Consensus Criteria for the Diagnosis of Partial Conduction Block
Author: Richard K. Olney, MD. Limited empiric data are available that suggest the upper limit of normal for changes in amplitude, area, and duration of the CMAP over distance in healthy control subjects. For the median and ulnar nerves with comparison of elbow to wrist stimulation, the normal range at least extends to an increase in duration of 25%, a decrease in amplitude of 25%, and a decrease in area of 20%, with similar changes for more proximal segments.3,5,8,10 For the peroneal nerve with comparison of knee to ankle stimulation, the limits of normal at least permit an increase in duration of 30%, a decrease in amplitude of 30%, and a decrease in area of 25%.7,10,11 For the tibial nerve with comparison of knee to ankle stimulation, the normal range at least extends to an increase in duration of 30%, a decrease in amplitude of 50%, and a decrease in area of 30%.7,11 These consensus criteria have been developed because empiric data do not distinguish temporal dispersion from partial conduction block, and this distinction is important clinically. Criteria for partial conduction block that are proposed in this consensus document are conservative. A strong consensus supports that these criteria need to be more conservative for lower limb nerves than for upper limb nerves, because lower limb stimulation sites are more widely separated. Furthermore, a strong consensus exists that partial conduction block cannot be reliably recognized in the context of severe axon loss. Until empiric data becomes available to support a different criterion for severe axon loss, the expert panel recommends that an amplitude below 20% of the lower limit of normal at the most distal stimulation site is sufficiently small to preclude the confident recognition of partial conduction block.
The American Association of Electrodiagnostic Medicine (AAEM) would like to acknowledge the following expert panel: James W. Albers, MD, PhD; William F. Brown, MD, FRCP(C); Jasper R. Daube, MD; Gerald Felsenthal, MD; Jun Kimura, MD; Richard A. Lewis, MD; Robert G. Miller, MD; Shin J. Oh, MD; Gareth J.G. Parry, MB, ChB; Jack Petajan, MD, PhD; and Austin J. Sumner, MD.
The AAEM would also like to thank the AAEM Quality Assurance Committee for participating in the Delphi process: Chair: Cheryl F. Weber, MD; Members: Faye Y. Chiou-Tan, MD; Sudhansu Chokroverty, MD, FRCP; Earl R. Hackett, MD; Robert L. Harmon, MD, MS; Tim Lachman, MD; Kevin R. Nelson, MD; Atul T. Patel, MD; Caroline A. Quartly, MD, FRCP(C); and John R. Wilson, MD.
Key Words: conduction block • temporal dispersion
INTRODUCTION
Physicians are often required to make diagnostic or therapeutic decisions for conditions in which empiric data and knowledge are incomplete or inconclusive. In such settings, the development of a consensus from an appropriate group of experts is often helpful in focusing research on the critical questions and in providing interim guidance until the questions are answered empirically. Because the need for establishing consensus criteria is common, clinical health research has developed consensus methods over the past 3 decades.
A 4-round modified Delphi process was used to develop this consensus.4 A member of the American Association of Electrodiagnostic Medicine (AAEM) Quality Assurance Committee was chosen to draft the document. An expert panel was then chosen from AAEM members who were authors of articles involving concepts relevant to conduction block and who held divergent opinions at the start of the consensus development process. The author wrote an initial draft that was circulated amongst the members of the expert panel for unsolicited comments. Based on these comments and areas of apparent agreement and disagreement, the document was revised by the author and circulated for a second time, together with 11 questions that focused on areas of comment and concern. After a second revision by the author, the document was circulated for a third round of comments with 7 more narrowly focused questions.
After a third revision by the author, the panel met to discuss remaining areas of concern and to finalize this document. The document was then circulated to the AAEM Board of Directors for a fourth round of input and approval.
Conduction block of an intact motor axon prevents the transmission of its impulses from the anterior horn cell to the muscle it innervates. Conduction block of an intact peripheral sensory axon prevents the transmission of its impulses from its sensory receptor to its cell body in the dorsal root ganglion. Partial conduction block of a nerve is a pathophysiological process that produces motor or sensory deficits (that is, weakness or loss of sensation) if a sufficient portion of its axons have conduction block. However, partial conduction block can only be reliably assessed in the motor axons of a nerve. Partial conduction block that persists for more than a week is diagnostic of focal demyelination.
Temporal dispersion is a physiological or pathophysiological process that has not been established to produce motor or sensory deficits. Physiological temporal dispersion occurs diffusely along the length of a nerve to a minor degree in normal subjects. Pathophysiological or abnormal temporal dispersion is the result of an abnormally increased range of conduction velocities among the individual axons of a nerve. It can be seen along the length of a nerve in axonal loss and in diffuse demyelinating lesions of peripheral nerve. Temporal dispersion may occur focally along a short segment of a nerve to a major degree, in which case it is diagnostic of focal demyelination, but may not be relevant to the pathophysiology of motor or sensory symptoms.
Although these concepts are well accepted, the various practical or operational definitions are controversial. One major purpose of this consensus statement is the development of a definition for the pathophysiological findings by which partial conduction block of a nerve can be diagnosed with a high level of confidence (definite partial or complete conduction block), and can be inferred with a moderate level of confidence (probable partial conduction block).
The criteria that follow are intended to serve several purposes. First, they provide diagnostic guidelines for electrodiagnostic medicine (EDX) consultants. A strong consensus of the expert panel supports the need for such diagnostic guidelines at present, until more empiric data are available. The expert panel anticipates that these criteria will require periodic revision as such empiric data become available. Second, they provide proposed diagnostic categories for research studies and clinical trials. Third, they are intended to stimulate further discussion and research about partial conduction block and its distinction from temporal dispersion. The criteria are not meant to exclude the diagnosis of a demyelinating neuropathy, because such a diagnosis includes consideration of clinical findings and laboratory results in addition to EDX abnormalities.
PROPOSED CRITERIA FOR THE ELECTRODIAGNOSIS OF CONDUCTION BLOCK
1. Technical considerations: a. All measurement of amplitude, area, and duration in these criteria refers to values for the negative peak of surface recorded compound muscle action potentials (CMAPs). The negative peak is defined as that component aspect of the waveform from the first negative deflection of the CMAP from the baseline to its first baseline crossing from negative to positive. CMAPs that have more than 1 negative peak are referred to as multiphasic CMAPs. b. These criteria are intended to apply only tonerves in which the negative-peak amplitude of the CMAP with distal stimulation is 20% or more of the lower limit of normal. c. The percent reduction in Table 1 is applicable toulnar nerve in the forearm only if median-toulnar nerve crossover in the forearm (MartinGruber anastomosis) has been excluded by the recording of an initially positive hypothenar CMAP with stimulation of median nerve at the elbow. Furthermore, usage of excessive stimulation intensity at the wrist that activates both median and ulnar nerves may result in the suggestion of partial conduction block in the forearm segment of the median nerve due to ulnar innervation of deep thenar muscles. d. Although the specificity for determining partialconduction block is similar for median and ulnar nerves when stimulating at the axilla or Erb’s point (EP), the sensitivity is often lower with these proximal stimulation sites for the median nerve unless collision stimulation techniques are used. This is because of the common ulnar innervation of deep thenar muscles. e. The criteria are more restrictive for the radial,peroneal, and tibial nerves than for the median and ulnar nerves. Even with surface recording of the CMAP, the vast majority of the expert panel agree that reduction of amplitude and area of the radial motor response is considered sufficient only to support probable partial conduction block. Ahigher percentage reduction in amplitude and area is required for the peroneal and tibial nerves than for the median and ulnar nerves. Furthermore, greater care is necessary to insure that stimulation is supramaximal at the knee for the tibial nerve; special stimulation techniques may need to be utilized. f. Stimulation at EP and at the sciatic notch (SN)with surface electrical or magnetic stimulator, or stimulation at SN with a needle, is not accepted by many of the panel as sufficiently reliable in producing supramaximal stimulation to be included in the criteria for definite partial conduction block. However, the expert panel accepts that the probability of achieving supramaximal stimulation is high if maximal amplitude and area of the CMAP is achieved with stimulus intensity at 70% or less of maximal stimulator output (in other words, the stimulator is able to deliver a supramaximal stimulus that is 30% more than maximal intensity). g. With the commercial stimulators that are presentlyavailable in the United States, neither needle nor magnetic stimulation of nerve roots is accepted as sufficiently reliable in producing supramaximal stimulation of demyelinated nerve roots to be included in these criteria. h. These criteria do not fully encompass all factorsthat experienced EDX consultants consider before interpreting that partial conduction block is present. For example, certain anatomical variations such as body weight and limb edema are difficult to quantify. To insure that supramaximal stimulation has been achieved, greater caution is required in obese rather than thin individuals and in limbs with edema. 2. Criteria for partial conduction block of motor fibers: a. Definite partial conduction block can be identi-fied, and probable partial conduction block can be suggested, when temporal dispersion is minimal (duration of the CMAP is increased by 30% or less over the specified segment). The criteria for definite and probable partial conduction block are summarized by nerve and segment in Table 1. Identifying definite or probable partial conduction block over any of the long segments identified in Table 1 (segments of 10 cm or more) requires reduction in amplitude or area of the specified amount over a segment without significant temporal dispersion. b. Partial conduction block over a long segmentcan only be suggested when temporal dispersion is moderate (duration of the CMAP is increased by 31% to 60% over the segment). Criteria for probable conduction block are summarized in Table 1. Reduction in amplitude or area of the specified amount over a long segment is required, but the expert panel strongly prefers that reduction exceed the specified amount for amplitude and area. c. Partial conduction block over a long segmentcan only be suspected when temporal dispersion is marked (duration of the CMAP is increased more than 60%) or if the CMAP is multiphasic. d. If the criteria are fulfilled for probable partialconduction block in a long segment of a nerve with minimal temporal dispersion (that is, duration is increased by 30% or less), the level of confidence in the presence of partial conduction block may be increased to definite if amplitude and area are reduced by 20% or more and duration is increased by 10% or less between stimulation sites that are separated by 3 cm or less (a short segment). Identifying definite partial conduction block in a long segment of nerve with moderate or marked temporal dispersion requires reduction in amplitude and area by 20% or more over a segment of 3 cm or less without significant temporal dispersion (that is, duration is increased by 10% or less). To identify probable conduction block over a segment of 3 cm or less requires reduction in amplitude and area by 10% without significant temporal dispersion. 3. Partial conduction block of sensory fibers may be suspected, but cannot be established, with conventional surface recording techniques. COMMENTS ON PARTIAL CONDUCTION BLOCK
However, these data limits of normal do not consider the effects of aging. In older patients the increase in duration and decrease in amplitude (and, to a lesser extent, decrease in area) are more prominent than in young patients.10 Furthermore, these data do not address the pathophysiology of changes that exceed these limits. In particular, abnormalities that exceed these limits may be produced by temporal dispersion from axonal lesions or demyelination, or by partial conduction block from demyelination. Reliable and objective techniques that clearly distinguish between prominent temporal dispersion and partial conduction block in intact human nerve(s) are not available.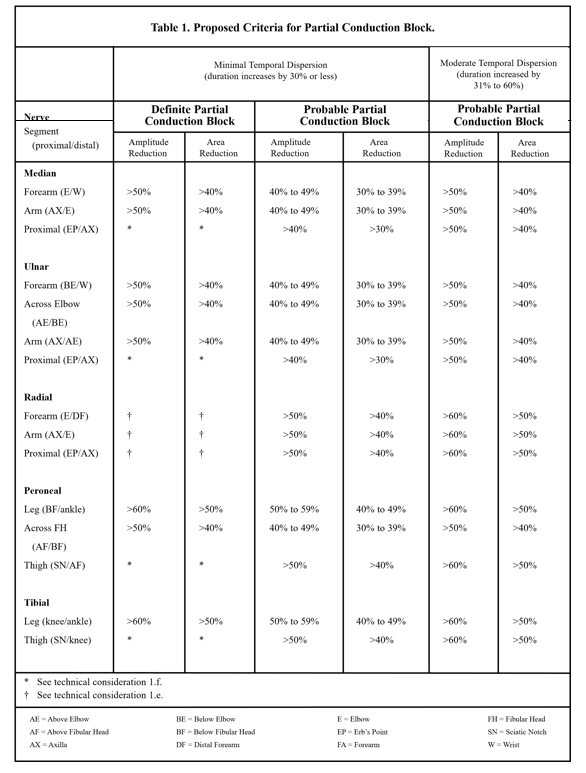
The degree of amplitude and area reduction that has been required to support partial conduction block in clinical studies has ranged from 20% to 50% for amplitude and 20% to 40% for area.1,6 In a computer simulation study of conduction block, amplitude reduction of 85% and area reduction of 50% was achieved with temporal dispersion as conduction distance approached 50 cm.9 However, this computer simulation was based on individual motor unit action potentials (MUAPs) recorded from the surface of a rat’s intrinsic foot muscle, and the representative MUAP was biphasic. The effect of phase cancellation among polyphasic MUAPs is difficult to determine but is expected to be greater. A previous consensus publication has suggested caution in the diagnosis of conduction block when stimulation sites are separated by more than 4 cm and when the stimulated nerve is deep at the proximal stimulation site.2
The expert panel was evenly divided on the issue of requiring area measurement for the diagnosis of partial conduction block in all cases, but did strongly favor the use of area if amplitude reduction is abnormal and temporal dispersion is moderate. At present, the expert panel recommends that marked temporal dispersion (an increase in duration over 60%) is sufficient to preclude the confident recognition of partial conduction block. A strong consensus of the expert panel encourages the need for more caution in using responses elicited from stimulation at EPand the SN sites to support partial conduction block because of the depth of nerves at these stimulation sites. The expert panel was evenly divided on the reliability of restrictive stimulation requirements to insure the delivery of supramaximal stimulation at these sites. Because the delivery of supramaximal stimulation to a demyelinated nerve root cannot always be certain, a strong consensus supports that nerve root stimulation is not presently considered sufficiently reliable to document partial conduction block.DISCLAIMER
This report is provided as an educational service of the AAEM. It is based on an assessment of the current scientific and clinical information. It is not intended to include all possible methods of care of a particular clinical problem, or all legitimate criteria for choosing to use a specific procedure. Neither is it intended to exclude any reasonable alternative methodologies. The AAEM recognizes that specific patient care decisions are the prerogative of the patient and his/her physician and are based on all of the circumstances involved.
References
- Brown WF, Feasby TE: Conduction block and denervation in Guillain-BarrJ polyneuropathy. Brain. 1984; 107:219-239.
- Cornblath DR, Sumner AJ, Daube J, Gilliat RW, Brown WF, Parry GJ, Albers JW, Miller RG, Petajan J: Conduction block in clinical practice. Muscle Nerve. 1991; 14:869-871.
- Felsenthal G, Teng CS: Changes in duration and amplitude of the evoked muscle action potential (EMAP) over distance in peroneal, median, and ulnar nerves. American Journal of Physical Medicine. 1983; 62:123-134.
- Jones J, Hunter D: Consensus methods for medical and health services research. Bmj. 1995; 311:376-380.
- Kimura J, Machida M, Ishida T, Yamada T, Rodnitzky RL, Kudo Y, Suzuki S: Relation between size of compound sensory or muscle action potentials and length of nerve segment. Neurology. 1986; 36:647-652.
- Lewis RA, Sumner AJ, Brown MJ, Asbury AK: Multifocal demyelinating neuropathy with persistent conduction block. Neurology. 1982; 32:958-964.
- Oh SJ, Kim DE, Kuruoglu HR: What is the best diagnostic index of conduction block and temporal dispersion? Muscle Nerve. 1994; 17:489-493.
- Olney RK, Miller RG: Conduction block in compression neuropathy: Recognition and quantification. Muscle Nerve. 1984; 7:662-667.
- Rhee EK, England JD, Sumner AJ: A computer simulation of conduction block: Effects produced by actual block versus interphase cancellation. Ann Neurol. 1990; 28:146-156.
- Taylor PK: CMAP dispersion, amplitude decay, and area decay in a normal population. Muscle Nerve. 1993; 16:1181-1187.
- Weber F: Conduction block and abnormal temporal dispersion - diagnostic criteria. Electromyogr Clin Neurophysiol. 1997; 37:305-309.
Document History
Approved by the American Association of Neuromuscular & Electrodiagnostic Medicine: March 1999.
Muscle Nerve 22: Supplement 8: S225-S229, 1999
Creation of New Guidelines, Consensus Statements, or Position Papers
AANEM members are encouraged to submit ideas for papers that can improve the understanding of the field. The AANEM will review nominated topics on the basis of the following criteria:- Members’ needs
- Prevalence of condition
- Health impact of condition for the individual and others
- Socioeconomic impact
- Extent of practice variation
- Quality of available evidence
- External constraints on practice
- Urgency for evaluation of new practice technology
