCSs and needle EMG to the sensitivity and specificity of other tests proposed for the diagnosis of CTS use the clinical diagnosis of probable CTS as defined in Table 2. These alternative diagnostic studies include the following: quantitative cutaneous sensory testing of perception threshold for vibration, 2-point discrimination,
touch, warmth, cold, and electric current;21,22,120,153,160,168,247 hand symptom diagrams;122,123,124 magnetic resonance imaging and computed tomographic studies of the carpal tunnel;16,17,99,169 thermography;100,170,240 wrist ratio;90 provocation of symptoms by ultrasound;172 and carpal tunnel pressure measurements.78,212
Both the first and second AAEMCTS Literature Reviews recommended that outcome
studies should be performed to assess the harms, benefits, and costs of performing NCSs and needle EMG in patients with symptoms suggestive of CTS.
The AAEM recommends that future outcome studies of treatment of CTS use the
clinical diagnoses of definite CTS (as defined in Table 2) with EDX studies of high sensitivity and specificity for the diagnosis of CTS performed by a specially trained physician, i.e., median mixed nerve palmar studies and/or
comparison of median to ulnar and/or radial sensory NCS in the same hand.
The AAEM CTS Task Force has addressed future research principles over future research topics (except for outcome studies) because the Task Force concluded that
future research studies need to meet these principles (1) to provide reliable and reproducible data to evaluate the usefulness of EDX studies to confirm the clinical diagnosis of CTS and (2) permit comparison of the relative utility of different
EDX studies for that purpose.
It is recommended that the AAEM review this report every 5 years and update the report as necessary.1. This report provides a new consensus based set of inclusion and exclusion criteria for the clinical diagnosis of CTS according to the certainty of the diagnosis: possible CTS, probable CTS, and definite CTS (Table 2). We recommend the
criteria for the diagnosis of probable CTS be used in future studies of EDX tests to reduce the possibility of selection bias, to provide a more uniform population of CTS patients, and to provide a valid scientific basis for comparison
of the results of future studies from different laboratories. This suggestion is a refinement on the original recommendation made in the 1993 CTS Literature Review. 2. Sackett and colleagues217 and others have recommended that clinical research studies of diagnostic tests (including EDX studies) be performed with the physician performing and interpreting the diagnostic tests blinded to the diagnosis
of the subject with the goal of eliminating observer bias. There is a solid body of clinical evidence and experience which indicates that NCSs are useful to confirm the diagnosis of CTS, a body of evidence similar in weight to the
clinical evidence that radiographs are useful to identify fractures of the limb bones and electrocardiograms are useful to identify myocardial ischemia and infarction. Nevertheless, it is worth performing future evaluations of EDX
studies in CTS with the examiner blinded to the clinical diagnosis of the subject as the next step to establishing the validity of these conclusions beyond a reasonable doubt. In fact, some clinical investigators have already begun
to perform evaluations of NCSs in CTS in a blinded fashion (Salerno and colleagues218,219 and Werner and colleagues263 ).
The AAEM has prepared a document that describes the risks in electrodiagnostic medicine.5 Briefly, the risks to the patient of needle EMG include transient discomfort, bruise, hematoma, and infection from the needle insertion required
to perform needle EMG. The risks of NCS to the patient include transient discomfort of the electric shocks. The risk of needle EMG to the EDX consultant includes inadvertent needle puncture of the EDX consultant by the needle used to evaluate
the patient and infection by hepatitis, human immuno-deficiency virus, or other communicable disease.
The AAEM has prepared a document that describes the benefits of electrodiagnostic medicine.
4 Briefly, the benefits of needle EMG and NCS include confirmation of the clinical diagnosis of CTS and the probability of identifying concomitant or alternative neurological disorders as the cause of the patient’s symptoms. In
a prospective study, Haig and colleagues95 reported that an EDX consultation, including EMG and NCS, changed the final clinical diagnosis 42% of the time.
This study has not undertaken a systematic evaluation of the economic
costs and economic benefits of NCSs and needle EMG in the evaluation of patients suspected of CTS. The interested reader is referred to the outcome study by Boniface and colleagues.
20
This report is provided as an educational service of the AAEM. It is based on an assessment of current scientific and clinical information. It is not intended to include all possible methods of care of a particular clinical problem or all legitimate
criteria for choosing to use a specific procedure. Neither is it intended to exclude any reasonable alternative methodologies. The AAEM recognizes that specific patient care decisions are the prerogative of the patient and his/her physician and
are based on all of the circumstances involved.
References
Abbreviations: abductor digiti minimi (ADM); abductor pollicis brevis (APB); compound motor action potential (CMAP); carpal tunnel (CT); carpal tunnel syndrome (CTS); distal motor latency (DML); distal sensory latency (DSL); electromyography (EMG); nerve conduction studies (NCSs); nerve conduction velocity (NCV); sensory nerve action potential (SNAP).
- American Academy of Neurology Quality Standards Subcommittee. Practice parameter for carpal tunnel syndrome. Neurology 1993;43:2406-2409. Background Reference. Source: AAEM 2000 CTS Task Force member. Summary statement that notes that the likelihood of the diagnosis of CTS increases with the number of classic symptoms, provocative factors, mitigating factors, and abnormalities on the physical examination. The clinical investigator can construct a set of clinical criteria for the diagnosis of CTS from these symptoms and signs common to CTS.
- American Association of Electrodiagnostic Medicine. Guidelines in electrodiagnostic medicine. Muscle Nerve 1992;15:229-253. Background Reference. Source: AAEM Consultant 1993.
- American Association of Electrodiagnostic Medicine. Guidelines in electrodiagnostic medicine. Practice parameter for electrodiagnostic studies in carpal tunnel syndrome: summary statement. Muscle Nerve 1999;S8:S141-143. Background Reference. Source: AAEM 2000 CTS Task Force member.
- American Association of Electrodiagnostic Medicine. Guidelines in electrodiagnostic medicine. Referral guidelines for electrodiagnostic medicine consultations. Muscle Nerve 1999;S8:S107-S108. Background Reference. Source: AAEM 2000 CTS Task Force member.
- American Association of Electrodiagnostic Medicine. Guidelines in electrodiagnostic medicine. Risks in electrodiagnostic medicine. Muscle Nerve 1999;S8:S53-S58. Background Reference. Source: AAEM 2000 CTS Task Force member.
- American Association of Electrodiagnostic Medicine. Guidelines in electrodiagnostic medicine. Who is qualified to practice electrodiagnostic medicine? Muscle Nerve 1999;S8:S263-S265. Background Reference. Source: AAEM 2000 CTS Task Force member.
- American Association of Electrodiagnostic Medicine, American Academy of Neurology, American Academy of Physical Medicine and Rehabilitation. Practice parameter for electrodiagnostic studies in carpal tunnel syndrome: summary statement. Muscle Nerve 1993;16:1390-1391. Background Reference. Source: AAEM 2000 CTS Task Force member.
- Anastasopoulos D, Chroni E. Effect of carpal tunnel syndrome on median nerve proximal conduction estimated by F waves. J Clin Neurophysiol 1997;14:63-67. Background Reference. Source: Medline Search. Abstract: Slowing of median nerve proximal motor conduction in patients with carpal tunnel syndrome (CTS) could be considered as an indicator of an additional proximal lesion (double crush syndrome). The effect of CTS on proximal conduction was assessed by comparing motor velocities calculated by F-waves obtained from muscles with the same root and nerve supply but different median branches, one emerging before the carpal tunnel (pronator quadratus muscle) and one passing through the tunnel (abductor pollicis brevis). Data were obtained from 26 patients with CTS and 21 age-matched healthy subjects. In the control group, the proximal (spinal cord and elbow) F-wave maximal velocity calculated when recording from abductor pollicis brevis (FCVmax-APB) was not different from the F-wave maximal velocity calculated when recording from pronator quadratus (FCVmax-PQ), while it was significantly different in the group of CTS patients, especially in patients with terminal motor latency greater than 4.5 ms (approximately 9% less, p = 0.001, Wilcoxon signed rank test). The study showed that median nerve proximal conduction velocity slowing in patients with CTS is restricted to the fibers that distally pass through the carpal tunnel and does not necessarily imply an additional proximal lesion. We suggest that comparison of FCVmaxAPB and FCVmax-PQ could be useful when the question arises if a single (distal) or two (one distal, one proximal) lesions are responsible for a patient’s symptoms.
- Andary MT, Fankhauser MJ, Ritson JL, Spiegel N, Hulce V, Yosef M. Comparison of sensory mid-palm studies to other techniques in carpal tunnel syndrome. Electromyogr Clin Neurophysiol 1996;36:279-285. Criteria Met (5/6: 1,3,4,5,6) Source: Medline Search. Abstract: Prospective study to compare the relative sensitivity of several NCS to identify abnormalities in patients with (1) mild CTS (antidromic median sensory peak latency less than or equal to 4.0 ms (conduction distance 14 cm) and (2) at least one NCS abnormality. Of a total of 205 patients with 275 hands, a study subgroup was selected on the basis of the results of NCS: 81 patients with 90 hands. The data from this subgroup was used to calculate the relative sensitivity of four tests: (1) Median-ulnar sensory latency differences across the wrist (sensory palm [M-U]), (2) Median-radial sensory difference (sensory thumb [M-R]), (3) Median-ulnar mixed palm difference (mix palm [M-U]) and (4) Median-ulnar sensory digit difference (sensory digits [M-U]). 90 hands met the electrodiagnostic (EDX) criteria for mild CTS. The sensory thumb (M-R) was abnormal in 90% of the hands followed in order by mix palm (M-U) 61%, sensory digits (M-U) 42% and sensory palm (M-U) 33%. sensory palm (M-U) did not significantly add to the diagnosis of CTS.
- Ashworth NL, Marshall SC, Satkunam LE. The effect of temperature on nerve conduction parameters in carpal tunnel syndrome. Muscle Nerve 1998;21:1089-1091. Background Reference. Source: Medline Search. Abstract: This study provides evidence that temperature correction factors based on normal nerves from normal individuals cannot be used to normalized NCS data from CTS patients.
- Aurora SK, Ahmad BK, Aurora TK. Silent period abnormalities in carpal tunnel syndrome. Muscle Nerve 1998;21:1213-1215.Criteria Met (3/6: 1,2,5) Source: Medline Search. Abstract: Cutaneous silent period (CSP) was measured on stimulating digits 2 and 5 in 19 patients with carpal tunnel syndrome (CTS) and compared with 20 healthy volunteers. In 2 patients with severe CTS, CSP was absent on digit 2 but present on digit 5. Example of use of CTS as a model for investigating the effect of a compressive neuropathy on the CSP. CSP abnormality does not localized pathology to carpal tunnel segment of the median nerve. 3004
- Baker EL, Ehrenberg RL. Preventing the work-related carpal tunnel syndrome: physician reporting and diagnostic criteria. Ann Intern Med 1990;112:317-319. Background Reference. Source: Medline Search.
- Balbierz JM, Cottrell AC, Cottrell WD. Is needle examination always necessary in evaluation of carpal tunnel syndrome? Arch Phys Med Rehabil 1998;79:514-516. Criteria Met: (2/6: 2,3) Source: Medline Search. Abstract: Retrospective review of EMG/NCS reports to determine if needle EMG evaluation was abnormal if NCS were normal during the evaluation of patients suspected of CTS. In patients in whom only CTS was suspected, normal NCS predicted that EMG would be normal 89.8% of the time. These findings suggest that there may be a subpopulation of patients referred for electrodiagnostic evaluation of CTS who may be adequately evaluated by nerve conduction studies alone.
- Baysal AI, Chang CW, Oh SJ. Temperature effects on nerve conduction studies in patients with carpal tunnel syndrome. Acta Neurol Scand 1993; 88: 213-216. Background Reference. Source: Medline Search. Abstract: Study to determine whether diseased nerves (CTS patients) responded to temperature rise in a different manner from normal controls. With rising temperature motor NCV increased, whereas latencies, amplitudes and duration of the compound muscle action potential decreased in both groups. Although these changes were not statistically significant between the two groups, there was a tendency with temperature changes for the decrease in the terminal latency of the CTS group to be greater than that of normal controls. (See Bolton and Ashworth).
- Bhala RP, Thoppil E. Early detection of carpal tunnel syndrome by sensory nerve conduction. Electromyogr Clin Neurophysiol 1981;21:155-164. Criteria Met (3/6: 1,2,3) Source: Pease, 1989. Abstract: With stimulation at the wrist, antidromic SNAPs were recorded from 50 hands in 25 healthy subjects and 36 hands of 21 CTS patients. DSL, amplitude, and duration of the SNAP were systemically evaluated, they were also compared to DMLs from previous studies. DSL was the most sensitive followed by DML and then duration of SNAP. They report 4 of 36 hands where the only abnormality was duration of SNAP (the statistics suggest that the criteria for abnormality was different for DSL and duration of SNAP).
- Bleecker ML. Medical surveillance for carpal tunnel syndrome in workers. J Hand Surg Am 1987;12(5 Pt 2):845-848. Criteria Met (1/6: 1) Source: Medline Search.
- Bleecker ML, Agnew J. New techniques for the diagnosis of carpal tunnel syndrome. Scan J Work Environ Health 1987;13:385-388. Criteria Met (2/6: 2,3) Source: Medline Search
- Bolton CF, Carter K, Koval JJ. Temperature effects on conduction studies of normal and abnormal nerve. Muscle Nerve 1982;5:S145S147.Background Reference. Source: Medline Search. Abstract: There are significant quantitative differences between normal and abnormal nerves in their response to physiological temperature change. These differences must be recognized if correction factors for temperature are to be used to normalized NCS data from cool limbs.
- *Bonebrake AR, Fernandez JE, Marley RJ, Dahalan JB, Kilmer KJ. A treatment for carpal tunnel syndrome: evaluation of objective and subjective measures. J Manipulative Physiol Ther 1990;13:507-520. Criteria Met (0/6) Source: Medline Search.
- Boniface SJ, Morris I, Macleod A. How does neurophysiological assessment influence the management and outcome of patients with carpal tunnel syndrome? Br J Rheumatol 1994;33:1169-1170. Background Reference: outcome study. Source: Medline Search. Abstract: The objective of this study was to determine how neurophysiological assessment influenced the management and outcome of 100 consecutive patients referred to a department of clinical neurophysiology in a district general hospital with a provisional clinical diagnosis of carpal tunnel syndrome. Nerve conduction studies excluded the diagnosis in 36 patients who may have otherwise received inappropriate treatment. The decision whether to perform a carpal tunnel decompression was greatly influenced by a positive study. Symptoms subsequently resolved in 72-86% of patients treated on this basis, depending on the mode of treatment and the nerve conduction study findings, with similar outcomes for surgical and conservative measures. The clinical and estimated resource implications of this diagnostic service were found to be substantial.
- Borg K, Lindblom U. Diagnostic value of quantitative sensory testing (QST) in carpal tunnel syndrome. Acta Neurol Scand 1988;78:537541. Criteria Met (1/6: 1) Source: Medline Search.
- Borg K, Lindblom U. Increase of vibration threshold during wrist flexion in patients with carpal tunnel syndrome. Pain 1986;26:211219. Criteria Met (2/6: 1,5) Source: Medline Search.
- Brain WR, Wright AD, Wilkinson M. Spontaneous compression of both median nerves in the carpal tunnel. Six cases treated surgically. Lancet 1947;1:277-282. Background Reference. Source: Gelbermann, 1980.
- *Brammer AJ, Pyykklo I. Vibration-induced neuropathy. Detection by nerve conduction measurements. Scand J Work Environ Health 1987;13:317-322. Criteria Met (0/6) Source: Medline Search.
- *Braun RM, Davidson K, Doehr S. Provocative testing in the diagnosis of dynamic carpal tunnel syndrome. J Hand Surgery 1989;14-A (2 Pt 1): 195-197. Criteria Met (2/6: 1,2) Source: Medline Search.
- Bromberg MB, Jaros L. Symmetry of normal motor and sensory nerve conduction measurements. Muscle Nerve 1998;21:498-503. Criteria Met (normal population study 4/6: 3,4,5,6). Source: Medline Search. Abstract: Retrospective study to determine the normal limits of symmetry of NCS measurements. The data support the twofold limit of side-to-side differences for amplitudes of the median and ulnar SNAP and CMAP. There were greater than twofold side-to-side differences for the peroneal, tibial and sural nerve amplitudes.
- Bronson J, Beck J, Gillet J. Provocative motor nerve conduction testing in presumptive carpal tunnel syndrome unconfirmed by traditional electrodiagnostic testing. J Hand Surg [Am ] 1997;22:1041-1046. Criteria Met (3/6: 3,5,6) Source: Medline Search. Abstract: Median distal motor latencies (DML) were measured in hands held in five wrist positions (neutral, flexion, extension, radial deviation, ulnar deviation) just long enough (few seconds) to record a response. The “differential latency” was defined as the difference between the absolute greatest and least median DML recorded in the five hand positions. The authors reported that the mean differential latency in pooled data from both hands of 16 reference subjects (no symptoms, normal NCS, and some with positive Tinel’s sign) was 0.13 ms (mean + 2SD was 0.24 ms) and that there was a very high rate of abnormalities among 22 CTS patients selected with normal (but unspecified) NCS: 91 % had a differential latency above 0.24 ms with the mean 0.44 ms. Three months after surgical release, the mean differential latency of the CTS patients fell within the range of normal. The authors suggest that differential latency measurements compliment standard NCS in the diagnosis of CTS. However, the article contains internal inconsistencies which could not be resolved by inquiry. For example, the authors state that the study was prospective, but entered 22 consecutive patients and all had unilateral CTS. Since CTS is symptomatic bilaterally in approximately 50% of patients, the odds of a random series of 22 consecutive unilateral CTS patients would be less than 1 in 4,000,000. There are statistical concerns that the variance of measurements from control subjects was incorrectly calculated by considering each of the two hands as an independent variable. Furthermore, the results of this report are contrary to other published reports of the effect of brief changes in wrist position on median latency measurements in CTS (see text for discussion of effect of brief and prolonged positioning on median NCS parameters: latency and amplitude.).
- Brown WF, Ferguson GG, Jones MW, Yates SK. The location of conduction abnormalities in human entrapment neuropathies. Can J Neurol Sci 1976;3:111-122. Background Reference. Source: DeLean, 1988.
- Buch-Jaeger N, Foucher G. Correlation of clinical signs with nerve conduction tests in the diagnosis of carpal tunnel syndrome [see comments]. J Hand Surg [Br ] 1994;19:720-724. Background Reference. Source: Medline Search. Abstract: A prospective study 112 patients with symptoms of CTS (172 symptomatic hands) sought correlation with 11 clinical criteria (symptoms and signs) taken either singly or in combination. Analysis of the sensitivity and specificity of various clinical tests and diagnostic maneuvers showed mediocre reliability in establishing the diagnosis of CTS. The authors concluded that NCS are an indispensable part of the evaluation of patients suspected of CTS.
- Buchthal F, Rosenfalck A. Sensory conduction from digit to palm and from palm to wrist in the carpal tunnel syndrome. J Neurol Neurosurg Psychiatry 1971;34:243-252. Criteria Met (6/6: 1,2,3,4,5,6) Source: Nau, 1988. Abstract: With stimulation on the digits (thumb, middle, and little finger with subdermal recording over the median nerve at the palm, wrist and elbow), orthodromic SNAPS were recorded using averaging techniques. Motor responses were evaluated with stimulation at the wrist, and elbow and subdermal recording over the APB. Ten normal subjects and 22 hospitalized patients were evaluated. Focal slowing across the carpal tunnel was seen in some patients with clinical signs of CTS in whom DML and sensory conduction from digit to wrist were normal.
- Buchthal F, Rosenfalck A, Trojaborg W. Electrophysiological findings in entrapment of the median nerve at wrist and elbow. J Neurol Neurosurg Psychiatry 1974;37:340-360. Criteria Met (6/6: 1,2,3,4,5,6) Source: Palliyath, 1990. Abstract: With stimulation on the digits and recording from the palm, wrist, and elbow, orthodromic SNAPS were recorded using subdermal electrodes. Motor responses were recorded by stimulation at the wrist and recording over the APB; 190 normal controls, 117 patients with CTS, and 11 patients with median nerve compression at the elbow were evaluated. Additionally 112 patients were evaluated by needle EMG in the APB. Abnormalities in CTS patients were found in NCSs across the carpal tunnel and relatively spared or normal in other portions of the nerve. There were needle EMG abnormalities in 91% of the CTS patients evaluated (as defined by altered pattern of discharge during full effort, change in mean duration and amplitude of motor unit action potentials, increased incidence of polyphasic potentials, or spontaneous activity).
- Buschbacher RM. Body mass index effect on common nerve conduction study measurements. Muscle Nerve 1998;21:1398-1404. Criteria Met (normal population study 5/6: 1,3,4,5,6) Source: Bushbacher 1999 monograph. Abstract: Study performed to determine effect of body fat on NCS parameters. There was no correlation between Body Mass Index and conduction velocities but sensory/mixed nerve amplitudes were 20-40% lower in the obese compared to thin subjects.
- Buschbacher RM. Median 14-cm and 7-cm antidromic sensory studies to digits two and three. Am J Phys Med Rehabil 1999;78:S53S62. Criteria Met (normal population study 5/6: 1,3,4,5,6) Source: Medline Search identified Bushbacher 1999 Monograph. Abstract: The purpose of the study was to create a large database of normal values for the antidromic median sensory conduction to D2 and D34 with stimulation at the wrist (14 cm) and palm (7 cm) bilaterally in 258 normal subjects. Analysis of variance demonstrated that increasing age and increasing body mass index correlated with decreasing amplitudes and area. For peak latency measurements, 50% of the 14 cm latency was attributed to the wrist-to-palm segment. The upper limit of normal increase in amplitude from wrist-to-palm stimulation is 50-55%.
- Buschbacher RM. Median nerve motor conduction to the abductor pollicis brevis. Am J Phys Med Rehabil 1999;78:S1-S8. Criteria Met (normal population study 5/6: 1,3,4,5,6) Source: Medline Search identified Bushbacher 1999 Monograph. Abstract: The purpose of the study was to create a large database of normal values for the median motor conduction to the APB including the amplitude (10.2 ± 3.6 mv), distal latency (3.7 ± 0.5 ms) and conduction velocity (57 ± 5 m/s). Analysis of variance demonstrated that age affects the distal latency, amplitude, area and forearm NCV. Gender affects distal latency and forearm NCV. Height has no significant effect on any of these measurements.
- Buschbacher RM. Median nerve F-wave latencies recorded from the abductor pollicis brevis. Am J Phys Med Rehabil 1999;78:S32-S37. Criteria Met (normal population study 5/6: 1,3,4,5,6) Source: Medline Search identified Bushbacher 1999 Monograph. Abstract: The purpose of the study was to create a large database of normal values for the median F-waves by analysis of F-wave responses from the APB to ten consecutive supramaximal stimuli applied to the wrist of each arm of 195 asymptomatic subjects without risk factors for neuropathy. An analysis of variance demonstrated that the minimum and mean F wave latentcies are dependent on age, gender and height.
- Buschbacher RM. Mixed nerve conduction studies of the median and ulnar nerves. Am J Phys Med Rehabil 1999;78:S69-S74. Criteria Met (normal population study 5/6: 1,3,4,5,6) Source: Medline Search. Abstract: Normal data from a reference population of 248 subjects, age range 19-79 yr, 45% males tested bilaterally for median and ulnar mixed nerve orthodromic conduction study across the wrist (conduction distance 8-cm) and the differences in latencies (onset and peak) for both studies. For both median and ulnar nerves, the mean onset latency was 1.6 ± 0.2 ms, and the mean peak latency was 2.1 ± 0.2 ms. Mean side-to-side difference for the median and ulnar onset and peak latencies was 0.0 ± 0.2 ms. The mean difference between onset and peak latencies between the nerves was 0.0 ± 0.2 ms. Because the stimulus artifact may obscure the onset in some cases, the peak latency is the preferred value. Amplitude measurements, but not latency measurements, were dependent on age, gender and body mass index (measure of obesity).
- Cannon BW, Love JG. Tardy median palsy; median neuritis; median themar neuritis amenable to surgery. Surgery 1946;20:210-216. Background Reference. Source: Gelbermann, 1980.
- Carroll G. Comparison of median and radial nerve sensory latencies in the electrophysiological diagnosis of carpal tunnel syndrome. Electroencephalogr Clin Neurophysiol 1987;68:101-106. Criteria Met (6/6: 1,2,3,4,5,6) Source: Medline Search. Abstract: With stimulation on index finger and thumb, orthodromic SNAPS were recorded at the wrist in 100 healthy hands and 161 CTS hands. When differences in the distal latencies between the median and radial nerves were used as abnormal, 60% sensitivity was obtained. The median-radial comparison increased the yield of abnormalities in 17 of 161 hands when compared to the index DSL latency alone.
- Casey EB, LeQuesne PM. Digital nerve action potentials in healthy subjects, and in carpal tunnel and diabetic patients. J Neurol Neurosurg Psychiatry 1972;35:612-623. Criteria Met (6/6: 1,2,3,4,5,6) Source: Palliyath, 1990. Abstract: With stimulation of the middle finger, median sensory nerve conduction velocities were calculated from the onset and peak latencies of SNAPs recorded from the wrist and proximal phalanx with surface electrodes. The conduction velocities of both the digit-wrist and distal-proximal digit segments were reduced uniformly in 18 patients with diabetic polyneuropathy. In contrast, the conduction velocity of the distalproximal digit segment was often normal while the conduction velocity of the digit-wrist segment was reduced in 16 CTS patients.
- *Cassvan A, Ralescu S, Shapiro E, Moshkovski FG, Weiss J. Median and radial sensory latencies to digit I as compared with other screening tests in carpal tunnel syndrome. Am J Phys Med Rehabil 1988; 67:221-224. Criteria Met (3/6: 1,3,5) Source: Medline Search.
- *Cassvan A, Rosenberg A, Rivera LF. Ulnar nerve involvement in carpal tunnel syndrome. Arch Phys Med Rehabil 1986;67:290-292. Criteria Met (1/6: 3) Source: Medline Search.
- *Chang CW, Lien IN. Comparison of sensory nerve conduction in the palmar cutaneous branch and first digital branch of the median nerve: a new diagnostic method for carpal tunnel syndrome. Muscle Nerve 1991;14:1173-1176. Criteria Met (5/6: 1,2,3,5,6) Source: Medline Search. Abstract: Comparison of orthodromic SNC in the median palmar cutaneous branch and digit I nerves was evaluated in 50 CTS patients and 40 healthy persons. The abnormalities were defined as the differences in latencies and SNCVs of more than mean plus 2.5SD of controls. Abnormalities were noted in 84% (36 of 43 patients) of the sensory latency comparisons and 77% (33 of 43 patients) of the SNCVs comparisons after exclusion of 7 CTS patients whose D1 SNAP was unobtainable. This method may serve as an adjunctive technique in the diagnosis of CTS.
- Chang MH, Chiang HT, Ger LP, Yang DA, Lo YK. Clin Neurophysiol 2000;111:1039-1044. The cause of slowed forearm median conduction velocity in carpal tunnel syndrome. Criteria Met (5/6: 1,3,4,5,6) Source: Medline Search. Abstract: A prospective study of 20 CTS patients with slowing (<50 m/s) of forearm conduction velocity (CV), 35 CTS patients with normal (>50 m/s) forearm CV and 20 normal control subjects. Median motor nerve CV was calculated from the results of recordings from the APB with stimulation at the wrist, elbow, mid-arm and axilla. The authors hypothesized that if the slowing of forearm CV was due to conduction block of large myelinated fibers at the wrist, median forearm CV and also proximal median CV would be decreased. However, the reduced median CV was limited to the forearm segment. The authors concluded that the data indicated that slowing of median forearm CV in CTS is due to retrograde axonal atrophy rather than conduction block.
- Chang MH, Liao KK, Chang SP, Kong KW, Cheung SC. Proximal slowing in carpal tunnel syndrome resulting from either conduction block or retrograde degeneration. J Neurol 1993;240:287-290. Criteria Met (4/6: 1,3,4,6) Source: Medline Search. Abstract: Decreased CV in the median nerve forearm segment has been documented by standard NCS in CTS patients. A new technique modified from the method of Stoehr et al. and Pease et al. was used to determine the forearm median nerve action potentials (FNAP) amplitude and forearm nerve conduction velocity (FNCV) proximal to the wrist. Age matched subjects with non-specific numbness referred to the laboratory and patients with CTS were studied by both standard NCS and the new FNAP methods. CTS patients were divided into subgroups according to the severity of abnormalities on standard median sensory and motor NCS. There was a significant decrease in FNAP amplitudes proportional to severity of the CTS, but FNCV was reduced to a lesser extent. In addition, the standard forearm median motor CV (MMCV) correlated well with severity, but the reduced MMCV did not correlate with the decreased FNCV. We interpreted these findings to indicate that the reduced forearm MMCV in CTS results primarily from the block of the faster conducting median motor nerve fibers at the wrist rather than from retrograde degeneration of median motor nerve fibers.
- Charles N, Vial C, Chauplannaz G, Bady B. Clinical validation of antidromic stimulation of the ring finger in early electrodiagnosis of mild carpal tunnel syndrome. Electroencephalogr Clin Neurophysiol 1990;76:142-147. Criteria Met (4/6: 1,3,5,6) Source: Medline Search. Abstract: The following techniques were studied: (a) orthodromic stimulation of the index finger with recording over the median nerve at the wrist, (b) antidromic SNAPs were recorded over the ring finger using ring electrodes after stimulation of the median nerve and then the ulnar nerve at the wrist, (c) DSL difference by subtracting the ulnar DSL to the ring finger from the median DSL to the ring finger, and (d) median DML with stimulation at the wrist and recording over APB. Three different groups were studied: (1) the control group with 100 hands in 60 healthy subjects; (2) 224 hands from 158 potential CTS patients; and (3) 30 hands from 30 patients with parasthesias into the middle and index fingers due to cervical spondylitic radiculopathy. They found the median-ulnar DSL difference to the ring finger the most sensitive technique followed in order by the median sensory NCV to ring finger, median sensory NCV to index finger and median DML. They report no differences between the cervical spondylitic radiculopathy group and the normal group and found no cases of abnormal median-ulnar DSL differences to the ring finger in this group (no false positives). They also report that amplitude was not a reliable parameter for the diagnosis of CTS.
- *Cho DS, MacLean IC. Comparison of normal values of median, radial and ulnar sensory latencies. Muscle Nerve 1984;7:575. Criteria Met (0/6) (Abstract Only) Source: Redmond, 1988.
- Cioni R, Passero S, Paradiso C, Giannini F, Battistini N, Rushworth G. Diagnostic specificity of sensory and motor nerve conduction variables in early detection of carpal tunnel syndrome. J Neurol 1989;236:208-213. Criteria Met (6/6: 1,2,3,4,5,6) Source: Medline Search. Abstract: The median, radial, and ulnar nerves were stimulated at the wrist at the horizontal line of the radial styloid and SNAPs were recorded over each finger in 375 abnormal and 56 control hands. Absolute latencies of the median nerve to thumb, index and ring fingers were recorded. Ratios comparing the median nerve to either the radial nerve or ulnar nerve were also evaluated. Using clinical criteria for the definition of CTS, they found abnormal sensory NCVs to the ring finger at 100%, middle finger 92%, index finger 80%, and thumb 64%. Amplitudes of the sensory responses were not sensitive. The ratio of latencies median index/ulnar little finger was abnormal in 93.9%, median ring/ulnar ring 95.5%, and median thumb / radial thumb 82.8%.
- Clifford JC, Israels H. Provocative exercise maneuver: its effect on nerve conduction studies in patients with carpal tunnel syndrome. Arch Phys Med Rehabil 1994;75:8-11. Criteria Met (6/6: 1,2,3,4,5,6) Source: Medline Search. Abstract: Prospective study of 10 normal controls and 20 patients with clinical symptoms of CTS whose work involved repetitive movements: 10 of the 20 CTS patients had abnormal median NCS which confirmed the presence of median nerve pathology in the carpal tunnel segment. The study evaluated the effect of dynamic exercise on antidromic median (wrist to thumb and to D4) and antidromic radial (wrist to thumb) sensory nerve conduction. The dynamic exercise consisted of 2 min of repetitive wrist flexion and extension through a full active range over a 2 s cycle followed immediately by full active finger flexion and extension of a 3 s cycle for an addition 2 min. The exercise protocol was sufficient to evoke symptom exacerbation in 50% of the CTS patients. The 4 minutes of dynamic exercise produced a statistically significant (p <.05) prolongation of only the median SNAP latency to D4, but the difference was too small to discriminate individual CTS patients from control subjects. There was no increase in the distal sensory latencies of those patients whose symptoms were exacerbated, when compared with those patients whose symptoms remained unchanged. The authors concluded that there was little value in performing the dynamic exercise testing to increase the laboratory diagnosis of CTS.
- *Cruz Martinez A. Diagnostic yield of different electrophysiological methods in carpal tunnel syndrome (letter to editor). Muscle Nerve 1991;14:183-184. Criteria Met (3/6: 1,2,3) Source: Medline Search.
- Cruz Martinez A, Barrio M, Perez Conde MC, Gutierrez AM. Electrophysiological aspects of sensory conduction velocity in healthy adults. J Neurol Neurosurg Psychiatry 1978;41:1092-1096. Criteria Met (4/6: 1,3,5,6) Source: Valls, 1988. Abstract: In 47 healthy subjects, the median and ulnar nerve conduction velocity was measured from digit to palm and from palm to wrist. Ulnar nerve conduction velocity from wrist to below sulcus and from below sulcus to above sulcus. NCVs for each segment were determined from measurements of the onset latency (personal communication). The results suggest that aging causes a decrement in conduction velocity and changes the shape of evoked potentials, especially at points where nerves are frequently compressed (carpal tunnel and cubital tunnel). No CTS patients were studied.
- Cuturic M, Palliyath S. Motor unit number estimate (MUNE) testing in male patients with mild to moderate carpal tunnel syndrome. Electromyography and Clin Neurophys 2000;40:67-72. Criteria Met (4/6: 1,3,5,6) Source: Medline Search. Abstract: Motor unit number estimate (MUNE) testing of the APB muscle of CTS patients with “mild” to “moderate” CTS identified by abnormal median sensory and motor NCS. Compared to 16 control subjects, 14 of the 19 CTS patients with abnormal needle EMG findings in the APB had a reduced mean MUNE. The mean MUNE was within normal limits in CTS patients with prolonged distal motor latencies or prolonged F wave latencies and normal needle EMG findings in the APB. Curiously, 8 of the 19 CTS patients had abnormalities on the needle EMG of the cervical paraspinal muscles which the authors interpreted as evidence of a concomitant C8 radiculopathy and this group of CTS patients also had lower mean MUNE values compared to the control subjects.
- Daube JR. Percutaneous palmar median nerve stimulation for carpal tunnel syndrome, abstract. Electroencephalogr Clin Neurophysiol 1977;43:139-140. Criteria Met (0/6) (Abstract Only) Source: Palliyath, 1990.
- Dawson GD. The relative excitability and conduction velocity of sensory and motor nerve fibers in man. J Physiol 1956;131:436-451. Background Reference. Source: Gilliatt, 1978.
- Dawson GD, Scott JW. The recording of nerve action potentials through the skin in man. J Neurol Neurosurg Psychiatry 1949;12:259267. Background Reference. Source: Mills, 1985.
- de Krom MC, Knipschild PG, Kester AD, Spaans F. Efficacy of provocative tests for diagnosis of carpal tunnel syndrome [see also comment in Lancet 1990;335:727]. Lancet 1990;335:393-395. Background Reference. Source: Medline Search. Abstract: Twelve clinical provocative tests for CTS (Tinel, Phalen, etc.) demonstrated low sensitivity and specificity for the diagnosis of CTS (as determined by abnormal median NCSs) in a random sample of 504 people from the general population.
- De Smet L, Steenwerckx A, Van den Bogaert G, Cnudde P, Fabry G. Value of clinical provocative tests in carpal tunnel syndrome. Acta Orthop Belg 1995;61:177-182. Background Reference. Source: Medline Search. Abstract: Prospective study of CTS patients, normal controls, and disease (diabetes) controls of the usefulness of five clinical provocative tests (Tinel, Phalen, Durkan, closed fist, Gilliatt) to diagnose CTS. Results of study led to a recommendation that surgeons use the results of median NCS studies in addition to clinical findings (1) to make the diagnosis of CTS and (2) to assist in decision to perform CTS surgery.
- DeLean J. Transcarpal median sensory conduction: detection of latent abnormalities in mild carpal tunnel syndrome. Can J Neurol Sci 1988;15:388-393. Criteria Met (6/6: 1,2,3,4,5,6) Source: Medline Search. Abstract: Median sensory studies were performed with stimulation over the index or middle finger and recording with subdermal electrodes at the midpalm and wrist over the median nerve; median motor conduction studies were performed with surface stimulation and recording electrodes over the APB in 80 hands from 43 healthy volunteers and 253 hands from 150 CTS patients. They found abnormalities in 63% of the CTS patients. Palmar latencies were most likely to be abnormal, then wrist DSLs, and finally, wrist DML.
- Di Benedetto M, Mitz M, Klingbeil GE, Davidoff D. New criteria for sensory nerve conduction especially useful in diagnosing carpal tunnel syndrome. Arch Phys Med Rehabil 1986;67:586-589. Criteria Met (normal population study 5/6: 1,3,4,5,6) Source: Medline Search. Abstract: This paper reports normal values in 45 hands of 30 healthy adults with careful attention to temperature and distance measurements. Antidromic and orthodromic SNAPs from median, ulnar and radial nerves, wrist-to-thumb, wrist-to-index finger, wristto-middle finger, wrist-to-ring finger, and palm-to-wrist. Latencies to onset, negative peak, amplitude, 2 measures of duration, and normal values for side-to-side differences are reported. No CTS patients were studied.
- Di Guglielmo G, Torrieri F, Repaci M, Uncini A. Conduction block and segmental velocities in carpal tunnel syndrome. Electroencephalogr Clin Neurophysiol 1997;105:321-327. Criteria Met (6/6: 1,2,3,4,5,6) Source: Medline Search. Abstract: Conventional median sensory and motor conduction studies of CTS do not determine whether low amplitude responses are due to axonal degeneration or demyelination in the carpal tunnel segment of the median nerve. In 88 control and 294 CTS hands we recorded amplitude and duration of the APB CMAP and of antidromic SNAP after wrist and palm stimulation to determine wrist to palm amplitude and duration ratios and segmental conduction velocities. In 16% of CTS hands there was an abnormal amplitude reduction without increased duration of CMAP or SNAP from wrist stimulation indicating partial conduction block in the carpal tunnel segment of the median nerve. In 148 hands distal motor latency to abductor pollicis brevis and/or sensory conduction to digit 2 were abnormal. In the remaining 146 hands wrist to palm motor conduction was less than 35 m/s in 22.6% and wrist to palm sensory conduction was less than 45 m/s in 13%. At least one segmental conduction was abnormal in 27% of hands. Segmental studies allow the discrimination between conduction block and axonal degeneration, increase diagnostic yield in CTS, and might be useful in addressing treatment and predicting outcome.
- Donahue JE, Raynor EM, Rutkove SB. Forearm velocity in carpal tunnel syndrome: when is slow too slow? [published erratum appears in Arch Phys Med Rehabil 1998;79:723. Arch Phys Med Rehabil 1998;79:181-183. Criteria Met (3/6: 3,4,6) Source: Medline Search. Abstract: In cases of CTS, the finding of moderate to severe slowing of median motor forearm conduction velocity (<47 m/s) should prompt a careful evaluation to exclude superimposed proximal median nerve pathology or polyneuropathy.
- Dorfman LJ, Robinson LR. AAEM Minimonograph #47: Normative data in electrodiagnostic medicine. Muscle Nerve 1997;20:4-14. Background Reference. Source: Buschbacher, 1999. Abstract: This article reviews, without mathematics, the important principles governing the acquisition and use of normative data in electrodiagnostic medicine.
- Dunnan JB, Waylonis GW. Wrist flexion as an adjunct to the diagnosis of carpal tunnel syndrome. Arch Phys Med Rehabil 1991;72:211-213. Criteria Met (2/6: 1,3) Source: Medline Search.
- Editorial. Diagnosis of the carpal tunnel syndrome. Lancet 1985;1(8433):854-855. Criteria Met (0/6) Source: Golding, 1986.
- Eisen A, Schulzer M, Pant B, MacNeil M, Stewart H, Trueman S, Mak E. Receiver operating characteristic curve analysis in the prediction of carpal tunnel syndrome: a model for reporting electrophysiological data. Muscle Nerve 1993;16:787-796. Criteria Met (4/6: 2,3, 5,6). Source: Medline Search. Abstract: Receiver operating characteristic (ROC) curves were used to predict the risk of CTS. Patients were classified clinically as (1) normal exam and no symptoms (169 hands); (2) having motor and/or sensory deficit typical of CTS (115 hands); (3) having a history characteristic of CTS (156 hands); and (4) non-diagnostic symptomatology (122 hands). Measurements were made of median and ulnar distal motor latency (DML), median and ulnar sensory peak latency (orthodromic 14 cm), and median and ulnar mixed palmar latency (orthodromic 8 cm). Differences between median and ulnar mixed palmar latency were calculated. Median DML combined with median-ulnar palmar latency differences discriminate over other measurements and correlated highly for all groups (r values = 0.71-0.73). These variables were used to construct ROC curves and prediction tables. The approach used allows one to assign a percentage risk of having CTS and can be used n outcome studies.
- Eklund G. A new electrodiagnostic procedure for measuring sensory nerve conduction across the carpal tunnel. Ups J Med Sci 1975;80:6367. Criteria Met (0/6) Source: Macleod, 1987.
- Evans BA, Daube JR. A comparison of 3 electrodiagnostic methods of diagnosing carpal tunnel syndrome. Muscle Nerve 1984;7:565. Criteria Met (2/6: 1,2) [Abstract only] Source: Redmond, 1988.
- *Feierstein MS. The performance and usefulness of nerve conduction studies in the orthopedic office. Orthop Clin North Am 1988;19:859866. Criteria Met (0/6) Source: Medline Search.
- Felsenthal G. Comparison of evoked potentials in the same hand in normal subjects and in patients with carpal tunnel syndrome. Am J Phys Med 1978b;57:228-232. Criteria Met (3/6: 3,5,6) Source: Jackson, 1989.
- Felsenthal G. Median and ulnar distal motor and sensory latencies in the same normal subject. Arch Phys Med Rehabil 1977;58:297-302. Criteria Met (normal population study 4/6: 1,3,5,6) Source: Jackson, 1989. Abstract: The following techniques were studied in 50 normal subjects: (a) median DML after stimulation at the wrist and recording over APB, (b) ulnar DML after stimulation at the wrist and recording over abductor digiti minimi, (c) median DSL with stimulation at the wrist and recording with ring electrodes over the index finger and (d) ulnar DSL after stimulation at the wrist and recording with ring electrodes over the little finger. Additionally, side-to-side differences and median-ulnar latency differences are reported. No data on CTS patients is reported.
- Felsenthal G. Median and ulnar muscle and sensory evoked potentials. Am J Phys Med 1978a;57:167-182. Criteria Met (normal population study 4/6: 1,3,5,6) Source: Jackson, 1989. Abstract: The following techniques were studied in 50 normal subjects: (a) CMAP potentials were recorded after stimulation at the wrist and recording over the APB, (b) CMAPs were recorded from the abductor digiti minimi after stimulation of the ulnar nerve at the wrist, (c) SNAPs were recorded from the index finger after stimulation from the median nerve at the wrist, and (d) SNAPs were recorded from ring electrodes from the little finger after ulnar nerve stimulation at the wrist. Amplitudes of the CMAP and SNAPs are reported and left-to-right comparisons and median-to-ulnar comparisons are reported. No CTS patients were studied.
- Felsenthal G, Spindler H. Palmar conduction time of median and ulnar nerves of normal subjects and patients with carpal tunnel syndrome. Am J Phys Med 1979;58:131-138. Criteria Met (5/6: 1,2,3,5,6) Source: Redmond, 1988. Abstract: With stimulation at the wrist and palm, antidromic SNAP latencies were determined for the median and ulnar nerves from 60 hands in 30 normal subjects and 33 patients with CTS. They found that both the absolute median wrist-topalm conduction time and the median ulnar wrist-to-digit comparison were more sensitive than the median wrist-to-digit latency. The latency ratio comparing median wrist-to-palm and wrist-to-digit latency was too variable to be useful in the diagnosis of CTS.
- *Ferry S, Pritchard T, Keenan J, Croft P, Silman AJ. Estimating the prevalence of delayed median nerve conduction in the general population [see comments]. Br J Rheumatol 1998;37:630-635. Criteria Met (4/6: 1,2,4,6). Source: Medline Search. Abstract: The objective of this study was to determine the point prevalence of delayed median nerve conduction at the wrist as determined by published criteria in a random sample of the general population. The details of the median NCS in the article were not sufficient to permit reproduction of the study. Non-response to the questionnaire and non- attendance for nerve conduction testing may have biased the prevalence estimates. After adjustment for such biases, a prevalence estimate for delayed median nerve conduction of between 7 and 16% was obtained, varying with the different latency values used to define delayed median nerve conduction. Those with hand symptoms consistent with CTS only explained 20% of all subjects with prolonged median nerve latency values. The authors concluded that delayed median nerve conduction across the wrist is not uncommon in the general population. A subsequent letter to the editor pointed out that the authors did not measure ulnar nerve conduction so that the clinical significance of the delayed median nerve conduction is not clear. In addition, this was a cross-sectional study so that the subsequent development of CTS symptoms in subjects with delayed median nerve latency values would not have been detected.
- Fisher MA, Hoffen B. F-wave analysis in patients with carpal tunnel syndrome. Electromyogr Clin Neurophysiol 1997;37:27-31. Criteria Met (4/6: 1,3,5,6) Source: Medline Search. Abstract: The carpal tunnel syndrome (CTS) provides a model for analyzing the effects of focal nerve injury on F-waves. Twenty-four patients with clinical and electrodiagnostic features for unilateral (5) or bilateral CTS (19) were studied. F-waves were evaluated following 20 supramaximal stimuli and recording from abductor pollicis brevis muscles. Minimal and mean latencies, persistences, chronodispersion (CD), mean F/M amplitude ratios, and repeater waves were evaluated. CD’s in those limbs with the most prolonged distal motor latencies (DML) were significantly greater than in those with less prolonged DML’s; 80% or greater repeater waves were found almost exclusively in those hands with decreased M-wave amplitudes; and mean F/M values were almost always larger in the hand with the more prolonged DML. The data support differing effects of demyelinating and axonal injury on F-waves and suggest physiological compensation in those hands with the more pronounced neuropathic dysfunction.
- Fitz WR, Mysiw WJ, Johnson EW. First lumbrical latency and amplitude. Control values and findings in carpal tunnel syndrome. Am J Phys Med Rehabil 1990;69:198-201. Criteria Met (5/6: 1,3,4,5,6) Source: Medline Search. Abstract: With stimulation at the wrist, CMAPs were recorded from the first lumbrical and APB from 44 healthy adults and 36 patients with CTS. Sensory latencies were also recorded, but not systematically reported. In CTS patients, 8% had an abnormal DML to the lumbrical with a normal DML to the APB. They did not find any cases where the latency to the lumbrical was abnormal and sensory studies were normal.
- Foresti C, Quadri S, Rasella M, Tironi F, Viscardi M, Ubiali E. Carpal tunnel syndrome: which electrodiagnostic path should we follow? A prospective study of 100 consecutive patients. Electromyogr Clin Neurophysiol 1996;36:377-384. Criteria Met (4/6: 1,3,5,6) Source: Medline Search. Abstract: Based on written communications, it was learned that this was a prospective study of 6 different motor and sensory electrodiagnostic tests on both hands of 100 patients and on 25 healthy subjects. Reference values obtained from other sources if the reference values obtained from the health subjects in the study were “too far” from reference values previously adopted by the laboratory.
- Fullerton PM. The effect of ischaemia on nerve conduction in the carpal tunnel syndrome. J Neurol Neurosurg Psychiatry 1963;26:385397. Background Reference. Source: Gilliatt, 1990.
- Gelberman RH, Aronson D, Weisman MH. Carpal tunnel syndrome: Results of a prospective trial of steroid injection and splinting. J Bone Joint Surg 1980;62a:1181-1187. Criteria Met (2/6: 1,6) Source: Borg, 1986.
- Gelberman RH, Hergenroeder PT, Hargens AR, Lundborg GN, Akeson WH. The carpal tunnel syndrome: A study of carpal canal pressures. J Bone Joint Surg 1981;63-A:380-383. Criteria Met (0/6) Source: Rojviroj, 1990.
- Gelberman RH, Rydevik BL, Pess GM, Szabo RM, Lundborg G. Carpal tunnel syndrome: a scientific basis for clinical care. Orthop Clin North Am 1988;19:115-124. Background Reference. Source: AAEM 2000 CTS Task Force member.
- Gellman H, Gelberman RH, Tan AM, Botte MJ. Carpal tunnel syndrome. An evaluation of the provocative diagnostic tests. J Bone Joint Surg Am 1986;68:735-737. Criteria Met (1/6: 1) Source: Medline Search.
- *Ghavanini MR, Kazemi B, Jazayeri M, Khosrawi S. Median-radial sensory latencies comparison as a new test in carpal tunnel syndrome. Electromyogr Clin Neurophysiol 1996;36:171-173. Criteria Met (2/6: 2,3) Source: Medline Search.
- Gilliatt RW. Chronic nerve compression and entrapment. In: Sumner AJ, editor. The physiology of peripheral nerve disease. Philadelphia: WB Saunders; 1980. pp 316-339. Background Reference. Source: Lundborg, 1986.
- Gilliatt RW. Sensory conduction studies in early recognition of nerve disorders. Muscle Nerve 1978;1:352-359. Background Reference. Source: Kimura, 1979.
- Gilliatt RW, Meer J. The refractory period of transmission in patients with carpal tunnel syndrome. Muscle Nerve 1990;13:445-450. Criteria Met (4/6: 1,3,4,5) Source: Medline Search. Abstract: With stimulation at the wrist and recording at the finger and elbow, the refractory period of transmission (RPT) was determined between 2 successive shocks by using averaging and signal subtraction techniques. Fourteen hands from 10 CTS patients and 15 control subjects were evaluated. The RPT was abnormal in 11 out of 14 CTS patients.
- Gilliatt RW, Sears TA. Sensory nerve action potentials in patients with peripheral nerve lesions. J Neurol Neurosurg Psychiatry 1958;21:109-118. Background Reference. Source: Stevens, 1987.
- Gilliatt RW, Wilson TG. A pneumatic-tourniquet test in the carpal tunnel syndrome. Lancet 1953;2:595-597. Criteria Met (0/6) Source: Gellman, 1986.
- Gnatz SM, Conway RR. The role of needle electromyography in the evaluation of patients with carpal tunnel syndrome. Muscle Nerve 1999;22:282-286. Background Reference. Editorial. Source: Medline Search. Pros: (1) Identify other nerve pathology which may mimic CTS, e.g. (a) proximal median neuropathy with accompanying slowing of median nerve conduction across the CT and (b) cervical radiculopathy with normal median NCS and (2) identify coexisting cervical radiculopathy with CTS with abnormal median NCS. Cons: In absence of clinical suspicion that there is nerve pathology proximal to CT, it is unclear how the needle EMG examination changes the course of management of a CTS patient.
- Golding DN, Rose DM, Selvarajah K. Clinical tests for carpal tunnel syndrome: An evaluation. Br J Rheumatol 1986;25:388-390. Criteria Met (2/6: 1,3) Source: Medline Search.
- Gordon C, Bowyer BL, Johnson EW. Electrodiagnostic characteristics of acute carpal tunnel syndrome. Arch Phys Med Rehabil 1987;68:545-548. Criteria Met (0/6) Source: Pease, 1988.
- Gordon C, Johnson EW, Gatens PF, Ashton JJ. Wrist ratio correlation with carpal tunnel syndrome in industry. Am J Phys Med Rehabil 1988;67:270-268. Criteria Met (3/6: 1,3,5) Source: Medline Search.
- Gunnarsson LG, Amilon A, Hellstrand P, Leissner P, Philipson L. The diagnosis of carpal tunnel syndrome. Sensitivity and specificity of some clinical and electrophysiological tests. J Hand Surg [Br ] 1997;22:34-37. Criteria Met (4/6: 1,3,4,6) Source: Medline Search. Abstract: Clinical (history, clinical exam, hand diagram) and NCS studies were performed blinded from each other on 100 persons referred with suspected CTS. The diagnosis of CTS was based on the results of both clinical exam and NCS, and, in addition, relief of CTS symptoms after surgery was also required. The sensitivity and specificity for the combined results of the clinical examinations were 94% and 80% respectively, and for the neurophysiological examinations, 85% and 87%. Of the neurophysiological methods used, the quotient of sensory nerve conduction velocity between palm to wrist and wrist to elbow was most sensitive and specific and the cut-off for this test was studied by means of an ROC-curve. Electrodiagnostic studies were (1) more specific than clinical findings and (2) are particularly useful to identify CTS suspects if there is a history of pain, atypical symptoms or previous fractures in the arm, wrist or hand.
- Gutmann L. Median-ulnar communications and carpal tunnel syndrome. J Neurol Neurosurg Psychiatry 1977;40:982-986. Criteria Met (1/6: 3) Source: Gutmann, 1986.
- Gutmann L, Gutierrez A, Riggs J. The contribution of median-ulnar communications in diagnosis of mild carpal tunnel syndrome. Muscle Nerve 1986;9:319-321. Criteria Met (1/6: 3) Source: Rivner, 1991.
- *Hagberg M, Nystrom A, Zetterlund B. Recovery from symptoms after carpal tunnel syndrome surgery in males in relation to vibration exposure. J Hand Surg Am 1991;16:66-71. Criteria Met (1/6: 4) Source: Medline Search.
- Haig AJ, Tzeng HM, LeBreck DB. The value of electrodiagnostic consultation for patients with upper extremity nerve complaints: a prospective comparison with the history and physical examination. Arch Phys Med Rehabil 1999;80:1273-1281. Background Reference. Source: Medline Search. Abstract: Prospective study to determine whether electrodiagnostic testing changes diagnostic certainty compared with a detailed history and physical examination, and whether interactions between medical information, the extent of testing, and diagnostic certainty imply a need for advanced medical knowledge on the part of the examiner. Two hundred fifty-five consecutive referrals for upper extremity nerve complaints were subjects of the study. Diagnosis, diagnostic confidence, and severity of neurologic lesion were coded after standardized history and physical and again after electrodiagnostic testing was completed. Electrodiagnostic testing substantially altered 42% of diagnoses, confirmed 37%, and did not clarify 21%. The extent of testing correlated with the size of the differential diagnosis, the number of previous hospitalizations, and the number of other medical problems. Confidence in final diagnoses correlated positively with severity of the lesion, but negatively with the size of the differential diagnosis and the number of painful body areas. Hospitalizations and medical problems also tended towards negative correlations. This study, in which all electrodiagnostics, histories, and physical examinations were performed by a single physician, indicates that electrodiagnosis substantially alters clinical impressions in a large percentage of patients. The complex relationship between clinical information, the extent of testing, and final diagnostic certainty indicates that specialized medical knowledge is required for accurate electrodiagnosis.
- Hansson S. The association between nerve conduction velocity and the compound action potential amplitude during ischemic blocking. Electromyogr Clin Neurophysiol 1999;39:113-122. Criteria Met (3/6: 1,3,4) Source: Medline Search. Abstract: Ischemia was produced by inflating a tourniquet around the upper arm in five healthy subjects. When antidromic median sensory NCV and SNAP amplitudes were recorded from the third digit with stimulation at the elbow, wrist and palm, the amplitude and CV decreased in parallel. This sequence of changes duplicates the blocking of nerve conduction during wrist flexion in healthy subjects and CTS patients described previously (Hansson 1995).
- Hansson S, Nilsson BY. Median sensory nerve conduction block during wrist flexion in the carpal tunnel syndrome. Electromyogr Clin Neurophysiol 1995;35:99-105. Criteria Met (5/6: 1,2,3,5,6) Source: Medline Search. Abstract: Prospective study of the effect of prolonged passive wrist flexion on median and ulnar sensory amplitude and latency in 10 normal controls and 30 CTS patients with a clinical diagnosis of CTS of whom 10 had mild abnormalities of median sensory latency measurements: digit wrist CV <45 m/s or median-ulnar latency difference from 4th digit to wrist >0.4 ms. During prolonged (up to 45 min) passive wrist flexion, the antidromic median (wrist to 2nd finger) and ulnar (wrist to 5th finger) SNAP were recorded. The measurements were made every 2.5 min during sustained passive wrist flexion for up to 45 min and the time (T50) for the amplitude to fall to 50% of the initial amplitude determined. The median sensory conduction (but not the ulnar) became partially blocked in all CTS patients and also in 8 out of 10 controls. Median sensory nerve conduction returned to normal in all subjects 30 seconds after release of flexion. At 10 minutes of wrist flexion, no significant increase of the median SNAP peak latency in normal subjects (mean 0.01 ± 0.04 ms) and CTS patients (mean 0.24 ± 0.26 ms) was noted. The time (T50) necessary to reach a 50% reduction in median SNAP amplitude in 8 out of 10 probable CTS patients and in 14 out of possible 20 CTS patients was below the lowest recorded value in the control group (25 min). It was shown that ischemia caused the block (reduction in median SNAP amplitude) by demonstrating (1) that the reversal of a 70% block with release of wrist flexion was prevented by inflating a pneumatic cuff around the upper arm to above systolic pressure for 5 minutes before release of wrist flexion after which (2) the SNAP amplitude returned to normal 30 seconds after deflating the cuff. Determination of T50 of the median nerve SNAP during wrist flexion has the potential to add to the sensitivity and specificity of the electrophysiological diagnosis of CTS.
- Harmon RL, Naylor AH. Sensory and mixed nerve action potential temporal dispersion in median neuropathy at the wrist. Am J Phys Med Rehabil 1999;78:213-215. Criteria Met (1/6: 6) Source: Medline Search. Abstract: Retrospective study to determine the usefulness of measuring SNAP and mixed nerve AP temporal dispersion to diagnose CTS demonstrated that increased median mixed nerve AP temporal dispersion may occur in association with peak latency prolongation in CTS. However, the small magnitude of the increase makes the clinical usefulness of this observation unclear.
- Healy C, Watson JD, Longstaff A, Campbell MJ. Magnetic resonance imaging of the carpal tunnel. J Hand Surg Br 1990;15:243-248. Criteria Met (3/6: 1,2,3) Source: Medline Search.
- Herrick RT, Herrick SK. Thermography in the detection of carpal tunnel syndrome and other compressive neuropathies. J Hand Surg Am 1987;12:943-949. Criteria Met (1/6: 1) Source: Medline Search.
- *Holmgren H, Rabow L. Internal neurolysis or ligament division only in carpal tunnel syndrome. II. A 3 year follow-up with an evaluation of various neurophysiological parameters for diagnosis. Acta Neurochir (Wien) 1987;87:44-47. Criteria Met (2/6: 1,2) Source: Medline Search.
- *Holmgren-Larsson H, Leszniewski W, Linden U, Rabow L, Thorling J. Internal neurolysis or ligament division only in carpal tunnel syndrome— results of a randomized study. Act Neurochir (Wien) 1985;74:118-121. Criteria Met (0/6) Source: Holmgren, 1987.
- *Homan MM, Franzblau A, Werner RA, Albers JW, Armstrong TJ, Bromberg MB. Agreement between symptom surveys, physical examination procedures and electrodiagnostic findings for the carpal tunnel syndrome. Scand J Work Environ Health 1999;25:115-124. Background Reference. Source: Medline Search. Abstract: The goal of this study was to evaluate the concordance between various clinical screening procedures for carpal tunnel syndrome. The subject population consisted of 824 workers from 6 facilities. The procedures evaluated included bilateral median sensory nerve conduction testing, physical examinations, and symptom surveys, including hand diagrams. The agreement between the outcomes of various combinations of these procedures was assessed by determining the kappa coefficient. There was relatively poor overlap between the reported symptoms, the physical examination findings, and the electrodiagnostic results consistent with carpal tunnel syndrome. Overall, only 23 out of 449 subjects (5%) with at least 1 positive finding met all 3 criteria (symptoms, physical examination findings, and electrophysiological results consistent with carpal tunnel syndrome) for the dominant hand. The screening procedures showed poor or no agreement with kappa values ranging between 0.00 and 0.18 for all the case definitions evaluated for carpal tunnel syndrome. The poor overlap between the various screening procedures warns against the use of electrodiagnostic findings alone without the symptom presentation being considered. The results of this study also point to a need for the further development and evaluation of methods for detecting carpal tunnel syndrome.
- Hughes ACR. An evaluation of 2 electrodiagnostic procedures in patients with symptoms of a carpal tunnel syndrome. Electroencephalogr Clin Neurophysiol 1977;43:140. Criteria Met (0/6) (abstract only) Source: AAEM Consultant 1993.
- *Imai T, Matsumoto H, Minami R. Asymptomatic ulnar neuropathy in carpal syndrome. Arch Phys Med Rehabil 1990;71:992-994. Criteria Met (3/6: 1,3,5) Source: Medline Search.
- Imaoka H, Yorifuji S, Takahashi M, Nakamura Y, Kitaguchi M, Tarui S. Improved inching method for the diagnosis and prognosis of carpal tunnel syndrome. Muscle Nerve 1992;15:318-324. Criteria Met (5/6: 2,3,4,5,6) Source: Medline Search. Abstract: A modified sensory “inching” method for the electrodiagnosis of CTS is described. The median nerve as stimulated at the cubital segment with 8 channel recording electrodes placed at 15 mm intervals along the median nerve from a point 3 cm proximal to the distal wrist crease up to the middle finder. Eight consecutive SNAP were recorded and the negative peak latency measured. Each latency (ms) was plotted against distance (mm). The results were a linear relationship (1) from channel 1 to 8 in 32 normal subjects and (2) from channel 1 to at least channel 4 in CTS patients. In 73 of 84 (87%) limbs of CTS patients, there was a conductive abnormality in the distal recordings as determined by discontinuous changes in the SNAP latency (greater than 0.6 ms) or amplitude (absence of response). The results suggest that this method provides high sensitivity and specificity for the diagnosis of CTS. A prospective study with comparison to current techniques would help determine whether or not the technique has advantages over current recommended techniques.
- Iyer V, Fenichel GM. Normal median nerve proximal latency in carpal tunnel syndrome: a clue to coexisting Martin-Gruber anastomosis. J Neurol Neurosurg Psychiatry 1976;39:449-452. Background Reference. Source: AAEM Consultant 1993.
- Jablecki CK, Andary MT, Di Benedetto M, Horowitz SH, Marino RJ, Rosenbaum RB, Shields RW, Stevens JC, Williams FH. American Association of Electrodiagnostic Medicine. Guidelines for outcome studies in electrodiagnostic medicine. Muscle Nerve 1996;19:16261635. Source: AAEM 2000 CTS Task Force member.
- Jablecki CK, Andary MT, So YT, Wilkins DE, Williams FH. Literature review of the usefulness of nerve conduction studies and electromyography for the evaluation of patients with carpal tunnel syndrome. Muscle Nerve 1993;16:1392-1444. Background Reference. Source: AAEM 2000 CTS Task Force member.
- Jackson D, Clifford JC. Electrodiagnosis of mild carpal tunnel syndrome. Arch Phys Med Rehabil 1989;70:199-204. Criteria Met (6/6: 1,2,3,4,5,6) Source: Medline Search. Abstract: This study evaluated the following techniques: (a) median nerve stimulation in the palm and recording proximal at the wrist (8 cm), (b) sensory latency difference between median and radial stimulation at the wrist and recording on the thumb (10 cm), (c) medial-ulnar sensory latency difference with stimulation at the wrist and recording on the ring finger (14 cm), (d) median-ulnar sensory latency difference with stimulation in the palm and recording at the wrist (8 cm), and (e) amplitude ratio between median SNAP to index finger/ulnar SNAP to the little finger. One hundred thirty-one abnormal hands in 123 subjects and 38 normal hands in 38 people were evaluated with analysis focused on the 40 hands in the mild CTS group. Symptoms were systematically recorded and reported in each patient. The median-radial latency difference to the thumb and median-ulnar latency difference to ring finger was slightly more sensitive than the midpalm studies. Amplitude ratios were very insensitive.
- Jhee WH, Oryshkevich RS, Wilcox R. Severe carpal tunnel syndrome with sparing of sensory fibers. Orthop Rev 1986;15:103-106. Criteria Met (0/6) Source: Medline Search.
- Johnson EW, Kukla RD, Wongsam PE, Piedmont A. Sensory latencies to the ring finger: normal values and relation to carpal tunnel syndrome. Arch Phys Med Rehabil 1981;62:206-208. Criteria Met (3/6: 1,3,5) Source: Redmond, 1988. Abstract: With stimulation at the wrist and recording over the ring finger, the median and ulnar nerve DSL were recorded across the wrist; 37 normal subjects and 18 cases of CTS were evaluated. The difference between median and ulnar DSL to the ring finger was abnormal in all 18 CTS patients.
- Johnson EW, Melvin JL. Sensory conduction studies of median and ulnar nerves. Arch Phys Med Rehabil 1967;48:25-30. Criteria Met (4/6: 1,3,5,6) Source: Dunnan, 1991. Abstract: With stimulation of the middle or index finger and recording over the median nerve at the wrist, orthodromic SNAPs and DSLs were determined in 120 controls. Orthodromic ulnar SNAPs and DSL were determined after stimulation of the ring finger or little finger and recording at the wrist and 44 controls. They report cases of abnormal DSL in patients with carpal tunnel syndrome, toxic neuropathy, early diabetic neuropathy, and other peripheral nerve involvement problems.
- Johnson EW, Sipski M, Lammertse T. Median and radial sensory latencies to digit I: normal values and usefulness in carpal tunnel syndrome. Arch Phys Med Rehabil 1987;68:140-141. Criteria Met (2/6: 1,3) Source: Medline Search.
- *Jordan SE, Greider JL Jr. Autonomic activity in the carpal tunnel syndrome. Orthop Rev 1987;16:165-169. Criteria Met (2/6: 1,2) Source: Medline Search.
- Joynt RL. Comparison of residual latency and palmar stimulation for diagnosis of carpal tunnel syndrome. Muscle Nerve 1984;7:565. Criteria Met (0/6) (abstract only) Source: Redmond, 1988.
- Joynt RL. Correlation studies of velocity, amplitude and duration in median nerves. Arch Phys Med Rehabil 1989;70:477-481. Criteria Met (4/6: 1,3,5,6) Source: Medline Search. Abstract: The following techniques were studied: (a) stimulation in the palm between the third and fourth metacarpals and median recording at the wrist and (b) stimulation at the wrist and CMAP recording over the ABP. Distal latencies, amplitudes, duration of response and residual latencies were evaluated; 390 patients were studied, all these were symptomatic and many of them had CTS. The results suggest that amplitude, duration, and conduction velocity are relatively poorly correlated and independent variables. There is a very high correlation between residual latency and distal motor latency, thus suggesting limited usefulness for residual latency in the diagnosis of CTS.
- Joynt RL. Differences in sensory conduction velocity between different sensory branches and segments of the median and ulnar nerves. Am J Phys Med Rehabil 1989;68:210-214. Criteria Met (3/6: 1,5,6) Source: Medline Search.
- Kabiraj MMU, Al Rajeh S, Al Tahan AR, Abduljabbar M, Al Bunyan M, Daif AK, Awada A. Carpal tunnel syndrome: a clinicoelectrophysiological study. Medical Science Research 1998;26:631633. Criteria Met (4/6: 2,3,4,5). Source: Medline Search. Retrospective review of 5 years record to identify 72 CTS patients 57% idiopathic, 19% associated with diabetes mellitus, 11% with rheumatoid arthritis, 7% with hypothyroidism, and 6% with renal or heart failure. The group of CTS patients showed abnormal median sensory and motor terminal latencies decreased median SNAP amplitude and velocity and median terminal latency index compared to a group of 65 normal subjects. There was a positive correlation between the median motor distal latency and the median terminal latency index. The study did not examine the percentage of CTS patients showing each type of NCS abnormality.
- Katims JJ, Rouvelas P, Sadler BT, Weseley SA. Current perception threshold: Reproducibility and comparison with nerve conduction in evaluation of carpal tunnel syndrome. Trans Am Soc Artif Intern Organs 1989;35:280-284. Criteria Met (2/6: 1,2) Source: Medline Search.
- Katz JN, Larson MG, Fossel AH, Liang MH. Validation of a surveillance case definition of carpal tunnel syndrome (comment in Am J Public Health 1991;81:161-162). Am J Public Health 1991;81:189-193. Criteria Met (2/6: 1,2) Source: Medline Search.
- Katz JN, Larson MG, Sabra A, Krarup C, Stirrat CR, Sethi R, Eaton HM, Fossel AH, Liang MH. The carpal tunnel syndrome: diagnostic utility of the history and physical examination findings (comments in Ann Intern Med 1990;113:254 and Ann Intern Med 1990;113:409). Ann Intern Med 1990;112:321-327. Criteria Met (2/6: 1,5) Source: Medline Search.
- Katz JN, Stirrat CR, Larson MG, Fossel AH, Eaton HM, Liang MH. A self-administered hand symptom diagram for the diagnosis and epidemiologic study of carpal tunnel syndrome. J Rheumatol 1990;17:1495-1498. Criteria Met (3/6: 2,3,4) Source: Medline Search.
- Katz JN, Stirrat CR. A self-administered hand diagram for the diagnosis of carpal tunnel syndrome. J Hand Surg Am 1990;15:360363. Criteria Met (1/6: 1) Source: Medline Search.
- Kemble F. Electrodiagnosis of the carpal tunnel syndrome. J Neurol Neurosurg Psychiatry 1968;31:23-27. Criteria Met (4/6: 1,2,5,6) Source: Winn, 1989. Abstract: With stimulation over thumb, index, middle, and ring fingers and recording over the median nerve at the wrist and elbow, orthodromic SNAPs and CMAPs to the APB were determined in 120 hands in 66 female patients with CTS. They found that the DSL was more likely to be abnormal than DML.
- Kiernan MC, Mogyoros I, Burke D. Conduction block in carpal tunnel syndrome. Brain 1999;122(Pt 5):933-941. Criteria Met (4/6: 1,4,5,6) Source: Medline Search. Abstract: Prolonged wrist extension was performed passively (written communication) in 6 healthy subjects and 7 CTS patients. Preliminary experiments demonstrated that changes in the CSAP (compound sensory action potential) developed sooner than changes in the CMAP so subsequent studies were confined to the CSAP. During maintained wrist extension to 90 degrees, all subjects developed greater than 50% conduction block in cutaneous afferents in the wrist (but not distal to the wrist) and slight increases in distal latency (0.44 ± 0.07 ms for normal subjects and 0.51 ± 0.05 ms for CTS patients). The changes in normal subjects began after wrist extension for 21.8 ± 5.8 min and was maximal at 49.3 ± 10.7 min. The changes in CTS patients began after wrist extension for 12.8 ± 2.8 min and was maximal at 28.1 ± 3.3 min. The reduction in the amplitude of the SNAP potential in normal subjects and CTS patients was associated with changes in axonal excitability at the wrist with a decrease in supernormality and an increase in refractoriness compatible with axonal depolarization. All subjects (normals and patients) reported mild paresthesiae during prolonged wrist extension and more intense paresthesiae were reported following the release of wrist extension. It is concluded that wrist extension produces a depolarization block in both normal subjects and CTS patients, much as occurs with ischemic compression, but that this block cannot be altered merely by compensating for the axonal depolarization. It is argued that conduction block and conduction slowing need not always be attributed to disturbed myelination, and that ischemic compression may be sufficient to explain some of the intermittent symptoms and electrodiagnostic findings in patients with carpal tunnel syndrome, particularly when it is of mild or moderate severity.
- Kim LYS. Palmar digital nerve stimulation to diagnose carpal tunnel syndrome. Orthop Rev 1983;59-63. Criteria Met (4/6: 1,3,5,6) Source: Joynt, 1989. Abstract: With stimulation in the midpalm and recording at the wrist, median and ulnar distal latencies and medianulnar distal latency differences were determined in 66 hands in 33 normal control subjects and 50 hands in 39 mild CTS patients. Mild CTS was defined as patients who had symptoms who were highly suggestive of CTS, but had normal DSL between the finger and wrist. Sixty percent of these mild CTS patients were abnormal by the median-ulnar difference criteria (greater than or equal to 0.4 ms).
- Kimura J. A method for determining median nerve conduction velocity across the carpal tunnel. J Neurol Sci 1978;38:1-10. Criteria Met (5/6: 1,2,3,5,6) Source: Palliyath, 1990. Abstract: With stimulation at the wrist and midpalm and recording SNAPs over the index finger and CMAPs from the APB, NCVs were determined across the carpal tunnel for both motor and sensory nerves; 50 hands from 25 control subjects and 20 hands from 13 patients with mild CTS were evaluated. The motor and sensory NCV across the carpal tunnel were more likely to be abnormal than conventional DSLs and DMLs determined from the wrist.
- Kimura J. Collision technique. Physiologic block of nerve impulses in studies of motor nerve conduction velocity. Neurology 1976;26:680682. Background Reference. Source: Kimura 1978.
- Kimura J. The carpal tunnel syndrome: Localization of conduction abnormalities within the distal segment of the median nerve. Brain 1979;102:619-635. Criteria Met (6/6: 1,2,3,4,5,6) Source: Shurr, 1986. Abstract: With stimulation at the wrist and palm, orthodromic SNAPs were recorded over the index finger and median CMAP from the wrist to APB were recorded from 122 hands from 61 normal subjects and 172 hands from 105 CTS patients. Sixty-one percent of the median CMAPs were abnormal, 63% of the wrist-to-finger latencies were abnormal and 81% of the wrist to palm latencies were abnormal. They also reported cases where l cm inching stimulation across the carpal tunnel was abnormal in patients with otherwise normal studies.
- Kimura I, Ayyar DR. The carpal tunnel syndrome: Electrophysiological aspects of 639 symptomatic extremities. Electromyogr Clin Neurophysiol 1985;25:151-164. Criteria Met (4/6: 1,2,3,5) Source: Mortier, 1988. Abstract: The following techniques were studied: (a) with stimulation at the elbow, wrist and mid-palm, orthodromic DSL were determined to the index finger, (b) DMLs were determined to the APB after stimulation at the wrist and elbow, and (c) electro-myography in 639 symptomatic hands from 438 CTS patients and 175 extremities of 148 normal subjects. There was a relative slowing of the sensory NCV across the carpal tunnel as compared to the forearm in 100% of the patients with CTS. This was more sensitive than the median DSL and DML. Forty percent of the patients had abnormalities on needle EMG with 21.7% having positive sharp waves or fibrillations.
- Kimura J, Murphy MJ, Varda DJ. Electrophysiological study of anomalous innervation of intrinsic hand muscles. Arch Neurol 1976;33:842-844. Background Reference. Source: Gutmann, 1986.
- *Kopell HP, Goodgold J. Clinical and electrodiagnostic features of carpal tunnel syndrome. Arch Phys Med Rehabil 1968;49:371-376. Criteria Met (2/6: 1,2) Source: Louis, 1987.
- Koskimies K, Farkkila M, Pyykko I, Jantti V, Aatola S, Starck J, Inaba R. Carpal tunnel syndrome in vibration disease. Br J Ind Med 1990;47:411-416. Criteria Met (2/6: 1,3) Source: Medline Search.
- Kothari MJ, Rutkove SB, Caress JB, Hinchey J, Logigian EL, Preston DC. Comparison of digital sensory studies in patients with carpal tunnel syndrome. Muscle Nerve 1995;18:1272-1276. Criteria Met (5/6: 1,3,4,5,6) Source: Medline Search. Abstract: Prospective study to evaluate the relative sensitivity of antidromic sensory studies of the four median innervated digits in 59 patients with CTS diagnosed on the basis of a combination of clinical and median NCS abnormalities. The conduction distance was 10 cm for D1 and 13 cm for D2-D4. The reference population of 30 was composed of healthy volunteers or patients with lower extremity radiculopathies. In the 26 CTS patients with a normal DML to APB, digit 1 was abnormal in 81%, digit 2 in 42%, digit 3 in 54%, and digit 4 in 38%. In the 33 CTS patients with a prolonged DML, digit 1 was abnormal in 94%, digit 2 in 88%, digit 3 in 91%, and digit 4 in 88%. We conclude that in CTS patients with a normal DML to the APB, digit 1 is the most sensitive in identifying focal slowing of sensory conduction across the wrist. However, in CTS patients with a prolonged DML, the sensitivity of sensory conduction is not significantly different among the four digits.
- *Kouyoumdjian JA, Morita Mda P. Comparison of nerve conduction techniques in 95 mild carpal tunnel syndrome hands. Arq Neuropsiquiatr 1999;57:195-197.Criteria Met (3/6: 1,3,4). Source: Medline Search. Abstract: Prospective study of 5 NCS techniques in patients suspected of CTS and selected for the study at least one of the 5 studies was abnormal: (1) wrist-index finger onset latency (WIF), abnormal ! 2.8 ms, 14 cm; (2) palm-wrist onset latency (PW), abnormal ! 1.8 ms, 8 cm; (3) comparison median/ulnar palm-wrist onset latency (CPW), abnormal ! 0.4 ms; (4) comparison of median/ulnar onset latency, wrist-ring finger (CMU), abnormal ! 0.5 ms, 14 cm; (5) comparison of median/radial onset latency, wristthumb (CMR), abnormal ! 0.4 ms, 10 cm. All 95 CTS hands selected have the WIF " 3.5 ms to identify “mild CTS.” We found the CMR (97.8%) technique the most sensitive for mild CTS electrodiagnosis and the only comparative method with all potentials recordable when compared to CPW (88.4%), PW (84.2%), CMU (72.6%) and WIF (68.4%).
- Kraft GH, Halvorson GA. Median nerve residual latency: Normal value and use in diagnosis of carpal tunnel syndrome. Arch Phys Med Rehabil 1983;64:221-226. Criteria Met (4/6: 1,3,5,6) Source: Bleecker, 1987. Abstract: With stimulation at the elbow and wrist and recording over the ABP, DMLs and forearm NCVs were determined in 100 normal subjects and 3 CTS patients. The residual latency (DML–distance between stimulation and recording electrodes in mm/forearm NCV in m/s). They present 3 cases where the residual latency was the only abnormality found.
- Kremer M, Gilliatt RW, Golding JSR, Wilson TG. Acroparaesthesiae in carpal tunnel syndrome. Lancet 1953;2:590-595. Background Reference. Source: Phalen 1966.
- Kuhlman KA, Hennessey WJ. Sensitivity and specificity of carpal tunnel syndrome signs. Am J Phys Med Rehabil 1997;76:451-457. Background Reference. Source: Medline Search. Abstract: The sensitivity and specificity of six CTS signs were determined by evaluating 143 subjects (228 hands) with symptoms of CTS. Immediately after performing the six physical examination tests, standard nerve conduction studies were performed on all 228 hands to determine the presence or absence of CTS. CTS was present in 142 hands and absent in 86 hands. The signs were not very sensitive (2369%), but were fairly specific (66-87%) for CTS. A square-shaped wrist and abductor pollicis brevis weakness were the most sensitive signs (69 and 66%, respectively), and are recommended as part of the examination of CTS. Median nerve hypesthesia and the Phalen sign both have fair sensitivity (51%) but good specificity (85 and 76%, respectively). The median nerve compression sign and the HoffmannTinel sign both have poor sensitivity (28 and 23%, respectively), and thus are less helpful in evaluating subjects with suspected CTS.
- Kuntzer T. Carpal tunnel syndrome in 100 patients: sensitivity, specificity of multi-neurophysiological procedures and estimation of axonal loss of motor, sensory and sympathetic median nerve fibers. J Neurol Sci 1994;127:221-229. Criteria Met (6/6: 1,2,3,4,5,6) Source: Medline Search. Abstract: Study of 70 control subjects and of the more symptomatic hands of 100 CTS patients diagnosed independently by clinical history and examination. Study specifically designed to meet all six AAEM criteria for evaluation of usefulness of NCS to diagnose CTS including continuous monitoring of hand temperature during the NCS. Reports the criteria for abnormalities, sensitivities and specificities of 19 sensory, motor and autonomic parameters. 9/19 parameters reached a specificity of 97%. At least 1/9 of the parameters was abnormal in 87% of the CTS patients. Abnormal median CMAP and SNAP amplitudes and abnormal median F-wave parameters were not as sensitive or specific to diagnose CTS as abnormal median sensory and motor carpal tunnel segment conduction velocities. Of median nerve conduction velocities in the carpal tunnel segments, the sensory studies were more frequently abnormal than the motor studies.
- Lambert EH. Diagnostic value of electrical stimulation of motor nerves. Electroencephalogr Clin Neurophysiol 1962;22(suppl):9-16. Background Reference. Source: Kimura 1985.
- Laroy V, Spaans F, Reulen J. Nerve conduction studies show no exclusive ulnar or median innervation of the ring finger. Clin Neurophysiol 1999;110:1492-1497. Criteria Met (2/6: 1,3) Source: Medline Search. Abstract: Combination of retrospective study of 1617 hands of 1000 patients and prospective study of 430 hands in 260 patients referred for electrodiagnostic evaluation of brachialgia (not defined in paper). No case of mononeural innervation of D4 by the median or ulnar nerve was encountered. In all cases in which D4 SNAPs were obtained with both median and ulnar stimulation, it could be demonstrated that the SNAPs were not due to co-stimulation by simultaneous recording of SNAPs from another median or ulnar innervated finger. The authors discuss the reasons why some previous clinical and experimental studies may have mistakenly concluded that mononeural innervation of D4 occurs as a physiological variation. Finally, comparison of SNAP parameters in 183 hands with increased median nerve distal latencies showed conduction to be more impaired in the fibers innervating D4 than in those supplying D3.
- Lauritzen M, Liguori R, Trojaborg W. Orthodromic sensory conduction along the ring finger in normal subjects and in patients with a carpal tunnel syndrome. Electroencephalogr Clin Neurophysiol 1991;81(1):18-23. Criteria Met (5/6: 1,3,4,5,6) Source: Medline Search. Abstract: With stimulation of the ring finger using ring electrodes and needle electrode recording with averaging at the wrist over the median and ulnar nerves, DSLs and median-ulnar differences were recorded in 23 normal volunteers and 38 CTS patients. Their findings suggest that the median-ulnar orthodromic DSL difference from the ring finger was a useful screening technique in the diagnosis of CTS, but did not identify every patient when compared to stimulation of thumb and/or middle finger.
- Lesser EA, Venkatesh S, Preston DC, Logigian EL. Stimulation distal to the lesion in patients with carpal tunnel syndrome. Muscle Nerve 1995;18:503-507. Criteria Met (5/6: 1,3,4,5,6) Source: Medline Search. Abstract: In CTS patients, a low amplitude median CMAP or SNAP with stimulation at the wrist crease (proximal to the carpal tunnel) is due to either demyelination or axonal degeneration or both. With axonal degeneration, the amplitude of the CMAP and SNAP is the same with stimulation above and below the site of the pathology. With focal demyelination, the amplitude of the CMAP and SNAP is greater with stimulation below compared to stimulation above the site of the pathology. Of 59 consecutive CTS patient hands, 36 (61%) showed significant reduction in CMAP and/or antidromic SNAP amplitudes with stimulation at the wrist compared to stimulation at the palm which indicated the presence of focal demyelination resulting in conduction block and/or pathologic dispersion with phase cancellation. We conclude that in patients with CTS, as in other entrapment neuropathies, stimulation both proximal and distal to the carpal tunnel provides important information about the median nerve pathology in the carpal tunnel.
- Lew HL, Wang L, Robinson LR. Test-retest reliability of combined sensory index: implications for diagnosing carpal tunnel syndrome. Muscle Nerve 2000;23: 1261-1264. Criteria Met (5/6: 1,2,3,5,6). Source: Medline Search. Abstract: Robinson and colleagues (1998) previously showed that, compared to a single NCS, the combined sensory index (CSI) has superior sensitivity and specificity for the diagnosis of CTS. This prospective study evaluated the test-retest reliability of a single NCS versus the CSI by the same examiner in one hand of 32 subjects: 26 normal subjects and 6 CTS patients. In a subgroup of 18 subjects, the study evaluated the effect of temperature on absolute latencies and latency differences derived from sensory NCS. CSI had the highest test re-test reliability and the CSI score (the sum of 3 latency differences) was less affected by temperature changes than absolute latency values of individual NCSs.
- Logigian EL, Busis NA, Berger AR, Bruynincky F, Khalil N, Shahani BT, Young RR, Lumbrical sparing in carpal tunnel syndrome: anatomic, physiologic, and diagnostic implications. Neurology 1987;37:1499-1505. Criteria Met (5/6: 1,3,4,5,6) Source: Medline Search. Abstract: With stimulation at the wrist, simultaneous recording of CMAP to the second lumbrical and APB were recorded in 61 patients with CTS (as defined by electrophysiologic criteria) and in 16 normal subjects. They found that the lumbrical distal latency was relatively spared when compared to the distal latency to the APB and that this may be a sensitive test that could be used in addition to other tests for the diagnosis of CTS. They also found that it was not specific for CTS since it occasionally was abnormal in more proximal lesions of the median nerve.
- Loong SC. The carpal tunnel syndrome: a clinical and electrophysiological study of 250 patients. Proc Aust Assoc Neurol 1977;14:51-62. Criteria Met (3/6: 1,2,6) Source: Holmgren, 1987.
- Loong SC, Seah CS. Comparison of median and ulnar sensory nerve action potentials in the diagnosis of the carpal tunnel syndrome. J Neurol Neurosurg Psychiatry 1971;34:750-754. Criteria Met (5/6: 1,2,3,5,6) Source: Macleod, 1987. Abstract: With stimulation at the index and little fingers and recording at the wrist over the median and ulnar nerves, DSL and SNAP amplitudes were recorded in 30 healthy female subjects and 22 hands in 15 CTS patients. They found that the median-to-ulnar SNAP amplitude ratio of less than 1 was a sensitive test in the diagnosis of CTS and particularly useful in patients who showed a normal DML and DSL.
- *Louis DS, Hankin FM. Symptomatic relief following carpal tunnel decompression with normal electroneuromyographic studies (notification of retraction by Hankin and Louis in two subsequent issues: Orthopedics 1988;11:532 and Orthopedics 1988;11:1244). Orthopedics 1987;10:434-436. Criteria Met (1/6: 2) Source: Medline Search.
- *Luchetti R, Schoenhuber R, Landi A. Localized nerve damage recorded intraoperatively in carpal tunnel syndrome. Electromyogr Clin Neurophysiol 1988;28:379-383. Criteria Met (3/6: 1,3,5) Source: Medline Search.
- *Luchetti R, Schoenhuber R, Nathan P. Correlation of segmental carpal tunnel pressures with changes in hand and wrist positions in patients with carpal tunnel syndrome and controls. J Hand Surg [Br ] 1998;23:598-602. Criteria Met (3/6: 1,2,5) Source: Medline Search. Abstract: The authors investigated pressures with an endoscopic pressure monitor at 1 cm intervals along the carpal tunnel in 39 patients with CTS and 12 controls. Pressures were measured for relaxed and gripping hand positions in combination with neutral, extended, and flexed wrist positions. The study confirmed previous reports that CT pressures are generally higher in CTS patients than controls, and that intratunnel pressures are generally increased with wrist extension in comparison with wrist flexion. Maximum intratunnel pressures were generally found in the central part of the tunnel and minimum pressures in the distal tunnel. Gripping hand pressures in the tunnel were lowest with the wrist flexed. In both controls and CTS patients, only in the neutral wrist and relaxed hand positions were pressures highest at the point where nerve conduction studies have indicated the nerve is most likely to be compromised (in the midpalm just distal to the distal margin of the carpal tunnel).
- Lundborg G, Gelberman RH, Minteer-Convery M, Lee YF, Hargens AR. Median nerve compression in the carpal tunnel functional response to experimentally induced controlled pressure. J Hand Surg 1982;7:252-259. Background Reference. Source: AAEM 2000 CTS Task Force member.
- Lundborg G, Lie-Stenstrom AK, Sollerman C, Stromberg T, Pyykko I. Digital vibrogram: a new diagnostic tool for sensory testing in compression neuropathy. J Hand Surg Am 1986;11:693-699. Criteria Met (3/6: 1,2,3) Source: Medline Search.
- *Macdonald G, Robertson MM, Erickson JA. Carpal tunnel syndrome among California dental hygienists. Dent Hyg (Chic) 1988;62:322327. Criteria Met (2/6: 1,2) Source: Medline Search.
- *Macdonell RA, Schwartz MS, Swash M. Carpal tunnel syndrome: Which finger should be tested? An analysis of sensory conduction in digital branches of the median nerve. Muscle Nerve 1990;13:601-606. Criteria Met (3/6: 1,2,3) Source: Medline Search.
- *MacLean IC, Sik Cho D. Carpal tunnel syndrome: a comparison of distal sensory latencies of median and radial nerves. Muscle Nerve 1981;4:444. Criteria Met (0/6) (Abstract Only) Source: Rivner, 1991.
- Macleod WN: Repeater F-waves: a comparison of sensitivity with sensory antidromic wrist-to-palm latency and distal motor latency in the diagnosis of carpal tunnel syndrome. Neurology 1987;37:773-778. Criteria Met (4/6: 1,3,5,6) Source: Medline Search. Abstract: With stimulation at the wrist and recording of F waves over the APB, the frequency of repeater F waves (identical recurring F waves in latency, configuration, and amplitude) was determined by measuring 100 supramaximal shocks; 209 healthy hands and 147 entrapped median nerves were evaluated. The repeater F waves was compared to the sensory 1 cm DSL inching latency across the wrist. A high percent repeater F-wave value was considered indicative of CTS and the sensitivity approaches that of the sensory antidromic inching technique across the carpal tunnel.
- Marin EL, Vernick S, Friedmann LW. Carpal tunnel syndrome: Median nerve stress test. Arch Phys Med Rehabil 1983;64:206-208. Criteria Met (5/6: 1,2,3,5,6) Source: Borg, 1986. Abstract: With median stimulation at the wrist and recording over the APB and ring electrodes to the index finger, DML and DSL were obtained from the median nerve in the neutral position, then in extreme tolerable extension at 5 minutes and 10 minutes followed by the testing in the extreme tolerable flexion position after 5 and 10 minutes. An orthosis was devised to enable the wrist to be held in extreme tolerable extension which ranged from 45E-85E and extreme tolerable flexion which ranged from 45E-90E. Fourteen hands in 14 patients who had CTS and 12 hands from 12 volunteers were evaluated. Of the 14 patients, 5 of these had normal DSL and DML latencies in the neutral position. Three of these 5 showed an increase in DSL from the upper range of normal to above normal following extension or flexion.
- Marinacci AA. Comparative value of measurement of conduction velocity and electromyography in the diagnosis of carpal tunnel syndrome. Arch Phys Med Rehabil 1964;45:548-554. Criteria Met (4/6: 1,2,3,5) Source: Nathan, 1988. Abstract: With stimulation at the wrist, elbow and axilla, and recording over the APB, motor NCVs and DMLs were determined in 204 patients having CTS and 64 control subjects. Needle EMG was also performed in this group; 70% of CTS cases had abnormal wrist DML and the needle EMG was abnormal in 96% of the cases (fibrillations, polyphasic units, and large amplitude motor units). Sensory latencies were also recorded in 23 CTS patients.
- Marsh DR. Use of a wheel esthesiometer for testing sensibility in the hand. J Hand Surg Br 1986;11:182-186. Criteria Met (3/6: 1,2,3) Source: Medline Search.
- Mavor H, Shiozawa R. Antidromic digital and palmar nerve action potentials. Electroencephalogr Clin Neurophysiol 1971;30:210-221. Criteria Met (4/6: 1,3,5,6) Source: Buchthal, 1974. Abstract: With stimulation at the elbow and wrist and recording over the middle finger, SNAPs and DSLs from the median nerve were recorded in 21 normal subjects. With stimulation over the ulnar nerve at the elbow and wrist, antidromic SNAPs and DSLs were recorded in 13 normal subjects. No CTS patients were studied.
- Mayer RF. Nerve conduction studies in man. Neurology 1962;12:733744. Criteria Met (4/6: 1,3,5,6) Source: Kraft, 1983. Abstract: The following techniques were studied in 64 normal subjects and 31 diabetics without peripheral neuropathy: (a) stimulation in axilla, above elbow and wrist with recording of the CMAP over the APB. Surface and concentric needle electrodes were used, (b) with stimulation in the axilla, above the elbow and wrist, SNAPs were recorded from digital nerves using surface and needle electrodes, (c) ulnar, (d) peroneal, (e) tibial, and (f) H reflex. They found a slight decrease in NCV in patients older than 50, and in patients with diabetes mellitus without clinical signs of peripheral neuropathy. No CTS patients were studied.
- *Mazur A. Role of thenar electromyography in the evaluation of carpal tunnel syndrome. Phys Med Rehabil Clin N Am 1998;9:755764. Review article. Background Reference. Source: Medline Search. Abstract: The author suggests that needle EMG of the APB (1) is not necessary to evaluate most cases of CTS and (2) be reserved for atypical situations or unusual presentations of CTS such as when (a) NCS cannot be performed or (b) when the median nerve pathology is potentially aggressive causing significant axonal injury over a short time.
- McLellan DL, Swash M. Longitudinal sliding of the median nerve during movements of the upper limb. J Neurol Neurosurg Psychiat. 1976;39:566-570. Background Reference. Source: AAEM CTS Task Force 2000 member. Normal subjects. An incidental finding during recording of median NAP with monopolar needle electrode in the median nerve in the upper arm was that the nerve slid longitudinally several mm when the limb moved at a joint. Wrist extension and flexion resulted in opposite directions of sliding movement. Note: the needle in nerve may have impeded movement leading to underestimates of magnitude of sliding.
- McNeil BJ, Keller E, Adelstein SJ. Primer on certain elements of medical decision making. NEJM 1975;293:211-215. Background Reference. Source: Gunnarsson 1997 paper.
- Melvin JL, Harris DH, Johnson EW. Sensory and motor conduction velocities in the ulnar and median nerves. Arch Phys Med Rehabil 1966;47:511-519. Criteria Met (4/6: 1,3,5,6) Source: Joynt, 1989. Abstract: The following techniques were studied: (a) orthodromic SNAPs were recorded from the median nerve at the wrist and elbow, (b) orthodromic SNAPs were recorded from the ulnar nerve after stimulation of the ring and little fingers and recording over the wrist and elbow, (c) antidromic SNAPs were recorded from the median and ulnar nerve after reversing the electrodes for the orthodromic SNAPs, (d) median CMAPs recording over the opponens pollicus, and (e) ulnar CMAP over the abductor digiti quinti. The orthodromic NCVs were determined in 48 normal persons, motor conduction NCVs were determined in 47 normal people and antidromic SNAPs were completed in 36 normal people. No CTS patients were studied. They found there was no significant difference between orthodromic and antidromic sensory NCVs and that the fastest afferent sensory NCVs were faster than the fastest efferent motor fibers.
- Melvin JL, Schuchmann JA, Lanese RR. Diagnostic specificity of motor and sensory nerve conduction variables in the carpal tunnel syndrome. Arch Phys Med Rehabil 1973;54:69-74. Criteria Met (5/6: 1,2,3,5,6) Source: Redmond, 1988. Abstract: With stimulation at the wrist and recording CMAP over the APB and SNAP over the index and middle finger, latency, velocities, and amplitudes were determined from 24 normal volunteers and 19 patients with CTS. They found that the DSL followed by the DML were the best tests and that sensory duration, sensory amplitude, motor amplitude, and motor duration were not sensitive.
- Merchut MP, Kelly MA, Toleikis SC. Quantitative sensory thresholds in carpal tunnel syndrome. Electromyogr Clin Neurophysiol 1990;30:119-124. Criteria Met (5/6: 1,2,3,4,6) Source: Medline Search. Abstract: Twenty-eight hands from 23 patients with CTS as defined by 1 or more of these abnormal NCSs; orthodromic DSL median-ulnar difference from ring finger-to-wrist, palm-to-wrist median DSL, finger-to-wrist median DSL, or DML from the wrist-toAPB. Quantitative sensory threshold (QST) testing was done using vibration thresholds and thermal sensitivity thresholds comparing the index to little finger in 23 age matched control subjects. Abnormal QST was found in only 3 of the 28 symptomatic hands (11%) and was found to be much less sensitive than NCSs.
- Merhar GL, Clark RA, Schneier HJ, Stern PJ. High-resolution computed tomography of the wrist in patients with carpal tunnel syndrome. Skeletal Radiol 1986;15:549-552. Criteria Met (3/6: 1,3,6) Source: Medline Search.
- Meyers S, Cros D, Sherry B, Vermeire P. Liquid crystal thermography: quantitative studies of abnormalities in carpal tunnel syndrome (comments in Neurology 1990;40:1146). Neurology 1989;39:1465-1469. Criteria Met (2/6: 1,2) Source: Medline Search.
- Mills KR. Orthodromic sensory action potentials from palmar stimulation in the diagnosis of carpal tunnel syndrome. J Neurol Neurosurg Psychiatry 1985;48:250-255. Criteria Met (4/6: 1,3,5,6) Source: Golding, 1986. Abstract: While recording at the wrist over the median and ulnar nerves, SNAPs were elicited by stimulation over the index and little fingers and from stimulation in the palm (mixed nerve); 72 hands with CTS, 53 healthy hands and 20 hands of patients with unrelated neurological conditions were evaluated. They found that the palm-to-wrist conduction velocity and the palm-to-wrist median-ulnar comparison was more likely to be abnormal than the DSL or DML. They also found no significant difference between the normal control group and the 20 hands with unrelated neurologic conditions.
- Molitor PJ. A diagnostic test for carpal tunnel syndrome using ultrasound. J Hand Surg Br 1988;1340-1341. Criteria Met (3/6: 1,3,5) Source: Medline Search.
- Monga TN, Laidlow DM. Carpal tunnel syndrome measurement of sensory potentials using ring and index fingers. Am J Phys Med 1982;61:123-129. Criteria Met (4/6: 1,2,3,5) Source: Redmond, 1988. Abstract: With stimulation of the fourth digit (D4), orthodromic SNAPs were simultaneously recorded at the wrist over the median and ulnar nerves in 15 control subjects and 30 CTS patients and the results compared to median sensory studies with stimulation of the second digit (D2). The D4 SNAP was absent or the peak latency prolonged more frequently than the D2 SNAP in patients with CTS.
- Monga TN, Shanks GL, Poole BJ. Sensory palmar stimulation in diagnosis of carpal tunnel syndrome. Arch Phys Med Rehabil 1985;66:598-600. Criteria Met (5/6: 1,2,3,5,6) Source: Jackson, 1989. Abstract: The following techniques were studied: (a) ring stimulation over the index and little fingers and recording at the wrist over the median and ulnar nerve, (b) median palm stimulation and recording at the wrist, and (c) wrist stimulation over median and ulnar nerves and recording over the APB and ADM were evaluated in 36 hands in 22 CTS patients and 22 normal patients. They found the palm-to-wrist stimulation to be abnormal in 88%, the median index finger DSL (in 86%), median-ulnar finger DSL comparison (in 81%), and median DML (in 81%).
- *Mortier G, Deckers K, Dijs H, Vander Auwera JC. Comparison of the distal motor latency of the ulnar nerve in carpal tunnel syndrome with a control group. Electromyogr Clin Neurophysiol 1988;28:7577. Criteria Met (3/6: 1,3,5) Source: Medline Search.
- Murga L, Moreno JM, Menendez C, Castilla JM. The carpal tunnel syndrome. Relationship between median distal motor latency and graded results of needle electromyography. Electromyogr Clin Neurophysiol 1994; 34: 377-383. Criteria Met (1/6: 2) Source: Medline Search.
- Nakamichi K, Tachibana S. Restricted motion of the median nerve in carpal tunnel syndrome. J Hand Surg 1995;20B:460-464. Background Reference. Source: AAEM 2000 CTS Task Force member. Ultrasound imaging of the mid carpal tunnel permits measurement of the magnitude of median nerve sliding with finger flexion. The studies demonstrated control subjects median nerves slid 1.75 ± 0.49 mm with finger flexion whereas CTS patients median nerves slid 0.37 ± 0.49 mm. The findings were compatible with limited longitudinal sliding on the median nerve in the CT of CTS patients.
- *Narkas AD. The role of thoracic outlet syndrome in the double crush syndrome. Am Hand Surg 1990;9:331-340. Criteria Met (1/6: 2) Source: Medline Search.
- *Nathan PA, Keniston RC, Meadows KD, Lockwood RS. Predictive value of nerve conduction measurements at the carpal tunnel. Muscle Nerve 1993;16:1377-1382. Criteria Met (3/6: 3,5,6) Source: Medline Search. Abstract: We compared the predictive values of three measurements of sensory conduction of the median nerve at the carpal tunnel (maximum latency difference [MLD], 8 cm latency [S8], and 14 cm latency [S14]) in 2334 hands of industrial workers, workers’ compensation patients, and students. The MLD for the median sensory nerve across the wrist was determined by the centimetric technique (inching study). The threshold, sensitivity, and specificity of abnormalities were as follows: MLD ! 0.40 ms, 86%, 82%, S8 ! 2.3 ms, 67%, 90% and S14 ! 3.6 ms, 56%, 94%.
- Nathan PA, Meadows KD, Doyle LS. Relationship of age and sex to sensory conduction of the median nerve at the carpal tunnel and association of slowed conduction with symptoms. Muscle Nerve 1988;11:1149-1153. Criteria Met (3/6: 1,2,4) Source: Medline Search.
- Nathan PA, Meadows KD, Doyle LS. Sensory segmental latency values of the median nerve for a population of normal individuals. Arch Phys Med Rehabil 1988;69:499-501. Criteria Met (6/6: 1,2,3,4,5,6) Source: Medline Search. Abstract: With stimulation at l cm intervals at the wrist and across the carpal tunnel and recording over the middle finger, 70 normal hands and 54 CTS hands were evaluated for relative sensitivity and specificity at 2 levels of abnormality. At 0.5 ms abnormality, the specificity was 97% and sensitivity was 54%. At 0.4 ms or greater, the sensitivity improved to 81% and specificity dropped to 81%. The positive predictive value at 0.5 ms was 93% and decreased to 77% at the 0.4 ms abnormality.
- Nathan PA, Srinivasan H, Doyle LS, Meadows KD. Location of impaired sensory conduction of the median nerve in carpal tunnel syndrome. J Hand Surg Br 1990;15:89-92. Criteria Met (6/6: 1,2,3,4,5,6) Source: Medline Search. Abstract: Stimulation in 1 cm segments across the carpal tunnel was performed from 2 cm proximal to the distal wrist crease (DWC) to 6 cm distal and SNAP latencies were recorded over the middle finger in 70 normal and 217 CTS hands. The focal areas of slowing were reported with the most common area of slowing 3 to 4 cm distal to the DWC with slowing proximal to the DWC being unusual.
- *Nau HE, Lange B, Lange S. Prediction of outcome of decompression for carpal tunnel syndrome. J Hand Surg Br 1988;13:391-394. Criteria Met (1/6: 3) Source: Medline Search.
- Nesathurai S, Gwardjan A, Kamath AN. Median-to-ulnar sensory nerve action potential amplitude ratio as an electrodiagnostic adjunct for carpal tunnel syndrome. Arch Phys Med Rehabil 1999;80:756759. Criteria Met (normal population study 3/6: 3,4,6). Source: Medline Search. Abstract: Retrospective review of previously obtained NCS data in 46 normal controls to obtain normative data for the median-to-ulnar sensory nerve action potential (SNAP) amplitude ratio (MUSAR) and to discuss the potential use of MUSAR in diagnosis of CTS. Antidromic median and ulnar SNAPs were recorded and the respective MUSAR ratios were calculated. Descriptive statistical analysis was completed with the assumption that SNAP values are not Gaussian in distribution. The normal MUSAR ranged from .74 (5th percentile) to 2.5 (95th percentile). The MUSAR, being an intrapersonal ratio, may decrease the false positives and false negatives that would otherwise arise when using absolute values of SNAP amplitudes. Further studies are needed to determine the clinical and application of the MUSAR value to the diagnosis of CTS.
- Nielsen VK. Sensory and motor nerve conduction in the median nerve in normal subjects. Acta Med Scand 1973;194:435-443. Criteria Met (normal population study 5/6: 1,3,4,5,6) Source: Buchthal, 1974. Abstract: Orthodromic SNAPs were recorded over the median nerve using needle electrodes at the wrist and elbow after stimulation of the thumb and middle fingers. CMAPs were recorded with concentric needle electrodes placed in the endplate zone of the APB after stimulation at the wrist and elbow. NCVs were determined for 28 male and 20 female normal subjects aged 16 to 62 years. There was no significant difference in NCV between male and female subjects. There was a decrease in NCV with increasing age. No CTS patients were studied.
- Occupational Disease Surveillance. Carpal tunnel syndrome. MMWR Morb Mortal Wkly Rep 1989;38:485-489. Background Reference Source: Baker, 1990.
- *Osborn JB, Newell KJ, Rudney JD, Stoltenberg JL. Carpal tunnel syndrome among Minnesota dental hygienists. J Dent Hyg 1990;64(2):79-85. Criteria Met (2/6: 1,2) Source: Medline Search.
- Padua L, Lo Monaco M, Valente EM, Tonali PA. A useful electrophysiologic parameter for diagnosis of carpal tunnel syndrome. Muscle Nerve 1996;19:48-53. Criteria Met (6/6: 1,2,3,4,5,6). Source: Medline Search. Abstract: In 43 patients (50 hands) with clinical manifestations of mild-moderate CTS and 36 healthy volunteers (40 hands), orthodromic sensory nerve conduction velocity (SNCV) was measured with surface electrodes in the median nerve between the third digit and palm and between the palm and wrist. These figures were used to calculate the ratio of distal to proximal conduction (distoproximal ratio). All 90 hands were also subjected to other nerve conduction studies used for diagnosis of CTS. All control hands presented distoproximal ratios less than 1.0 reflecting higher conduction rates in the proximal segment. In contrast, 49 of 50 CTS hands (98%) presented reversed ratios (>1.0) indicating compromised proximal conduction. The sensitivity of this test was significantly greater than that of other methods evaluated, including comparative studies and segmental study of the palm-wrist portion of the median nerve. Segmental study of median SNCV with calculation of the distoproximal ratio is a sensitive technique for diagnosis of CTS in patients with normal findings in standard nerve conduction studies. Note: The author indicated by correspondence that the mean ± SD for the Control DML in Table 1 should read 3.2 ± 0.4 and not 3.2 ± 0.8 as published.
- Padua L, LoMonaco M, Gregori B, Valente EM, Padua R, Tonali P. Neurophysiological classification and sensitivity in 500 carpal tunnel syndrome hands. Acta Neurol Scand 1997;96:211-217. Criteria Med (6/6: 1,2,3,4,5,6) Source: Medline Search. Abstract: Prospective study of 500 hands (379 patients) with clinical diagnosis of CTS symptoms. Normal values from the same laboratory previously published (Padua, 1996). In the 500 CTS patients, DML was prolonged (55%), median orthodromic sensory latency was prolonged (D2, 74%; D3, 67%). Of the remaining 117 patients with normal DML and median orthodromic sensory studies over 14 cm, the median sensory palmwrist NCV over 8 cm was abnormal in 21% and the distoproximo ratio of the median palm and digit segments was abnormal in 87%.
- Palliyath SK, Holden L. Refractory studies in early detection of carpal tunnel syndrome. Electromyogr Clin Neurophysiol 1990;30:307-309. Criteria Met (5/6: 1,3,4,5,6) Source: Medline Search. Abstract: Using paired stimuli and varying the inter-stimulus interval, the absolute refractory period (ARP) and relative refractory period (RRP), were determined in 10 patients with mild electrophysiologic changes suggestive of CTS. They found that the sensory RRP was sensitive in diagnosing early CTS.
- *Pavesi G, Olivieri MF, Misk A, Mancia D. Clinicalelectrophysiological correlations in the carpal tunnel syndrome. Ital J Neurol Sci 1986;7:93-96. Criteria Met (3/6: 2,3,5) Source: Medline Search.
- Pease WS, Cannell CD, Johnson EW. Median to radial latency difference test in mild carpal tunnel syndrome. Muscle Nerve 1989;12:905-909. Criteria Met (4/6: 1,3,5,6) Source: Medline Search. Abstract: The following techniques were studied: (a) antidromic DSL median radial differences to the thumb, (b) antidromic DSL after stimulation at the wrist and recording from the third digit, (c) median mid-palmar DSL compared as a ratio of the wrist to middle finger DSL, (d) median ulnar DSL latency difference between the ulnar SNAP recorded from the little finger after stimulation at the wrist and the median DSL after stimulation at the wrist and recording from the middle finger, and (e) median motor DML after recording from the APB after stimulation at the wrist. Three hundred thirty-three symptomatic hands in 262 patients were initially evaluated with subgroups of patients with CTS evaluated with different tests. The median radial DSL difference and median ulnar DSL difference were most likely to be abnormal followed by median DSL then the palmto-wrist DSL latency ratio and lastly the DML.
- Pease WS, Cunningham ML, Walsh WE, Johnson EW. Determining neurapraxia in carpal tunnel syndrome. Am J Phys Med Rehabil 1988;67:117-119. Criteria Met (5/6: 1,3,4,5,6) Source: Medline Search. Abstract: With needle stimulation at the wrist and midpalm, CMAPs were recorded over the APB in 25 CTS patients and 23 healthy asymptomatic persons. They found a significant difference in the amplitude of the CMAP in the CTS group when compared to the control group. They propose that this is evidence for conduction block (neurapraxia) in CTS.
- Pease WS, Lee HH, Johnson EW. Forearm median nerve conduction velocity in carpal tunnel syndrome. Electromyogr Clin Neurophysiol 1990;30:299-302. Criteria Met (4/6: 1,3,4,5) Source: Medline Search. Abstract: The NCV of the median nerve in the forearm was determined by 2 methods: (a) stimulation in the forearm and recording the nerve action potential at the wrist, and (b) stimulation at the wrist and elbow with recording over the APB, in 21 CTS patients and 16 control subjects. They found that the forearm NCV was slowed in the CTS group using either technique. The authors have proposed that this suggest that there is proximal nerve dysfunction as a result of median nerve compression in the carpal tunnel.
- *Peterson GW, Will AD. Newer electrodiagnostic techniques in peripheral nerve injuries. Orthop Clin North Am 1988;19:13-25. Criteria Met (0/6) Source: Narkis, 1990.
- *Phalen GS. The carpal tunnel syndrome: clinical evaluation of 598 hands. Clin Orthop 1972;83:29-40. Background Reference. Source: Katz 1990 (J Rheumatology).
- *Phalen GS. The carpal tunnel syndrome: seventeen years’ experience in diagnosis and treatment of 654 hands. J Bone Joint Surg 1966;48:211-228. Criteria Met (1/6: 2) Source: Meyers, 1989.
- Phalen GS, Gardner WJ, LaLonde AA. Neuropathy of the median nerve due to compression beneath the transverse carpal ligament. J Bone Joint Surg 1950;32-A:109-112. Background Reference. Source: Braun, 1989.
- Plaja J. Comparative value of different electrodiagnostic methods in carpal tunnel syndrome. Scan J Rehabil Med 1971;3:101-108. Criteria Met (4/6: 1,3,5,6) Source: Joynt, 1989. Abstract: The following techniques were studied: (a) CMAP potentials were recorded after stimulation at the wrist and recording with coaxial needle electrodes, (b) orthodromic SNAPs with stimulation over the index finger and recording with surface electrodes at the wrist, (c) needle EMG using a coaxial needle, (d) strength/duration curves and chronaxy. Fifty-six cases of CTS and 20 normal subjects were evaluated. Sensory latencies were more likely to be abnormal than the other techniques measured.
- Preston DC, Logigian EL. Lumbrical and interossei recording in carpal tunnel syndrome [see comments]. Muscle Nerve 1992; 15: 1253-1257. Criteria Met (5/6: 1,3,4,5,6) Source: Medline Search. Abstract: Median motor studies are commonly “normal” in mild carpal tunnel syndrome (CTS). This reflects either the sparing of motor compared to sensory fibers, or the inability of conventional studies to detect an abnormality. A novel approach to demonstrate early motor fiber involvement in CTS is the placement of the same active electrode lateral to the third metacarpal, allowing recording from the second lumbrical or the deeper interossei, when stimulating the median or ulnar nerves at the wrist, respectively. We compared the difference between these latencies in 51 normal control hands to 107 consecutive patient hands referred with symptoms and signs suggestive of CTS, who were subsequently proven to have electrophysiologic CTS by standard nerve conduction criteria. A prolonged lumbrical-interossei latency difference (>0.4 ms) was found to be a sensitive indicator of CTS in all patient groups. It was also helpful in patients with coexistent polyneuropathy, where localization of median nerve pathology at the wrist was otherwise difficult.
- *Preston DC, Ross MH, Kothari MJ, Plotkin GM, Venkatesh S, Logigian EL. The median-ulnar latency difference studies are comparable in mild carpal tunnel syndrome. Muscle Nerve 1994; 17: 1469-1471. Criteria Met (2/6: 1,3). Source: Medline Search. Abstract: Compares sensitivity 159 patients of orthodromic palm-wrist mixed palmar median-ulnar peak latency difference with normal <0.4 ms, antidromic wrist-D4 sensory median-ulnar onset latency difference with normal <0.5 ms, and the second lumbrical/interossei motor with normal <0.5 ms. See discussion of benefits of techniques and diagrams of electrode placements and line drawings of electrode and stimulator placement.
- Preswick G. The effect of stimulus intensity in motor latency in carpal tunnel syndrome. J Neurol Neurosurg Psychiatry 1963;26:398-401. Criteria Met (4/6: 1,3,5,6) Source: Loong, 1971. Abstract: With stimulation at the wrist and coaxial needle electrode recording from the APB, DMLs were recorded at super-maximal stimulation and threshold stimulation in 29 CTS hands from 25 patients and 25 control subjects. Over 80% of the patients were identified with an abnormality either with super-maximal stimulation or threshold stimulation. Threshold stimulation was more sensitive than supermaximal stimulation.
- Read RL. Stress testing in nerve compression. Hand Clin 1991;7:521526. Criteria Met (1/6: 3). Source: Medline Search. Comment: Inspection of the tracings in the article indicates that the nonphysician author changed the sweep speed and gain during the recordings which casts doubt on the accuracy of the conclusions and confounds the reproducibility of the measurements.
- Redmond MD, Rivner MH. False positive electrodiagnostic tests in carpal tunnel syndrome. Muscle Nerve 1988;11:511-518. Criteria Met (4/6: 1,3,5,6) Source: Medline Search. Abstract: Several techniques were evaluated in a normal population using literature norms to assess for specificity in 100 hands of 50 normal subjects. Fifteen percent of the hands (30% of people) exhibited an abnormal median-to-ulnar sensory amplitude ratio, 8% of hands (14% of people) had abnormal residual latencies, and 4% of hands (8% of people) had prolonged median-ulnar palm to wrist latency (8 cm) differences. They suggested a more conservative abnormality of >0.5 ms between median and ulnar nerve for midpalm stimulation to avoid false positive tests for CTS. No CTS patients were studied. Rempel D, Evanoff B, Amadio PC, de Krom M, Franklin G, Franzblau A, Gray R, Gerr F, Hagberg M, Hales T, Katz JN, Pransky G. Consensus criteria for the classification of carpal tunnel syndrome in epidemiologic studies. Am J Public Health 1998;88:1447-1451. Source: Medline Search. Background Reference. Abstract: Criteria for the classification of carpal tunnel syndrome for use in epidemiologic studies were developed by means of a consensus process. Twelve medical researchers with experience in conducting epidemiologic studies of carpal tunnel syndrome participated in the process. The group reached agreement on several conceptual issues. First, while there is no perfect gold standard for carpal tunnel syndrome, the combination of electrodiagnostic study findings and symptom characteristics will provide the most accurate information for diagnosis of carpal tunnel syndrome. Second, use of only electrodiagnostic study findings to diagnose CTS is not recommended. Finally, specific combinations of symptom characteristics and physical examination findings may be useful to diagnose CTS but are likely to result in greater misclassification of patients than the combination of finding on the clinical history and the results of electrodiagnostic studies.
- Repaci M, Torrieri F, Di Blasio F, Uncini A. Exclusive electrophysiological motor involvement in carpal tunnel syndrome. Clin Neurophysiol 1999; 110: 1471-1474. Criteria Met (2/6: 3,5) Source: Medline Search.
- Resende LA, Adamo AS, Bononi APO, Castro HA, Kimaid PA, Fortinguerra CH, Schelp AO. Test of a new technique for the diagnosis of carpal tunnel syndrome. J Electromyog Kinesiol 2000;10:127-133. Criteria Met (4/6: 1,3,5,6) Source: Medline Search. Abstract: Study of 55 CTS hands (32 patients) compared to 40 normal hands (20 normal subjects) of the difference between the median motor distal latency to the second lumbrical muscle and the ulnar motor distal latency to the interossei muscle. The test was more sensitive to identify CTS than measurement of the median motor distal latency to the APB.
- Resende LA, Alves RP, Castro HA, Kimaid PA, Fortinguerra CR, Schelp AO. Silent period in carpal tunnel syndrome. Electromyogr and Clin Neurophys 2000;40:31-36. Criteria Met (4/6: 1,3,5,6) Source: Medline Search. Abstract: There was no correlation between the silent period alterations and the severity of the CTS in 20 hands of 20 CTS patients compared to 20 normal subjects.
- *Rivner MH. Carpal tunnel syndrome: a critique of “newer” nerve conduction techniques. In: AAEM 1991 Course D: Focal peripheral neuropathies: selected topics. Rochester, MN: American Association of Electrodiagnostic Medicine; 1991. Criteria Met (2/6: 2,6) Source: AAEM Consultant 1993.
- Robinson LR, Micklesen PJ, Wang L. Optimizing the number of tests for carpal tunnel syndrome. Muscle Nerve 2000;23:1880-1882. Criteria Met (3/6: 3,5,6). Source: Medline Search. Abstract: The combined sensory index (CSI), the sum of three latency differences, median-ulnar across the palm (palmdiff), median-ulnar to the ring finger (ringdiff), and median-radial to the thumb (thumbdiff), has higher sensitivity and reliability for CTS than individual tests. The objective of this study was to develop an approach that minimizes testing but maximizes accuracy. A retrospective study of 300 hands determined that there were endpoints for individual tests that confidently predicted the results of the CSI; for ranges between these endpoints, further testing was required. These ranges were: palmdiff 0-0.3 ms; ringdiff 0.1-0.4 ms; and thumbdiff 0.2-0.7 ms. Therefore, if the results of one of these three tests exceeded these values, it was not necessary to perform all the NCS necessary to calculate a CSI without loss of sensitivity and reliability.
- Robinson LR, Micklesen PJ, Wang L. Strategies for analyzing nerve conduction data: superiority of a summary index over single tests. Muscle Nerve 1998;21:1166-1171. Criteria Met (5/6: 1,2,3,5,6) Source: Medline Search. Abstract: Comparison of three strategies for diagnosing CTS with NCSs: use of a single NCS result; requirement that one, two, or three of three NCSs results to be abnormal; and use of a single summary variable incorporating data from three different NCSs. Sixty-five hands of subjects without clinical CTS were compared with 66 hands with clinical CTS. Three latency differences were measured: median-ulnar (8 cm) midpalmar orthodromic (palmdiff); median-ulnar ring finger (14 cm) antidromic (ringdiff); and median-radial thumb (10 cm) antidromic (thumbdiff). The combined sensory index (CSI) was the sum of these three differences. Sensitivity for the tests was palmdiff 69.7%, ringdiff 74.2%, thumbdiff 75.8%, and CSI 83.1%. Specificity was 95.4-96.9%. Requiring one, two, or three of three tests to be abnormal yielded sensitivities of 84.8%, 74.2%, or 56.1%, respectively, but specificities of 92.3%, 98.5%, and 100%, respectively. We conclude that a combined index improves diagnostic classification over use of single test results.
- Rojviroj S, Sirichativapee W, Kowsuwon W, Wongwiwattananon J, Tammanthong N, Jeeravipoolvarn P. Pressures in the carpal tunnel. A comparison between patients with carpal tunnel syndrome and normal subjects. J Bone Joint Surg Br 1990;72:516-518. Criteria Met (3/6: 1,3,6) Source: Medline Search.
- Rosecrance JC, Cook TM, Bingham RC. Sensory nerve recovery following median nerve provocation in carpal tunnel syndrome. Electromyogr Clin Neurophysiol 1997;37:219-229. Criteria Met (6/6: 1,2,3,4,5,6) Source: Medline Search. Abstract: The latency and amplitude of orthodromic median SNAP from palm to wrist were measured 5 minutes before and at intervals up to 10 minutes until recovery after sustained maximal wrist flexion combined with the fingers simultaneously performing finger flexion against resistance. 35 hands with a clinical diagnosis of CTS were subdivided into 24 with a prolonged baseline latency (+NCS) and 11 with normal latencies (-NCS), and 25 asymptomatic control hands were studied. Four measures were analyzed: difference in latency and amplitude before flexion and at 2 minutes afterward, time for the SNAP amplitude to recover to 95% initial value, and time for latency to return to initial latency. The latency increased only 1-2% in CTS hands compared to controls, but the amplitude decreased to a greater extent (17%) compared to control hands (2%) and the amplitude recovery time was longer. For groups, mean recovery times were 0.6 min controls, 2.25 min CTS (-NCS) group, and, paradoxically, 4.74 min for CTS (-NCS) group. Amplitude recovery time greater than 1.62 min (asymptomatic mean + 2SD) was considered abnormal for individual hands. With this criterion, abnormalities were present in 71% of clinically symptomatic hands, including 8 of 11 without other NCS abnormalities. SNAP recovery time may be complimentary to other NCS to diagnosis CTS but does not replace median orthodromic palm-wrist SNAP latency measurements to diagnose CTS.
- Rosen I. Neurophysiological diagnosis of the carpal tunnel syndrome: evaluation of neurographic techniques. Scand J Plast Reconstr Surg Hand Surg 1993;27:95-101. Criteria Met (4/6: 3,4,5,6) Source: Medline Search. Abstract: Retrospective study of 28 patients diagnosed with CTS on basis of combination of clinical, NCS and EMG data. The median motor DML, orthodromic median SNCV for D1 and D3, palmar mixed median NCV were measured and the quotient of SNCV across CT to forearm were calculated in 86 normal controls and the results compared to the same studies in the 28 CTS patients. The palmar mixed median NCV was superior to the quotient of SNCV across CT to forearm and the other tests for the diagnosis of CTS.
- Rosenberg JN. Anterior interosseous/median nerve latency ratio. Arch Phys Med Rehabil 1990;71:228-230. Criteria Met (4/6: 1,3,5,6) Source: Medline Search. Abstract: With stimulation at the antecubital fossa and simultaneous recording over the APB and pronator quadratus (needle electrode) DMLs were determined from 100 anterior interosseous nerves in 61 normal volunteers, 5 patients with anterior interosseous syndrome, and 35 patients with CTS. The results show abnormal ratios for both CTS and anterior interosseous syndrome.
- Rossi S, Giannini F, Passero S, Paradiso C, Battistini N, Cioni R. Sensory neural conduction of median nerve from digits and palm stimulation in carpal tunnel syndrome. Electroencephalogr Clin Neurophysiol 1994;93:330-334.Criteria Met (4/6: 3,4,5,6) Source: Medline Search. Abstract: A variation of palmar stimulation with more distal stimulation over the metacarpophalangeal interspaces so that the conduction distances was 1-1.5 cm longer than the usual 8 cm orthodromic palmar conduction study. The more distal stimulation was performed to evaluate the median nerve palmar branches to the adjacent surfaces of the index and middle finger (P2), the middle finger and ring finger (P3), and the ulnar palmar branches to the adjacent surfaces of the ring and little finger (P4). The authors noted that the sensitivity of the modified orthodromic palmar study paralleled the sensitivity of orthodromic median sensory digit stimulation studies to diagnose CTS. The modified palmar stimulation technique had the advantages (1) of frequently demonstrating a measurable response in CTS patients with stimulation at P3 whereas the response was absent with stimulation of D4 and (2) of demonstrating an abnormality when the response with stimulation at P2 was normal. Since the authors used NCS criteria to select patients for the study, the clinical sensitivity and specificity of the modified palmar studies could not be calculated although they could compare the sensitivity of one study to another.
- Sackett DL, Straus SE, Richardson WS, Rosenberg W, Haynes RB. Evidence-based medicine: how to practice and teach EBM. New York: Churchill Livingstone: 2000. Background Reference. Source: AAEM 2000 CTS Task Force member.
- Salerno DF, Franzblau A, Werner RA, Bromberg MB, Armstrong TJ, Albers JW. Median and ulnar nerve conduction studies among workers: normative values. Muscle Nerve 1998;21:999-1005. Criteria Met: (normal population study 4/6: 1,2,5,6) Source: Medline Search: Abstract: To determine normative values for NCS among active workers, a prospective cross-sectional study was performed of active workers in contrast to the typical reference populations. The authors selected a subset of 326 workers from 955 subjects who participated in medical surveys in the workplace. Bilateral median (D2) and ulnar (D5) antidromic sensory conduction studies over a 14 cm conduction distance to the wrist were performed after checking midpalm temperature to be 32.0 degrees centigrade or greater with or without warming the limb; limb temperatures were not monitoring during the study (personal communication). Median and ulnar SNAP amplitude and latency (onset and peak) were measured. Workers with upper extremity symptoms, medical conditions that could adversely affect peripheral nerve function, low hand temperature, or highly repetitive jobs were excluded from the “normal” cohort. Linear regression models explained variance in nerve function with covariate of age, sex, hand temperature, and anthropometric factors and provide evidence that electrodiagnostic testing should control for those relevant covariates to improve diagnostic accuracy. The median-ulnar peak latency difference was the best measure to use if corrections are not made to account for relevant covariates. However, the authors noted the 95th percentile at 0.8 ms in active workers in contrast to current standards of 0.4 to 0.5 ms so that current standards for diagnosing CTS among workers appear too sensitive.
- Salerno DF, Werner RA, Albers JW, Becker MP, Armstrong TJ, Franzblau A. Reliability of nerve conduction studies among active workers. Muscle Nerve 1999;22:1372-1379. Criteria Met (worker population study 4/6: 1,3,5,6). Source: Medline Search. Abstract: Prospective study of the inter-examiner and intra-examiner reliability for the measurement of antidromic median (D2) and ulnar (D5) sensory conduction from wrist with conduction distance of 14 cm and without averaging of responses. The first round of testing evaluated inter-examiner reliability in 158 workers by comparison of the results of NCS performed by two different examiners on the same day. The second round of testing was performed 3 weeks later and analyzed data from 58 subjects retested by examiner 1 and 76 subjects retested by examiner 2. Midpalm temperature was recorded at the beginning of testing and subjects with cool hands were warmed to 32 degrees centigrade when possible; temperature was not monitored continuously during the testing. The data was analyzed with and without correction of latency measurements by 0.3 ms for each degree below 35 degrees centigrade. Inter-examiner reliability analysis noted (1) median sensory nerve measurements of amplitude, onset latency, and peak latency were more reliable than ulnar measurements, (2) amplitude and peak latency measurements were more reliable than onset latency measurements, (3) the median-ulnar peak latency difference had consistently high reliability, (4) ulnar onset latency had the poorest reliability. Inter-examiner reliability analysis showed a high congruence between examiners and the same pattern of interexaminer results between median and ulnar measurements as noted in the intra-examiner reliability analysis described above. Temperature correction made a small change in reliability of ulnar latency measurements. Based on these results, the authors recommended that the same examiner perform the repeated NCS in longitudinal studies to minimize inter-examiner variability and use of median-ulnar peak latency differences (in addition to short segment orthodromic median nerve studies) to evaluate patients for CTS.
- Sander HW, Quinto C, Saadeh PB, Chokroverty S. Sensitive medianulnar motor comparative techniques in carpal tunnel syndrome. Muscle Nerve 1999;22:88-98. Criteria Met (5/6: 1,3,4,5,6) Source: Medline Search. Abstract: CTS was diagnosed in 50 patients (79) hands based on a combination of clinical and electrodiagnostic criteria (median palm-wrist mixed NAP onset latency greater than 1.7 ms or onset latency exceed the ipsilateral ulnar palm-wrist latency by more than 0.3 ms as described by Jackson and Clifford in 1988). Three motor conduction studies were evaluated: the median-thenar to ulnar-thenar latency difference (TTLD), the median- thenar to ulnarhypothenar latency difference (THLD), and the ulnar-to-median Fwave latency difference (FWLD). The abnormal cutoffs based upon 34 normal controls are: TTLD, 0.8 ms; THLD, 1.2 ms; FWLD, 0.6 ms. The diagnostic sensitivities were: 95-98%, 85-88%, and 75-78%, respectively, in this CTS patient group with abnormal median sensory conduction studies as described above.
- Scelsa SN, Herskovitz S, Bieri P, Berger AR. Median mixed and sensory nerve conduction studies in carpal tunnel syndrome. Electroencephalogr Clin Neurophysiol 1998;109:268-273. Criteria Met (6/6: 1,2,3,4,5,6) Source: Medline Search. Abstract: To assess the sensitivities and specificities of velocity differences between median mixed nerve conduction across the wrist (Medmxpw) and (I) median mixed nerve conduction in the forearm (Medmxf) and (II) palm to D2 sensory conduction (MedpD2), we prospectively studied 67 limbs of patients with clinically definite carpal tunnel syndrome (CTS). Medmxf and Medmxpw were performed by stimulating the median nerve at the elbow and palm respectively and recording at the proximal wrist crease. We also compared conventional median sensory (D2-wrist) and mixed (palm-wrist) tests in all patients. Thirty limbs of asymptomatic subjects served as normal controls and 21 limbs of subjects with other neuropathies served as diseased controls; control data was collected prospectively. The sensitivity of the MedpD2-Medmxpw difference (0.87) was significantly greater than that of the Medmxf-Medmxpw difference (0.61, P <0.001). Both tests were similar and highly specific (0.98 and 0.96, respectively). The MedpD2-Medmxpw study is among the most sensitive and specific electrophysiologic tests for CTS.
- Schwartz MS, Gordon JA, Swash M. Slowed nerve conduction with wrist flexion in carpal tunnel syndrome. Ann Neurol 1980;8:69-71. Criteria Met (3/6: 1,2,5) Source: Golding, 1986. Abstract: DMLs from the wrist to APB and DSLs from the index finger to the wrist were determined in 32 hands in 20 patients and 10 control subjects. The latencies were determined before and after 2 minutes of full voluntary wrist flexion (Phalen’s maneuver). They found that the DSL or DML increased by greater than 0.2 ms in 16 out of 32 CTS patients and was not greater than 0.1 ms in normal subjects. In 2 CTS patients the only abnormality was the increase in distal latencies after Phalen’s maneuver. Temperature differences before and after wrist flexion were not reported.
- Sener HO, Tascilar NF, Balaban H, Selcuki D. Sympathetic skin response in carpal tunnel syndrome. Clin Neurophys 2000;111:13951199. Criteria Met (6/6: 1,2,3,4,5,6) Source: Medline Search. Abstract: Prospective study of 31 CTS patients and 21 healthy volunteers of the sympathetic skin response (SSR) recorded from D2 and D5 with sternal stimulation. Sternal stimulation was chosen to elicit the SSR instead of limb stimulation to avoid the effect of afferent dysfunction in a limb on the results. The SSR latency recorded from symptomatic limbs of CTS did not differ from normal controls, and the same was true for median-to-ulnar ratios of latency, amplitude and area of the SSR. Of a subset of 23 CTS patients who completed a questionnaire, 70% of CTS patients did complain of sympathetic symptoms in the symptomatic limbs: red or purple discoloration, excessive sweating, or feeling cold (personal communication).
- Seror P. Comparative diagnostic sensitivities of orthodromic or antidromic sensory inching test in mild carpal tunnel syndrome. Arch Phys Med Rehabil 2000; 81:442-446. Criteria Met (4/6: 1,3,5,6) Source: Medline Search. Abstract: Prospective study comparing the orthodromic inching test (OIT) to the antidromic inching test (AIT) in the dominant hand of 20 CTS patients with control data from 20 normal subjects. The diagnosis of the 20 CTS patients was based on clinical criteria and confirmed by NCS. To select cases of definite but mild CTS, the criteria for NCS results was as follows: normal median motor distal latency (<4.0 ms), normal sensory conduction velocity palm-wrist (>45 m/s), and abnormal median-ulnar latency difference of the fourth digit (>0.4ms). Temperature was measured at the start of the study, but not monitored continuously during the study. The IT (100% positive) was superior to the AIT (20% positive) in the 20 CTS patients.
- *Seror P. Comparison of the distal motor latency of the first dorsal interosseous with abductor pollices brevis. Report of 200 cases. Electromyogr Clin Neurophysiol 1988;28:341-345. Criteria Met (1/6: 1) Source: Medline Search.
- Seror P. Orthodromic inching test in mild carpal tunnel syndrome. Muscle Nerve 1998a;21:1206-1208. Criteria Met (4/6: 2,3,5,6). Source: Medline Search. Abstract: Orthodromic inching test (OIT) of the median nerve at wrist was performed on the dominant wrist of 80 controls and 100 patients with mild CTS defined by the presence of clinical features and chosen for study because standard electrodiagnostic tests for CTS were normal (median motor distal latency less than 4 ms and palm-to-wrist orthodromic sensory conduction velocity greater than 45 m/s). In controls the mean conduction delay per centimeter (CD/cm) was 0.184 ms and was slightly higher inside than outside the carpal tunnel; the maximal CD/cm (MCD/cm) was never greater than 0.34 ms (mean 0.247). The MCD/cm was 0.36 ms or more in 96 CTS patients. This abnormality was located within the carpal tunnel in 92% of cases. Outside the entrapment site CD/cm values remained normal and similar to those found in the controls. On the whole, this results in an overall specificity of 100% and sensitivity of 96% for the OIT.
- Seror P. Phalen’s test in the diagnosis of carpal tunnel syndrome. J Hand Surg 1988;13-B:383-385. Criteria Met (3/6: 1,2,6) Source: Medline Search.
- Seror P. Sensitivity of the various tests for the diagnosis of carpal tunnel syndrome. J Hand Surg [Br ] 1994;19:725-728. Criteria Met (5/6: 1,3,4,5,6) Source: Medline Search. Abstract: A prospective study of 150 hands in 96 patients suspected of CTS. Patients were included in the study because at least one EDX test for CTS was abnormal; patients suspected of CTS with normal EDX tests were excluded from the analysis. The data was used to compare the relative sensitivity of nine different EDX tests to diagnose CTS. The distal motor latency was greater than 5 ms in 35% of cases and greater than or equal to 4 ms in 55% of cases. The D3 to wrist (14 cm) orthodromic median sensory CV was less than or equal to 45 m/s in 66% of cases. The palm to wrist (8 cm) orthodromic median CV was less than or equal 45 m/s in 76%. The remaining 24% of cases were assessed by additional EDX tests: the median-ulnar latency difference recorded from D4 was abnormal in 21 of the remaining 24% and the centimetric test was altered in all 24%. The median-ulnar latency difference is simpler to perform than the centimetric test and, in this study, there was only a small difference in the percentage of median nerve abnormalities detected in CTS suspects with these two tests.
- Seror P. The axonal carpal tunnel syndrome. Electroencephalogr Clin Neurophysiol 1996b;101:197-200. Criteria Met (4/6: 1,4,5,6) Source: Medline Search. Abstract: Five patients with clinical symptoms of CTS and a response to a single corticosteroid injection of the CT were studied. Each patient had a normal electrodiagnostic evaluation, including needle examination (C5 to C8T1), distal motor latency, palm to wrist orthodromic sensory conduction velocity, and special tests: median-ulnar latency difference of the 4th digit, palmar centimetric technique. A new test is described: the orthodromic sensory ultra distal stimulation of each digit “at the pulp” with recording over the median nerve at the wrist for digits 1,2,3,4 and over the ulnar nerve for digit 5. The test revealed a significant amplitude change (60-90%) in at least two median digits of the symptomatic hand compared to the asymptomatic hand interpreted as “axonal loss” in these five CTS patients. These findings led to the proposal of the term “axonal CTS.”
- Seror P. Tinel’s sign in the diagnosis of carpal tunnel syndrome. J Hand Surg 1987;12-B:364-365. Criteria Met (3/6: 1,2,6) Source: Medline Search.
- Shafshak TS, el-Hinawy YM. The anterior interosseous nerve latency in the diagnosis of severe carpal tunnel syndrome with unobtainable median nerve distal conduction. Arch Phys Med Rehabil 1995; 76: 471-475. Criteria Met (5/6: 1,3,4,5,6). Source: Medline Search. Abstract: The authors concluded that measurement of the anterior interosseous nerve latency (AINL) with surface electrodes has a role in the differential diagnosis of severe CTS from other causes of median nerve pathology. The alternative is to perform needle EMG examination of forearm muscles innervated by the median nerve.
- Shahani BT, Young RR, Potts F, Maccabee P. Terminal latency index (TLI) and late response studies in motor neuron disease (MND), peripheral neuropathies and entrapment syndromes. Acta Neurol Scand 1979;73(suppl):118. Criteria Met (0/6) (Abstract only) Source: Stevens, 1987.
- Sheean GL, Houser MK, Murray NM. Lumbrical-interosseous latency comparison in the diagnosis of carpal tunnel syndrome. Electroencephalogr Clin Neurophysiol 1995;97:285-289. Criteria Met (4/6: 1,3,5,6) Source: Medline Search. Abstract: In 66 hands of 45 patients with suspected CTS, the second lumbrical-interosseous distal motor latency difference (2LI-DML) was abnormal as frequently (48 hands, 72%) as the median-ulnar orthodromic mixed nerve palmar velocity difference.
- *Shurr DG, Blair WF, Bassett G. Electromyographic changes after carpal tunnel release. J Hand Surg Am 1986;11:876-880. Criteria Met (2/6: 1,2) Source: Medline Search.
- *Silverstein B, Fine L, Stetson D. Hand-wrist disorders among investment casting plant workers. J Hand Surg Am 1987;12:838-844. Criteria Met (0/6) Source: Medline Search.
- Simovic D, Weinberg DH. Terminal latency index in the carpal tunnel syndrome. Muscle Nerve 1997a;20:1178-1180. Criteria Met (3/6: 3,4,5) Source: Medline Search. Abstract: A retrospective study evaluated the usefulness of the median motor terminal latency index (m-TLI) to diagnose CTS. The m-TLI is a derived measure of distal motor conduction and calculated as follows: terminal distance / (proximal conduction velocity × distal latency). The 132 hands of 107 patients suspected of CTS were divided into two groups based on the results of mixed nerve palmar stimulation studies (normal "2.2 ms or median to ulnar peak latency difference "0.4 ms.) Group I contained patients with abnormal median palmar peak latencies (likely to have CTS). while group 2 contains patients with normal median palmar peak latencies (less likely to have CTS). The m-TLI was less than 0.34 in all patients in Group 1 and equal or greater than 0.34 in all patients in Group 2. This retrospective study suggests that the m-TLI is a diagnostic test for CTS potentially as useful as the median palmar conduction study (see 1999b reference).
- Simovic D, Weinberg DH. The median nerve terminal latency index in carpal tunnel syndrome: a clinical case selection study. Muscle Nerve 1999b;22:573-577. Criteria Met: (6/6: 1,2,3,4,5,6) Source: Medline Search. Abstract: The median terminal latency index (TLI) is a calculated value derived from the conventional median motor NCS data. The TLI is a ratio that adjusts the median motor distal latency (DL) for the terminal conduction distance (CD) and the proximal nerve conduction velocity (CV): TLI = terminal CD (mm) /[proximal CV (m/s) × DL (ms)]. The ratio decreases as the conduction time increases across the carpal tunnel. In this prospective study of 66 patients to assess the sensitivity of the median nerve TLI for the diagnosis of carpal tunnel syndrome (CTS), clinical and electrophysiological evaluations were completed by separate, blinded examiners. Based on clinical diagnostic criteria, 54 of the 66 patients (54 hands) were determined to have CTS (CTS group). Control data were obtained from 19 healthy subjects (38 hands). The mean TLI was 0.26 ± 0.04 in the CTS group and 0.43 ±0.04 in the control group (P <0.001). The sensitivity of the TLI for the diagnosis of CTS was 81.5%. The TLI was more sensitive to diagnose CTS than the median motor DL and median sensory peak latency (PL) to the second digit (CD 14 cm). The TLI was always abnormal when the median mixednerve palmar latency was abnormal. In three cases from the CTS group, the TLI was the only abnormal electrophysiological parameter.
- Simpson JA. Electrical signs in the diagnosis of carpal tunnel and related syndromes. J Neurol Neurosurg Psychiatry 1956;19:275-280. Criteria Met (2/6: 3,5) Source: Palliyath, 1990.
- Smith T. Near-nerve versus surface electrode recordings of sensory nerve conduction in patients with carpal tunnel syndrome. Acta Neurol Scand 1998; 98: 280-282. Criteria Met (5/6: 1,3,4,5,6) Source: Medline Search. Abstract: Comparison of the relative sensitivity of sensory nerve conduction (SNC) recorded with near-nerve needle electrodes and SNC recorded with surface electrodes to demonstrate focal slowing of the median nerve conduction in CTS patients. 82 consecutive patients with clinical symptoms and signs of CTS were studied prospectively by the same clinical neurophysiologist. Orthodromic near-nerve recording from digits 1 and 3, distal median motor latency, and antidromic surface recording from palm to digit 2 and wrist to digit 2 were performed in all patients. Near-nerve recording of the ulnar nerve was done in patients with abnormal median nerve conduction. Near-nerve SNC was abnormal compared to control (slowed velocity or absent response) in 52% of the patients from digit 1 to wrist, in 51% from digit 3 to wrist, and 40% had a prolonged distal motor latency. Surface antidromic SNC was abnormal in 49% from wrist to palm, and in 43% from wrist to digit 2. Statistical analysis revealed no significant difference between the near-nerve method and the surface method.
- So YT, Olney RK, Aminoff MJ. Evaluation of thermography in the diagnosis of selected entrapment neuropathies (comments in Neurology 1989;39:1003-1005). Neurology 1989;39:1-5. Criteria Met (2/6: 1,2) Source: Medline Search.
- *Spindler HA, Dellon AL. Nerve conduction studies and sensibility testing in carpal tunnel syndrome. J Hand Surg 1982;7:260-263. Criteria Met (3/6: 2,3,5) Source: Jordan, 1987.
- Stetson DS, Albers JW, Silverstein BA,Wolfe RA. Effects of age, sex, and anthropometric factors on nerve conduction measures. Muscle Nerve 1992;15:1095-1104. (normal population study 5/6: 1,3,4,5,6) Source: Buschbacher 1999. Study of 105 healthy, asymptomatic adults without history of hand-intensive occupational activities. Height and finger circumference was negatively associated with sensory amplitude of median, ulnar and sural nerves. Height was positively associated with median, ulnar and sural sensory distal latencies. Equations using age, height and finger circumference for prediction of normal values are presented. Failure to adjust normal nerve conduction values for these factors decreases the diagnostic specificity and sensitivity of nerve conduction studies.
- Stevens JC. AAEE Minimonograph #26: The electrodiagnosis of carpal tunnel syndrome. Muscle Nerve 1987;10:99-113. Criteria Met (3/6: 3,5,6) Source: Medline Search. Abstract: The author presents (1) the electrodiagnostic findings in 505 cases of CTS evaluated at the Mayo Clinic from 1961-1980, (2) normal values for median and ulnar sensory and motor conduction, (3) an EDX protocol for evaluation of CTS, and (4) a protocol to identify Martin-Gruber anastomosis.
- Stevens JC, Smith BE, Weaver AL, Bosch EP, Deen HG Jr, Wilkens JA. Symptoms of 100 patients with electromyographically verified carpal tunnel syndrome. Muscle Nerve 1999;22:1448-1456. Background Reference. Source: Medline Search. Abstract: To determine the symptoms of carpal tunnel syndrome (CTS), screening evaluations were performed in 244 consecutive patients with sensory symptoms in the hand and unequivocal slowing of median nerve conduction at the wrist. This yielded 100 patients thought to have no explanation other than CTS for their upper limb complaints. These patients completed a hand symptom diagram (HSD) and questionnaire (HSQ) about their symptoms. CTS symptoms were most commonly reported in median and ulnar digits, followed by median digits only and a glove distribution. Unusual sensory patterns were reported by some patients. Based on the HSQ, paresthesias or pain proximal to the wrist occurred in 36.5% of hands. The usefulness of the HSD and HSQ for diagnosis was determined by asking three physicians, blinded to the diagnosis, to rate the likelihood of CTS in the patients with CTS and in 50 patients with other causes of upper extremity paresthesia. The sensitivities of the independent instruments ranged from 54.1% to 85.5%. Based on the combined instrument ratings, the sensitivity increased to 79.3% to 93.7%.
- Stevens JC, Sun S, Beard CM, O’Fallon WM, Kurland LT. Carpal tunnel syndrome in Rochester, Minnesota, 1961-1980. Neurology 1988;38:134-138. Background Reference. Source: Medline Search.
- Steward JD, Eisen A. Tinel’s sign and the carpal tunnel syndrome. Br Med J 1978;2:1125-1126. Criteria Met (1/6: 3) Source: Golding, 1986.
- Szabo RM, Gelberman RH, Dimick MP. Sensibility testing in patients with carpal tunnel syndrome. J Bone Joint Surg 1984;66A:60-64. Criteria Met (1/6: 1) Source: Borg, 1988.
- Tackmann W, Kaeser HE, Magun HG. Comparison of orthodromic and antidromic sensory nerve conduction velocity measurement in the carpal tunnel syndrome. J Neurol 1981;224:257-266. Criteria Met (6/6: 1,2,3,4,5,6) Source: Uncini, 1989. Abstract: Using ring electrodes on the middle finger and subdermal electrodes at the midpalm and wrist, orthodromic and antidromic SNAP latencies were recorded from 56 hands from 50 CTS patients and 32 hands from 32 healthy subjects. They report no significant differences in latencies of orthodromic and antidromic recordings and that palmar latencies are more likely to be abnormal in CTS than digit latencies.
- Tackmann W, Lehman HJ. Relative refractory period of median nerve sensory fibers in the carpal tunnel syndrome. Eur Neurol 1974;12:309-316. Criteria Met (4/6: 1,2,4,5) Source: Palliyath, 1990. Abstract: With stimulation on the index finger and recording at the wrist, the relative median nerve refractory period was determined with paired stimuli in 11 hands of eight CTS patients and 12 hands of eight healthy controls. They found the relative refractory period more likely to be prolonged in patients with CTS as opposed to normal subjects.
- *Terzis S, Paschalis C, Metallinos IC, Papapetropoulos T. Early diagnosis of carpal tunnel syndrome: comparison of sensory conduction studies of four fingers. Muscle Nerve 1998; 21: 15431545. Criteria Met (3/6: 3,5,6) Source: Medline Search. Abstract: Sensory studies of four fingers were performed on 72 patients with early (distal motor latency <4.2 ms) carpal tunnel syndrome (CTS) and on 43 control subjects. Results demonstrate that sensory studies of digit 4 yields the highest sensitivity (88%) for diagnosis of early CTS. The sensitivity of digit 1, digit 2, and digit 3 was 61%, 22%, and 50%, respectively.
- Thomas JE, Lambert EH, Cseuz KA. Electrodiagnostic aspects of the carpal tunnel syndrome. Arch Neurol 1967;16:635-641. Criteria Met (3/6: 3,5,6) Source: Nau, 1988.
- Thomas PK. Motor nerve conduction in carpal tunnel syndrome. Neurology 1960;10:1045-1050. Criteria Met (5/6: 1,2,3,5,6) Source: Wiederholt, 1970. Abstract: With coaxial needle recording over the APB, stimulation at the wrist, elbow, and axilla, CMAPs and DMLs were recorded over the APB in 95 CTS patients and 50 control subjects. The DML was prolonged in approximately two-thirds of the CTS patients.
- Trojaborg W, Grewal RP, Weimer LH, Sheriff P. Value of latency measurements to the small palm muscles compared to other conduction parameters in the carpal tunnel syndrome. Muscle Nerve 1996;19:243-245. Criteria Met (5/6: 1,2,3,5,6). Source: Medline Search. Abstract: Study of 170 hands of 105 patients with clinical diagnosis of CTS. There was an abnormal lumbrical-interosseus latency difference in 83% of hands whereas there was an abnormal median sensory conduction velocity from the thumb to the wrist in 93% of hands. The authors concluded that the lumbrical-interosseus latency difference was especially useful in confirming CTS in patients with absence of the median SNAP or APB motor response or both.
- Uncini A, Di Muzio A, Awad J, Manente G, Tafuro M, Gambi D. Sensitivity of three median-to-ulnar comparative tests in diagnosis of mild carpal tunnel syndrome [see comments]. Muscle Nerve 1993;16:1366-1373. Criteria Met (6/6: 1,2,3,4,5,6). Source: Medline Search. Abstract: Study of 193 hands of 113 patients with clinical diagnosis of CTS compared to reference population of 72 hands of 47 volunteers. Ninety-five (49%) hands had normal median DML ("4.2 ms) and normal or borderline median SNCV from digit 2 stimulation (!45 m/s). In this subpopulation of 95 hands, the authors performed three median to ulnar comparative tests: (1) difference between median and ulnar distal motor latencies recorded from the second lumbrical and interossei muscles (2L-INT); (2) difference between median and ulnar sensory latencies from digit 4 stimulation (D4MD4U); and (3) difference between median and ulnar mixed nerve latencies from palmar stimulation (PM-PU). The 2L-INT difference was greater than or equal to 0.6 ms in 10 (10%) of the subpopulation of 95 hands. PM-PU and D4M-D4U were greater than or equal to 0.5 ms in 53 (56%) and 73 (77%) of the subpopulation of 95 hands, respectively. If each of these three studies were abnormal in the 98 hands with abnormal median DML or median D2S, the maximum sensitivity for the three tests would be (10 + 98 = 108)/193 = 56%, (53 + 98 = 151)/193 = 78%, and (73 + 98 = 171)/193 = 89%. The comparison of median and ulnar sensory conduction across the CT was more sensitive than comparison of median and ulnar motor conduction across the CT. The sensitivity of D4M-D4U might be explained by the funicular topography and consequent greater susceptibility to compression of the cutaneous fibers from the third interspace which, at the distal carpal tunnel, are clumped superficially in the volar-ulnar portion of the median nerve just beneath the transverse ligament.
- Uncini A, Lange DJ, Solomon M, Soliven B, Meer J, Lovelace RE. Ring finger testing in carpal tunnel syndrome: A comparative study of diagnostic utility (comments in Muscle Nerve 1990;13:560). Muscle Nerve 1989;12:735-741. Criteria Met (4/6: 1,2,3,5) Source: Medline Search. Abstract: With stimulation at the wrist and recording over the ring finger, the median and ulnar DSL latency differences were recorded in 43 hands of 33 normals and 42 hands in 32 patients with mild CTS as defined by electrodiagnostic criteria. Standard DML from wrist to APB, and median DSL from wrist to index finger were also determined. They found that the median ulnar difference to the ring finger was more likely to be abnormal than the DML and DSL.
- *Valls J, Llanas JM. Orthodromic study of the sensory fibers innervating the fourth finger. Muscle Nerve 1988;11:546-552. Criteria Met (3/6: 1,3,5) Source: Medline Search.
- Valls-Sole J, Alvarez R, Nunez M. Limited longitudinal sliding of the median nerve in patients with carpal tunnel syndrome. Muscle Nerve 1995; 18: 761-767. Criteria Met (4/6: 1,3,5,6) Source: Medline Search. Abstract: During normal movements or changes in position of the limbs, nerve structures must accommodate the resulting changes in length of the nerve path. In patients with CTS, we monitored electrophysiologically the longitudinal adjustment of the median nerve to positions of extreme flexion and extreme extension of the wrist and elbow, by measuring the differences induced in the latency of the SNAP recorded in the forearm and upper arm. In patients, the latency difference was significantly shorter than in normal subjects (0.196 ± 0.084 ms vs. 0.088 ± 0.059 ms in the forearm, and 0.485 ± 0.122 ms vs. 0.129 ± 0.086 ms in the upper arm). These results indicate that the displacement of the source of the median nerve SNAP with movements of flexion and extension is limited in patients with carpal tunnel syndrome. Since the latency changes in CTS patients were less than but within the range of latency changes in normal controls, the procedure cannot be used to distinguish CTS patients from controls. However, the abnormality noted may be a manifestation of the pathophysiology of entrapment syndromes: limited longitudinal sliding of nerves in entrapment neuropathies.
- Vennix MJ, Hirsh DD, Chiou-Tan FY, Rossi CD. Predicting acute denervation in carpal tunnel syndrome. Arch Phys Med Rehabil 1998;79:306-312. Criteria Met (3/6: 3,4,6) Source: Medline Search. Abstract: Retrospective study of 1590 patients diagnosed with median neuropathy at the wrist based on the results of NCS alone to determine the relationship of evidence of acute denervation on needle EMG of the APB to patient age, gender, and NCS parameters including median sensory peak latency and amplitude, and median motor distal latency and amplitude. Logistic regression analysis identified gender, median motor distal latency, and median motor amplitude (all p ".008) as contributing to the prediction of denervation. Needle EMG of the cases with a median CMAP amplitude <7 mV detected 95.3% (141/148) of all cases with denervation. However, the model is not applicable for predicting the presence of denervation in the individual patient.
- Verghese J, Galanopoulou AS, Herskovitz S. Autonomic dysfunction in idiopathic carpal tunnel syndrome. Muscle Nerve 2000;23:12091213. Criteria Met (5/6 1,3,4,5,6) Source: AAEM CTS Task Force 2000 member. Abstract: A prospective study of autonomic disturbances in 139 limbs of 76 CTS patients diagnosed on the basis of clinical and sensory and motor NCS abnormalities. Autonomic disturbances were identified as follows: swelling of the fingers (39%), dry palms (33%), Raynaud’s phenomenon (32%) and blanching of the hand (32%), finger tip ulcerations (0%) and nail changes (0%). Cold sensation of the fingertips (too non-specific) and excessive sweating (not reported in a preliminary survey) were not included. Sympathetic Skin Response (SSR) abnormalities (latency >1.72 ms or absent response) were noted in 24% (33 of 139) symptomatic hands and were more common in hands with autonomic symptoms (34%; 26 of 76 hands). Compared to control patients, the SSR had a specificity of 89%.
- Wang AK, Raynor EM, Blum AS, Rutkove SB. Heat sensitivity of sensory fibers in carpal tunnel syndrome [see comments]. Muscle Nerve 1999;22:37-42. Criteria Met (5/6: 1,3,4,5,6) Source: Medline Search. Abstract: CTS used as a model to study the effect of heat on nerves with focal demyelination secondary to chronic compression. Median SNAP amplitude and area decreased more in 12 CTS patients than in 12 normal controls at 42 degree C compared to baseline measurements at 32 degrees centigrade. It is hypothesized that these reductions in response amplitude are secondary to the occurrence of heat-induced conduction block in demyelinated sensory neurons.
- Werner RA, Albers JW. Relation between needle electromyography and nerve conduction studies in patients with carpal tunnel syndrome. Arch Phys Med Rehabil 1995;76:246-249. Criteria Met (2/6: 3,6) Source: Medline Search. Abstract: Retrospective study of 480 cases of electrodiagnostically confirmed CTS reviewed to determine if the findings on NCS could predict the presence or absence of fibrillation potentials or motor unit changes on the needle EMG of the APB. Two hundred thirty-one CTS patients had an abnormal needle EMG exam defined by presence of fibrillation activity (105 patients) and/or abnormal MUAP configuration. Motor and sensory evoked potential latencies were the most important predictors of an abnormal needle EMG examination.
- Werner RA, Bir C, Armstrong TJ. Reverse Phalen’s maneuver as an aid in diagnosing carpal tunnel syndrome. Arch Phys Med Rehabil 1994;75:783-786. Criteria Met (6/6, 1,2,3,4,5,6) Source: Medline Search. Abstract: Direct intracarpal canal pressure measurements in 5 subjects demonstrated that a reverse Phalen’s maneuver (wrist and finger extension) results in a significantly higher intracarpal canal hydrostatic pressure compared to a traditional Phalen’s (wrist flexion and finger extension) or a modified Phalen’s maneuver (wrist flexion while pinching a flat object between the thumb and third digit). 31 individuals with a clinical diagnosis of carpal tunnel syndrome and 20 normal controls were evaluated to determine the effect the reverse Phalen’s maneuver would have on antidromic median sensory latency and amplitude measured with the wrist and hand in the neutral position. Both groups demonstrated slight (1-4%) prolongation of the peak latency and reduction in the amplitude of the median SNAP after 1 minute of this maneuver. The control group had a mean peak latency prolongation of 0.05 ms (1.6% of the mean) and a mean amplitude reduction of 1.5 microvolts (2.6% of the mean) compared to 0.13 ms (3% of the mean) and 0.9 microvolts (4% of the mean) in the carpal tunnel syndrome group. Only the change in peak latency measurements between the two groups was significant at a p = 0.05 level. Additional studies with longer periods of maintained wrist extension were recommended to evaluate this technique to diagnose CTS.
- Werner RA, Franzblau A, Albers JW, Armstrong TJ. Median mononeuropathy among active workers: are there differences between symptomatic and asymptomatic workers? Am J Ind Med 1998;33:374-378. Criteria Met: (worker population study 3/6: 1,3,6). Source: Medline Search. Abstract: A prospective cross-sectional study of 700 active workers identified 184 with median neuropath defined as a prolongation of the median SNAP peak latency compared to the ulnar SNAP peak latency by at least 0.5 ms, antidromic studies, conduction distances 14 cm each to D2 and D5. Cool hands were warmed before testing but temperature was not monitored in every case during the testing. A review of self-reported symptoms of pain, numbness, tingling and burning in the hands or fingers lasting more than 1 week or occurred 3 or more times at the of the screening was used to identify “symptomatic” workers. Workers who complained of symptoms were more likely to be female, to have jobs with higher hand repetition levels, to have higher ratings of job security, not to have a history of diabetes, to use more force in their job with more abnormal postures of their wrist and fingers, and to have a trend toward a more prolonged median sensory distal latency. As noted by the authors, the study is limited because it is cross-sectional and cannot answer many of the questions raised: a longitudinal study would be necessary to determine the incidence and natural history of median mononeuropathy among active workers.
- White JC, Hansen SR, Johnson RK. A comparison of EMG procedures in the carpal tunnel syndrome with clinical-EMG correlations. Muscle Nerve 1988;11:1177-1182. Criteria Met (3/6: 1,2,3) Source: Medline Search. Abstract: Two hundred one hands in 122 patients were evaluated with several techniques for CTS. The asymptomatic hands of 43 of these patients served as controls. The following techniques were evaluated: (a) DML from wrist to APB, (b) DSL from wrist to index finger, (c) motor inching studies across the wrist to APB, (d) sensory inching studies across the wrist to the index finger, (e) inching studies to the lumbrical, (f) palm-to-wrist median latency, (g) comparison of median and radial DSLs, and (h) terminal latency index. Motor inching studies were most likely to be abnormal in both the CTS group and asymptomatic group. Motor inching studies were abnormal in 92% of mild CTS hands and 72% of the asymptomatic hands. All of the studies had high rates of abnormality in asymptomatic hands varying from 9% to 72%.
- Wiederholt WC. Median nerve conduction velocity in sensory fibers through carpal tunnel. Arch Phys Med Rehabil 1970;51:328-330. Criteria Met (normal population study 5/6: 1,3,4,5,6) Source: Macleod, 1987. Abstract: With stimulation over the middle finger and recording distal and proximal to the carpal tunnel, sensory NCVs were determined across the carpal tunnel and proximal to the carpal tunnel in 30 normal adults. Sensory NCV was faster proximal to the carpal tunnel than across the carpal tunnel. No CTS patients were studied.
- Wilbourn AJ: Electrodiagnosis of plexopathies. In: Aminoff MJ, editor. Neurologic clinics: symposium on electrodiagnosis. Vol 3, No 3:511-529. Philadelphia: WB Saunders; 1985. pp. 512-516. Criteria Met: Background Source: AAEM Consultant 1993.
- Wilbourn AJ, Lambert EH. The forearm median-to-ulnar nerve communication; electrodiagnostic aspects (abstract). Neurology 1976:26:368. Background Source: AAEM Consultant 1993.
- Wilson JR. Median mixed nerve conduction studies in the forearm: evidence against retrograde demyelination in carpal tunnel syndrome. J Clin Neurophysiol 1998;15:541-546. Background Reference. Source: Medline Search. Abstract: Motor conduction velocity (CV) measurements sometimes show conduction velocity slowing in the forearm segment of the median nerve in carpal tunnel syndrome (CTS). This slowing of motor nerve conduction is thought to be caused by either retrograde demyelination in the forearm or conduction block of the fastest fibers within the carpal tunnel. Direct measurement of the forearm segment of the median nerve were made to distinguish between these two possibilities. Median motor conduction studies and mixed nerve action potential (MNAP) recordings were performed on the forearm segment of the median nerve in patients (n = 32 limbs, aged 24 to 76) and controls (n = 15 limbs, aged 33 to 76). The results strongly support the hypothesis that the slowing seen in the forearm is caused by conduction block of the fastest conducting fibers within the carpal tunnel and is not caused by retrograde demyelination.
- *Winn FJ Jr, Krieg EF Jr. A regression model for carpal tunnel syndrome. Proc Soc Exp Biol Med 1989;192:161-165. Criteria Met (2/6: 1,2) Source: Medline Search.
- Woltman HW. Neuritis associated with acromegaly. Arch Neurol Psychiatry 1941;45:680-682. Background Reference. Source: Gelbermann, 1980.
- Wongsam PE, Johnson EW, Weinerman JD. Carpal tunnel syndrome: use of palmar stimulation of sensory fibers. Arch Phys Med Rehabil 1983;64:16-19. Criteria Met (3/6: 3,5,6) Source: Pease, 1989. Abstract: With stimulation at the wrist and midpalm and recording with ring electrodes over the middle finger, DSLs were obtained from the median nerve and 100 hands from 50 normal subjects, 15 patients with early CTS, and 6 with diabetes mellitus and superimposed median nerve entrapment. Amplitudes and durations of the SNAP were also reported. This technique is reported as useful in the diagnosis of CTS and underlying mild peripheral neuropathy.
- You H, Simmons Z, Freivalds A, Kothari MJ, Naidu SH. Relationships between clinical symptom severity scales and nerve conduction measures in carpal tunnel syndrome. Muscle Nerve 1999;22:497-501. Criteria Met (5/6: 1,3,4,5,6). Source: Medline Search. Background Reference. Abstract: This study examined the severity of symptoms in carpal tunnel syndrome (CTS) in relation to nerve conduction measures of the median nerve. Significant relationships identified among the clinical scales resulted in a dichotomous symptom classification scheme into primary symptoms more specific for nerve injury (numbness, tingling, nocturnal symptoms) and secondary symptoms (pain, weakness, clumsiness). There were significant relationships between symptom severity and nerve conduction abnormality, and the primary symptom scale correlated more strongly with the electrodiagnostic measures of nerve injury than did the secondary symptom scale.
- Zachary RB. Thenar palsy due to compression of the median nerve in the carpal tunnel. Surg Gynecol Obstet 1945;81:213-217. Background Reference. Source: Gelbermann, 1980.
Document History
AAEM PRACTICE TOPIC IN ELECTRODIAGNOSTIC MEDICINE
American Association of Electrodiagnostic Medicine
2621 Superior Dr. NW, Rochester, MN 55901 (507/288-0100)
© 2002 American Association of Electrodiagnostic Medicine Muscle Nerve 25: 918–922, 2002
Approved by the Board of Directors of the American Association of Electrodiagnostic Medicine: May 2002.
AAEM would like to thank the following who reviewed the manuscript and made helpful suggestions: Gary M. Franklin, MD; Catherine A. Zahn MD; Milton Alter, MD, PhD; Stephen Ashwal, MD; John R. Calverley, MD; Richard M. Dubinsky, MD; Jacqueline French, MD; Michael Glantz, MD; Gary S. Gronseth, MD; Deborah Hirtz, MD; James Stevens, MD; William Wiener, MD; William W. Campbell, MD; Joseph V. Campellone Jr, MD; William H. Cooper, MD; Earl J. Craig, MD; Richard M. Dubinsky, MD; Kenneth James Gaines, MD; James F. Howard, MD; John C. Kincaid, MD; Yuen T. So, MD, PhD; Frederick M. Vincent, MD; Robert A. Werner, MD, MS; Daniel Dumitru MD, PhD; Jacqueline J. Wertsch, MD; Neil A. Busis, MD; Lois M. Nora, MD, JD; Murray E. Brandstater MBBS, PhD, FRCP; John C. Kincaid, MD; Lawrence Robinson, MD; Richard K. Olney, MD; Donna L. Frankel, MD; and Janice M. Massey, MD.
This guideline is greater than 5 years old. Every five years, an interim literature search is performed and the guideline is reviewed. While new studies have been published since this guideline was last reviewed, the Practice Panel Committee of the AANEM has determined that these studies are not sufficient to mandate a revision of this guideline and the recommendations offered are still relevant to current practice.
Reaffirmed by the Practice Issue Review Panel: March 2015, October 2020
Creation of New Guidelines, Consensus Statements, or Position Papers
AANEM members are encouraged to submit ideas for papers that can improve the understanding of the field. The AANEM will review nominated topics on the basis of the following criteria:- Members’ needs
- Prevalence of condition
- Health impact of condition for the individual and others
- Socioeconomic impact
- Extent of practice variation
- Quality of available evidence
- External constraints on practice
- Urgency for evaluation of new practice technology