Cervical Radiculopathy
American Association of Electrodiagnostic Medicine
American Academy of Physical Medicine and Rehabilitation
ABSTRACT
Cervical radiculopathy is a common cause of morbidity. Its management often requires clinical, electrodiagnostic, and radiological evaluation, and its treatment may include surgery. Based on a critical review of the literature, electrodiagnostic evaluation is found to be moderately sensitive and highly specific in establishing a diagnosis of cervical radiculopathy. This document defines the guidelines and options for the electrodiagnostic medicine consultation of patients with suspected cervical radiculopathy.
INTRODUCTION
The Quality Assurance (QA) Committee of the American Association of Electrodiagnostic Medicine (AAEM) was charged to conduct a critical review of the literature on the usefulness of electrodiagnostic medicine (EDX) studies in cervical radiculopathy. The review focused on the use of the needle electromyographic (EMG) examination, the most widely adopted method for the evaluation of cervical radiculopathy.Developed by the following members of the American Association of Electrodiagnostic Medicine (AAEM) Quality Assurance Committee: Primary Author: Yuen T. So, MD, PhD; Chair: Cheryl F. Weber, MD; Member: William W. Campbell, MD, MSHA.
The AAEM would also like to acknowledge the help of the following: Murray E. Brandstater, MBBS, PhD, FRCP(C); Neil A. Busis, MD; Dorothy J. Carroll, MD, FRCP (C); Sudhansu Chokroverty, MD, FRCP; Faye Y. Chiou-Tan, MD; Janice L. Cockrell, MD; Leslie J. Dorfman, MD; Daniel Dumitru, MD, PhD; Michael K. Greenberg, MD; Ludwig Gutmann, MD; Earl R. Hackett, MD; Robert L. Harmon, MD, MS; M. David Jackson, MD; Tim Lachman, MD; Francis P. Lagattuta, MD; Trilok N. Monga, MD; Kevin R. Nelson, MD; Richard K. Olney, MD; Atul T. Patel, MD; Lawrence H. Phillips II, MD; Rhonda M. Pridgeon, MD; Caroline A. Quartly, MD, FRCP (C); Donald B. Sanders, MD; Kathryn A. Stolp-Smith, MD, MS; Robert L. Sufit, MD; Jacqueline J. Wertsch, MD; John R. Wilson, MD; and Claire V. Wolfe, MD.
Key words: cervical radiculopathy • electrodiagnosis • EMG • electromyography • spinal root compression • spondylosis • neuromuscular disease
Forty-six articles that described original EDX findings in patients suspected to have cervical radiculopathy were identified. All of these articles were reviewed, and 22 were found to provide sufficient and relevant information regarding the usefulness of the needle EMG examination. A set of 6 criteria were used to evaluate the scientific merits of each study. One study met all 6 criteria, and 8 studies met 4 or 5 criteria. The remaining 13 studies met 2 or 3 criteria.
LITERATURE CLASSIFICATION CRITERIA
- Prospective study design.
- Diagnosis of cervical radiculopathy independent of EDX findings.
- Exclusion of other upper extremity pathology that could confound EDX results.
- Sufficient description of the EDX procedure.
- Clearly stated criteria for electrodiagnosis of cervical radiculopathy.
- Results presented in sufficient detail to permit determination of the sensitivity and/or specificity of the EDX procedure.
DEFINITIONS FOR CLASSIFICATION OF EVIDENCE
- Class A evidence: studies that meet all 6 literature classification criteria.
- Class B evidence: studies that meet 4 or 5 literature classification criteria.
- Class C evidence: studies that meet 3 or fewer literature classification criteria.
DEFINITIONS OF PRACTICE RECOMMENDATION STRENGTHS
- Practice standards: Generally accepted principles for patient management which reflect a high degree of clinical certainty (Class A evidence).
- Practice guidelines: Recommendations for patient management which reflect moderate clinical certainty (Class B evidence).
- Practice options/advisories: Other strategies for patient management for which the clinical utility is uncertain (Class C evidence).
PRACTICE RECOMMENDATIONS
The EDX consultation in patients with suspected cervical radiculopathy should include a clinical history and physical examination, so that the laboratory findings can be interpreted in the proper clinical context. Since under some circumstances entrapment neuropathies such as carpal tunnel syndrome (CTS) and ulnar neuropathy may mimic cervical radiculopathy, the consultation should include a screening evaluation of these neuropathies. If EDX findings consistent with cervical radiculopathy are found, the EDX consultant should attempt to identify the specific nerve root affected and to assess the severity and chronicity of involvement.The following recommendations relate to EDX studies when laboratory confirmation of cervical radiculopathy is desired. The practice parameters are based on the scientific literature supporting the use of needle EMG in the evaluation of cervical radiculopathy and NCSs in the evaluation of entrapment neuropathies of the upper extremities.1,2The strength of a recommendation is based on the quality and consistency of supporting evidence as well as the magnitude of harms, benefits, and costs. Each recommendation is classified as a Guideline or Option according to the definitions provided above.
- Guideline: Needle EMG examination of at least 1 muscle innervated by the C5, C6, C7, C8, and T1 spinal roots in a symptomatic limb, performed and interpreted by a specially trained physician. Cervical paraspinal muscles at 1 or more levels, as appropriate to the clinical presentation, should be examined (except in patients with prior cervical laminectomy using a posterior approach). If a specific root is suspected clinically, or if an abnormality is seen on the initial needle EMG examination, additional studies as follows:
- Examination of 1 or 2 additional muscles innervated by the suspected root and a different peripheral nerve.
- Demonstration of normal muscles above and below the involved root.
- Guideline: At least 1 motor and 1 sensory NCS should be performed in the clinically involved limb to determine if concomitant polyneuropathy or nerve entrapment exists. Motor and sensory NCSs of the median and ulnar nerves should be performed if symptoms and signs suggest CTS or ulnar neuropathy.1,2 If 1 or more NCSs are abnormal, or if clinical features suggesting polyneuropathy are present, further evaluation may include NCSs of other nerves in the ipsilateral and contralateral limbs to define the cause of the abnormalities.
- Option: If needle EMG examination is abnormal, needle EMG of 1 or more contralateral muscles may be necessary to exclude bilateral radiculopathy, or to differentiate between radiculopathy and polyneuropathy, motor neuron disease, spinal cord lesions, or other neuromuscular disorders.
- Option: Perform median and/or ulnar F-wave studies in suspected C8 or T1 radiculopathy. Compare with the contralateral side if necessary.
- Option: Perform cervical nerve root stimulation to help in identifying radiculopathy.
- Option: Perform H-reflex study of the flexor carpi radialis to assist in identifying pathology of the C6 and C7 nerve roots.
RECOMMENDATIONS FOR FUTURE RESEARCH
It is recommended that:
- Future research of EDX studies should be designed to:
- Define specific clinical criteria used for patient selection.
- Provide an adequate description of the population studied, including the timing of the study in relation to symptom onset.
- Meet all 6 literature classification criteria described in this report.
- Correlate EDX results with clinical and radiological findings at each spinal root level.
- Outcome studies of the harms, benefits, and costs of EDX testing in patients suspected of having cervical radiculopathy be initiated.
- Studies to compare EDX examination with alternative tests proposed for the evaluation of cervical radiculopathy be designed.
- The AAEM review or update this report every 5 years or as necessary.
This report is provided as an educational service of the AAEM. It is based on an assessment of the current scientific and clinical information. It is not intended to include all possible methods of care of a particular clinical problem, or all legitimate criteria for choosing to use a specific procedure. Neither is it intended to exclude any reasonable alternative methodologies. The AAEM recognizes that specific patient care decisions are the prerogative of the patient and his/her physician and are based on all of the circumstances involved.
American Association of Electrodiagnostic Medicine
American Academy of Physical Medicine and Rehabilitation
ABSTRACT
The usefulness of the needle electromyography (EMG) examination in managing patients with suspected cervical radiculopathy was evaluated by a critical review of the scientific literature. Forty-six articles were identified and reviewed. Twenty-two of these articles provided the basis for addressing the diagnostic value of needle EMG examination. In the studies reviewed, the needle EMG examination provided confirmatory evidence of a cervical root pathology in 30% to 72% of patients presenting with symptoms or signs of cervical radiculopathy. The lack of a gold standard for the diagnosis of cervical radiculopathy likely introduced a bias towards underestimation of the sensitivity of needle EMG. In studies based on patients with neurological or radiological signs, the American Association of Electrodiagnostic Medicine (AAEM) Quality Assurance (QA) Committee estimated a sensitivity of 50% to 71%. Needle EMG abnormalities were highly correlated with motor weakness. Good agreement between imaging studies and needle EMG findings was possible in 65% to 85% of the cases. The AAEM QA committee concluded that the needle EMG examination confirms the diagnosis of cervical radiculopathy with a moderate degree of sensitivity and a high degree of specificity.
Developed by the following members of the American Association Electrodiagnostic Medicine (AAEM) Quality Assurance Committee: Primary Author: Yuen T. So, MD, PhD; Chair: Cheryl F. Weber, MD; Members: Richard D. Ball, MD, PhD; William W. Campbell, MD, MSHA.
The AAEM would also like to acknowledge the help of the following: Murray E. Brandstater, MBBS, PhD, FRCP(C); Neil A. Busis, MD; Dorothy J. Carroll, MD, FRCP (C); Sudhansu Chokroverty, MD, FRCP; Faye Y. Chiou-Tan, MD; Janice L. Cockrell, MD; Leslie J. Dorfman, MD; Daniel Dumitru, MD, PhD; Donna Frankel, MD; Erick A. Grana, MD; Michael K. Greenberg, MD; Ludwig Gutmann, MD; Earl R. Hackett, MD; Robert L. Harmon, MD, MS; Charles K. Jablecki, MD; M. David Jackson, MD; David A. Krendel, MD; Tim Lachman, MD; Francis P. Lagattuta, MD; Trilok N. Monga, MD; Kevin R. Nelson, MD; Richard K. Olney, MD; Atul T. Patel, MD; Lawrence H. Phillips II, MD; Rhonda M. Pridgeon, MD; Caroline A. Quartly, MD, FRCP(C); Donald B. Sanders, MD; Kathryn A. StolpSmith, MD, MS; Robert L. Sufit, MD; Jacqueline J. Wertsch, MD; Asa J. Wilbourn, MD; John R. Wilson, MD; and Claire V. Wolfe, MD.
Key words: cervical radiculopathy• electrodiagnosis • EMG • electromyography• spinal root compression • spondylosis • neuromuscular disease
JUSTIFICATION
The Quality Assurance (QA) Committee of the American Association of Electrodiagnostic Medicine (AAEM) was charged by the AAEM Board of Directors to conduct a critical review of the literature on the usefulness of electrodiagnostic studies in the clinical evaluation of patients with suspected cervical radiculopathy. This literature review is an educational effort by the AAEM. The focus is limited to the evaluation of the needle electromyography (EMG) examination. The following report is the result of a systematic review of the scientific literature on needle EMG, especially in regard to its usefulness in the confirmation of a diagnosis of cervical radiculopathy and localization of the level of root involvement.
OVERVIEW
Cervical radiculopathy is a substantial cause of disability and morbidity, and its cost-effective evaluation and treatment are crucial. Using diagnostic criteria based on a combination of clinical symptoms, physical signs, and radiological, electrodiagnostic, and surgical findings, a recent epidemiological study reported the average annual age-adjusted incidence rate of cervical radiculopathy to be 83.2 per 100,000.44This is slightly less frequent than carpal tunnel syndrome (CTS) and about half that of stroke. The age-specific annual incidence rate per 100,000 population reached a peak of 202.9 for the age group 50 to 54 years. There was recurrence of the condition in 31.7% of those with the diagnosis and 26% underwent surgery for cervical radiculopathy.
Characteristically, patients with cervical radiculopathy complain of pain in the neck and in a radicular distribution in the upper extremity. Pain is often accompanied by numbness, tingling, and weakness. The symptoms are usually unilateral but may also be bilateral. Neurologic examination may demonstrate abnormal sensory perception, weakness, and reduced tendon stretch reflexes in the distribution of the affected spinal nerve root.
A number of disorders must be distinguished from cervical radiculopathy. Referred pain may arise from several structures in the cervical spine including the facet joint, intervertebral disc, periosteum, ligaments, and fascia. Some conditions, such as subacromial bursitis, bicipital tendinitis, rotator cuff tendinitis or tear, and myofascial pain syndromes, may mimic the pain of cervical radiculopathy. Various neurologic disorders, such as idiopathic brachial plexitis, radiation or neoplastic plexopathy, entrapment neuropathy, intramedullary spinal cord lesion, motor neuron disease, and multifocal motor neuropathy, may also cause sensory or motor disturbances that are at times difficult to distinguish from cervical radiculopathy.
The most common cause of cervical radiculopathy is degenerative disease of the spine and intervertebral discs. Cervical radiculopathy may also result from spinal root avulsion, diabetes mellitus, bacterial abscess, herpes zoster infection, Lyme disease, neurosyphilis, tumor invasion of the leptomeninges, and various inflammatory polyradiculoneuropathies. Recognition of these less common causes is important because of the treatment implications. Careful clinical evaluation, aided by appropriate electrodiagnostic and other ancillary tests, often provides the only clues to the localization and identification of the pathology.
There is considerable variation in the use of EDX tests for the diagnosis and management of spondylotic or discogenic cervical radiculopathy. Some clinicians believe that decision-making about decompressive surgery and other treatments may be based entirely on clinical evaluation and imaging studies. Others believe that the advances in imaging techniques have not obviated the need for EDX assessment, but rather increased it. Asymptomatic radiological abnormalities are commonly revealed by magnetic resonance imaging (MRI),53 as well as myelography and computed tomography (CT) of the cervical spine.15 Findings on imaging studies may not correlate with physiological function. The false positive rate of imaging studies generally increases with advancing age and ranges from 20% to over 50%. For these reasons, it has been argued that EDX testing plays an important complementary role to the clinical examination in the evaluation of patients with cervical radiculopathy.57
EDX examination of paraspinal and limb muscles has been utilized for over 50 years,7,49 and cervical radiculopathy is among the most common referral diagnoses to the EDX laboratory. Although some evidence of denervation may be seen on surface EMG recordings,7 needle EMG is widely regarded as the technique of choice in the diagnostic evaluation of cervical radiculopathy.21,31,57 Needle EMG findings may include signs of denervation such as fibrillation potentials and reduced recruitment of motor unit potentials (MUPs), or signs of reinnervation such as an increased proportion of polyphasic, prolonged duration or increased amplitude MUPs. The pattern of denervation or reinnervation helps to establish the presence of radiculopathy, the level of spinal root involvement, and the severity and chronicity of the disease.
A variety of alternative electrophysiological techniques have also been investigated for use in the diagnosis of
cervical radiculopathy.5,10,22-25,28,30,35,42,43,46-48,54,55,58,59 There are circumstances that justify their use. Review of these procedures is beyond the scope of this report.
METHOD OF REVIEW
A Medline search for articles on clinical studies of cervical radiculopathy published in the English language between 1971 and 1998 identified over 1000 articles. Additional articles were identified from the bibliographies of relevant reviews and articles. Eighty-five articles were found that reported on the EDX findings in patients with spondylotic cervical radiculopathy. After excluding articles dedicated solely to literature review and expert opinions, 46 articles that described original EDX findings in patients with cervical radiculopathy were identified.5-7,10-17,20,22-30,32-43,45-52,54-56,58,59 All 46 articles were then reviewed in their entirety, with special attention to the study design, selection and number of patients, electrodiagnostic methods and, if available, the sensitivity and specificity of the technique. The scientific merits of each article were analyzed using 6 literature classification criteria adopted by the AAEM QA Committee.
LITERATURE CLASSIFICATION CRITERIA
- Prospective study design. A prospective study design permits uniform collection and analysis of data.
- Diagnosis of cervical radiculopathy independent of EDX findings. The diagnosis of cervical radiculopathy independent of EDX findings permits the identification of a patient population suitable for the evaluation of sensitivity and specificity of the EDX procedure.
- Exclusion of other upper extremity pathology that could confound EDX results. Conditions such as CTS and brachial plexopathy may mimic the sensory and motor disturbances of cervical radiculopathy.
- Sufficient description of the EDX procedure. A detailed description of the procedure or a reference to established techniques in the literature is necessary for validation of the study methodology and permits duplication of the procedure for subsequent use in the EDX laboratory.
- Clearly stated criteria for electrodiagnosis of cervical radiculopathy. The findings of conventional needle EMG examination cannot be easily analyzed in a quantitative and statistical manner. Clearly stated criteria for electrodiagnosis permits validation of methodology by comparison to widely accepted guidelines for needle EMG interpretation.
- Results presented in sufficient detail to permit determination of the sensitivity and/or specificity of the EDX procedure.
RESULTS
Of the 46 articles, 23 were excluded because they reported primarily anecdotal experience, included fewer than 10 patients, or provided insufficient information about the needle EMG findings.6,7,10,11,15,16,23-25,28,32,33,37,40,42,43,45-48,51,54,59 One article was excluded because the combined data for lumbosacral and cervical radiculopathy could not be analyzed separately.23 The remaining 22 articles form the basis for addressing the usefulness of needle EMG in the evaluation of cervical radiculopathy. Table 1 lists those articles which met 3 or more criteria.
This report focuses on 2 issues concerning the use of needle EMG: the sensitivity of needle EMG in confirming a diagnosis of cervical radiculopathy and the accuracy of needle EMG in localizing the level of spinal root lesion.
| Table 1. Literature Classification of Electrodiagnostic Studies.* |
| 6 of 6 Criteria Met Tackmann and Radu52 5 of 6 Criteria Met Berger and colleagues5 So and colleagues50 Partanen and colleagues41 Leblhuber and colleagues35 4 of 6 Criteria Met Tsai and colleagues55 Yiannikas and colleagues58 Hong and colleagues27 Katirji and colleagues29 3 of 6 Criteria Met Khan and colleagues30 Waylonis56 Negrin and colleagues39 Shea and colleagues49 Date and Gray17 Lauder and Dillingham34 |
| *Only studies which met 3 or more criteria are listed |
Sensitivity of needle EMG. The true sensitivity of a technique can be assessed only when it is compared to an independent reference standard. A gold standard unfortunately does not exist for the diagnosis of cervical radiculopathy, as clinical, radiological, or electrophysiological diagnosis all have inherent limitations. In the AAEM QA Committee’s estimation of sensitivity, 10 studies that selected patients on the basis of the electrodiagnostic findings were excluded.13,14,17,20,26,29,34,36,39,49In the remaining studies, patient selection was based on some combination of clinical or radiological findings, although none of the articles specified the inclusion criteria in detail. Of the remaining 12 articles, 2 that met only 2 of 6 literature classification criteria were also excluded.12,38 Thus, 10 articles provided the basis of the assessment of sensitivity of needle EMG (Table 2).
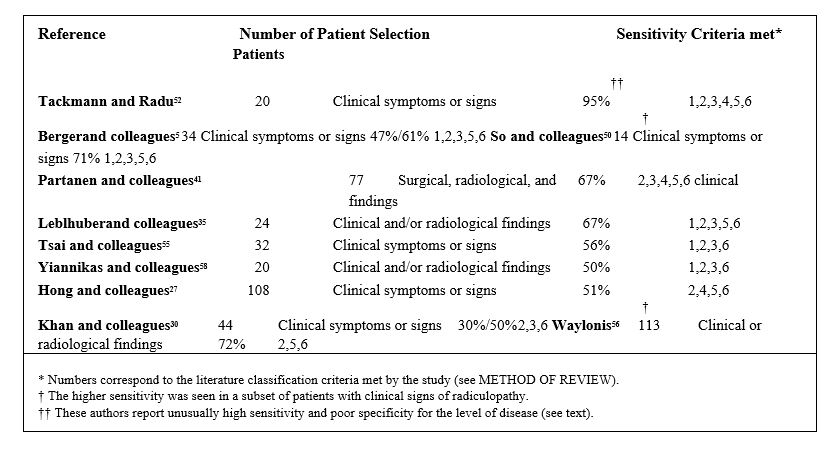
Although only 1 article met all 6 of the classification criteria,52 the findings from all 10 articles were of sufficient quality to permit an estimation of diagnostic sensitivity. Neglecting to document the needle EMG procedure in detail (Criterion 4) was the most common reason behind a failed criterion.5,30,35,50,55,56,58These articles typically mention the performance of needle EMG using conventional techniques, but did not specify the procedure, the muscles, or the myotomes studied. The omission is likely due to the widespread use and standardization of needle EMG technique over the years. These omissions hampered ndependent validation of the investigators’techniques, even though the studies may be otherwise satisfactory. Similarly, some articles did not provide an indication that confounding neuropathy or plexopathy was adequately excluded Criterion 3)27,56and others did not specifically state their criteria for identifying needle EMG abnormalities (Criterion 5).30,55,58
In a prospective study of 34 patients with cervical radiculopathy, Berger and colleagues compared the diagnostic utility of cervical root stimulation to that of needle EMG examination.5 Although the study focused primarily on spinal root stimulation, the needle EMG results were described adequately. Sixteen (47%) of their patients had needle EMG abnormalities supportive of the diagnosis of cervical radiculopathy. The yield was higher (61%) in a subset of 18 patients with clinical signs of radiculopathy. In another study comparing needle EMG with cervical root stimulation, 18 of 32 (56%) patients had abnormal needle EMG findings.55 In a small selected group of patients with clinical signs of cervical radiculopathy, needle EMG revealed denervation in affected myotomes in 71% and was superior to thermography in providing diagnostic information.50 Two prospective studies35,58 and 1 other study30 compared needle EMG to somatosensory evoked potentials (SEPs), and reported needle EMG abnormalities in 30% to 67% of patients with cervical radiculopathy.
Three large retrospective studies, reporting on a total of 298 patients, were devoted primarily to the conventional needle EMG examination.27,41,56 Despite their retrospective design, the patient selection in these investigations appeared to be independent of electrodiagnosis. The reported rates of needle EMG abnormality are similar to those reported by smaller prospective studies, ranging from 51% to 72%. A total of 189 of the 298 patients (63%) had evidence of denervation on needle EMG.
In a study which met all 6 criteria, Tackmann and Radu52 evaluated 20 patients with clinical evidence of radiculopathy and noted needle EMG evidence of acute or chronic denervation in 19 patients. The authors reported that the needle EMG findings frequently did not correlate with the clinical level of root involvement. The majority of their patients had C6 or C7 radiculopathy, yet the abductor pollicis brevis and abductor digiti quinti were frequently abnormal upon needle EMG examination. Patient selection bias or difference in testing and interpretation may account for the unusually high sensitivity and low specificity, although the precise reasons could not be determined from the article.
Accuracy of Needle EMG in Localizing Involved Root Levels.Hong and colleagues27 retrospectively analyzed 680 root levels in 80 patients with unilateral radiculopathy and 28 patients with bilateral radiculopathy. They observed that the presence of needle EMG abnormalities correlated in particular with motor weakness. Needle EMG was abnormal in 32 (97%) of 33 cervical root levels with motor weakness, in contrast to 79 (29%) of 275 levels with sensory abnormalities. Furthermore, only 6 (1.5%) of 404 levels with no clinical findings had needle EMG abnormalities. When compared to the finding of foraminal or disc space narrowing on plain adiographic examination, needle EMG abnormalities correlated better with the level of clinical involvement.
Katirji and colleagues29 correlated needle EMG findings with metrizamide myelography and CT in 20 patients with needle EMG diagnosis of single-level radiculopathy. The correlation was best at the C6 and C7 levels (73.3%), and the overall correlation was 65% for the C5 to C8 levels. Similar correlation was reported in other studies. General agreement between needle EMG and myelography was reported in 20 (77%) of 23 cases by Negrin and colleagues39 and in 44 (85%) of 52 patients with abnormal needle EMG studied by Partanen and colleagues.41 No studies on the correlation of needle EMG results with MRI studies were identified.
Levin and colleagues36 reviewed the preoperative needle EMG findings in 50 cases of solitary root lesions confirmed at surgery. Stereotypic patterns of denervation were seen in C5, C7, and C8 radiculopathies, whereas the pattern in C6 radiculopathy resembled that of either C5 or C7 radiculopathy. Thus, the pattern of needle EMG findings is, in general, highly specific for the level of spinal root involvement. An abnormal needle EMG should permit localization of lesion to an accuracy of 1 or 2 levels. This concept is supported by other studies correlating needle EMG findings with surgical observations. Partenen and colleagues41 reported that needle EMG provided correct localization in 50 (76%) of 66 operated cases. A very high level of concordance with surgical findings was reported in 2 early studies. Needle EMG findings correlated correctly with the surgical level in 13 of 14 cases reported by Shea and colleagues49 and in 62 of 69 cases of Crane and Krusen,12 although it is likely that the needle EMG findings may have influenced the root level for surgical exploration.
As noted earlier, Tackmann and Radu52 found frequent needle EMG abnormalities in clinically uninvolved myotomes. Their experience is contrary to that of others. Again, their unusually high sensitivity of 95% suggests a difference in either patient population or needle EMG technique.
DISCUSSION
The sensitivity of the needle EMG examination can be determined accurately only if a gold standard were available for comparison. In the AAEM QA Committee’s estimation of sensitivity, patient selection in the studies that were reviewed was based on clinical symptoms, signs, or radiological findings. None of these indicators, in isolation or when combined, come close to a gold standard for the diagnosis of cervical radiculopathy. Furthermore, none of the articles specify the inclusion criteria in detail. Despite these reservations, the literature review provides evidence that needle EMG examination of the cervical myotomes has a moderate diagnostic sensitivity in the diagnosis of radiculopathy.
The selected studies report a wide range of needle EMG abnormality rate from 30% to 72%, likely reflecting differences in selection criteria and patient populations. The prevalence of needle EMG abnormalities rises with the presence of motor deficits or other neurologic signs.5,27,30,41,58 The abnormality rate is 50% to 71% in patients with clinical signs or radiological findings (Table 2). The higher range probably represents a more accurate estimate of the true sensitivity of the needle EMG examination. The lack of a gold standard, if anything, is likely to introduce a bias towards an underestimation of the sensitivity, as some patients included in the studies may not have true cervical radiculopathy.
None of the reviewed articles report needle EMG findings of normal subjects. Published studies of needle EMG findings in normal subjects8,9 and subsequent extensive clinical experience have shown that a properly performed and interpreted needle EMG examination is rarely abnormal in normal subjects. This implies a very high specificity for needle EMG. Several observations in patients with cervical radiculopathy also support the high specificity of needle EMG. Needle EMG examination of 404 clinically normal myotomes revealed abnormality in only 1.5%.27 In 50 patients selected for single level radiculopathy, the level of needle EMG abnormality had excellent localizing value.36Thus, the presence of needle EMG abnormalities provide specific information regarding denervation and reinnervation. This degree of specificity is only possible if the procedure is performed by a specially trained physician and presently accepted standards are followed.3,4,18,19,31
Needle EMG abnormalities correlate less well with radiological findings, as would be expected from the well known occurrence of radiological lesions in asymptomatic patients and the overlapping innervation of myotomes. Agreement on the level of root lesion was found between needle EMG and myelography or CT in 65% to 85% of the cases.29,39,41 A similar degree of correlation is reported when needle EMG is compared with surgical findings.36
Although this literature review focuses on needle EMG, nerve conduction studies (NCSs) with the use of F wave, H reflex, or root stimulation may be applied to the diagnosis of cervical radiculopathy under selected circum-
stances.5,23,28,35,42,46,47,54,55 More importantly, a well documented use of NCSs is in the screening of concomitant peripheral nerve pathology.1,2CTS, ulnar neuropathy, thoracic outlet syndrome, brachial plexopathy, or peripheral neuropathy mimics the pain, paresthesias, and weakness of cervical radiculopathy. These disorders are important considerations in the EDX evaluation of patients with a suspected cervical radiculopathy. A minimal evaluation therefore should include motor and sensory NCSs of the involved limb in addition to needle EMG examination.
CONCLUSIONS
This review provides evidence from the medical literature that a properly performed and interpreted needle EMG examination confirms a clinical diagnosis of cervical radiculopathy with a moderate degree of sensitivity and a high degree of specificity.
INTERFACE WITH AANEM GUIDELINES
This literature review cites published studies that support the recommendations in the AAEM Guidelines in Electrodiagnostic Medicine, see Chapter 4, The Electrodiagnostic Medicine Consultation3 for patients undergoing EDX evaluation for symptoms of cervical radiculopathy.
SUMMARY OF HARMS, BENEFITS, AND COSTS FOR INTERVENTIONS CONSIDERED
The risks of EDX testing to the patient include transient discomfort, bruise, hematoma, and infection from the needle insertion required to perform needle EMG. The risk of needle EMG to the EDX consultant includes inadvertent self-puncture by the needle used to evaluate the patient and subsequent infection by hepatitis, human immunodeficiency virus (HIV), or other communicable disease.1,3 This study has not undertaken a systemic assessment of the harms, benefits, and costs of EDX testing. Such an evaluation would require an outcome study.
RECOMMENDATIONS FOR FUTURE RESEARCH
Future investigations of EDX testing in cervical radiculopathy should take into account the following recommendations:
- All 6 literature classification criteria described in this report should be met.
- The study should define specific clinical criteria used for patient selection.
- There should be an adequate description of the population studied, including the severity of cervical radiculopathy and the study timing in relation to symptom onset.
- EDX procedures should be described in sufficient detail, including specification of the muscles to be examined and clearly stated criteria for abnormality.
- Electrodiagnostic, clinical, and radiological findings should be analyzed and correlated at each spinal root level.
- Outcome studies of the harms, benefits, and costs of EDX testing in patients suspected of having cervical radiculopathy are needed.
ETHICAL AND LEGAL CONSIDERATIONS
In view of the existing evidence on the sensitivity and specificity of EDX testing to confirm the diagnosis of cervical radiculopathy, the AAEM recommends that health care providers and insurers should accept needle EMG examinations, performed as described in this review, as valid and reproducible techniques for the evaluation of patients suspected of cervical radiculopathy.
DISCLAIMER
This report is provided as an educational service of the AAEM. It is based on an assessment of the current scientific and clinical information. It is not intended to include all possible methods of care of a particular clinical problem, or all legitimate criteria for choosing to use a specific procedure. Neither is it intended to exclude any reasonable alternative methodologies. The AAEM recognizes that specific patient care decisions are the prerogative of the patient and his/her physician and are based on all of the circumstances involved.
References
- American Association of Electrodiagnostic Medicine: Literature review of the usefulness of nerve conduction studies and electromyography in the evaluation of patients with ulnar neuropathy at the elbow. Muscle Nerve 1999; 22 (suppl 8) S175-S205; Background Reference.
- American Association of Electrodiagnostic Medicine: Practice parameter for electrodiagnostic studies in carpal tunnel syndrome. Muscle Nerve 1993; 16:1390-1414.
- American Association of Electrodiagnostic Medicine: Guidelines in Electrodiagnostic Medicine. Muscle Nerve 1999; 22 (suppl 8); Background Reference.
- Aminoff MJ. Electromyography in clinical practice. New York, Churchill Livingstone, 1987. Background Reference.
- Berger AR, Busis NA, Logigian EL, Wierzbicka M, Shahani BT: Cervical root stimulation in the diagnosis of radiculopathy. Neurology 1987; 37:329-332. Criteria Met (5/6: 1,2,3,5,6) Patients with cervical radiculopathy were clinically defined. In the authors' hands, cervical root stimulation was more sensitive than needle EMG examination. Root stimulation was abnormal in 27 of 34 patients, whereas needle EMG was abnormal in 16. See text.
- Boot DA, Khan RH, Sellar RJ, Hughes SP, Kirkpatrick AE: Computed tomogram myelography in cervical spondylosis. Int Orthop 1987; 11:249-254. Criteria Met (1/6: 6) Only 9 patients.
- Brazier MAB, Watkins AL, Michelson JJ: Electromyography in differential diagnosis of ruptured cervical disc. Arch Neurol Psychiat 1946; 56: 651-658. Criteria Met (3/6: 4,5,6) Employed only surface EMG recording.
- Buchthal F, Guld C, Rosenfalck P: Action potential parameters in normal human muscle and their dependence on physical variables. Acta Physiol Scand1954; 32:200-229. Background Reference.
- Buchthal F, Rosenfalck P: Spontaneous electrical activity of human muscle. Electroencephalogr Clin Neurophyiol 1966; 20:321-336. Background Reference.
- Chistyakov AV, Soustiel JF, Hafner H, Feinsod M: Motor and somatosensory conduction in cervical myelopathy and radiculopathy. Spine 1995; 20:2135-2140. Criteria Met (3/6: 1,2,4) A study devoted solely to motor-evoked potentials and somatosensory-evoked potentials.
- Colachis SC, Pease WS, Johnson EW: Polyphasic motor unit action potentials in early radiculopathy: their presence and ephaptic transmission as an hypothesis. Electromyogr Clin Neurophysiol 1992; 32:27-33. Criteria Met (1/6: 6) Case reports.
- Crane CR, Krusen EM: Significance of polyphasic potentials in diagnosis of cervical root involvement. Arch Phys Med Rehab1968;49:403-406. Criteria Met (2/6: 4,6) Retrospective study that included 241 patients with referral diagnosis of cervical radiculopathy. Although not specifically stated, needle EMG was probably considered abnormal if any polyphasic potentials were present. Eighty-one of 87 patients with abnormal myelogram had abnormal needle EMG. Needle EMG findings correlated correctly with the affected level at surgery in 62 (90%) of 69 cases.
- Czyrny JJ, Lawrence J: The importance of paraspinal muscle EMG in cervical and lumbrosacral radiculopathy: review of 100 cases. Electromyogr Clin Neurophysiol 1996; 36:503-508. Criteria Met (2/6: 4,5) In the authors’ hands, 20 out of 49 patients with cervical radiculopathies had EMG abnormalities restricted only to the paraspinal muscles.
- Czyrny JJ, Lawrence J: Importance of paraspinal muscle EMG in cervical and lumbrosacral radiculopathies. Amer J Phys Med Rehab1995; 74:458-459. Same study as 13.
- Daniels DL, Grogan JP, Johansen JG, Meyer GA, Williams AL, Haughton VM: Cervical radiculopathy: computed tomography and myelography compared. Radiology1984; 151:109-113. Background Reference. Radiologic study. Little mention of EMG.
- Danner R: Referral diagnosis versus electroneurophysiological finding. Two years electroneuromyographic consultation in a rehabilitation clinic. Electromyogr Clin Neurophysiol 1990; 30:153-157. Criteria Met (0/6) (Study not designed to specifically address cervical radiculopathy).
- Date ES, Gray LA: Electrodiagnostic evidence for cervical radiculopathy and suprascapular neuropathy in shoulder pain. Electromyogr Clin Neurophysiol 1996; 36:333-339. Criteria Met (3/6: 1,4,5) Eleven of 33 patients diagnosed with a shoulder impingement syndrome had electrodiagnostic evidence suggestive of cervical radiculopathy.
- Daube JR: AAEM Minimonograph #11: needle examination in clinical electromyography. Muscle Nerve 1991; 14:685-700. Background Reference.
- Daube JR: Assessing the motor unit with needle electromyography, in J. R. Daube (eds): Clinical Neurophysiology. Philadelphia, F. A. Davis, 1996; 257-281. Background Reference.
- Dillingham TR, Pezzin LE, Lauder TD: Cervical paraspinal muscle abnormalities and symptom duration: a multivariate analysis. Muscle Nerve 1998, 21:640-642. Criteria Met (2/6: 4,5) Attempt to correlate spontaneous activity in cervical paraspinal muscles with symptom duration in patients with electrodiagnostic evidence of cervical radiculopathy.
- Eisen A: Electrodiagnosis of radiculopathies, in A. J. Aminoff (eds): Neurologic Clinics: Symposium on Electrodiagnosis. Philadelphia, W. B. Saunders, 1985, vol 3, pp. 495-510. Background Reference.
- Eisen A, Hoirch M, Moll A: Evaluation of radiculopathies by segmental stimulation and somatosensory evoked potentials. Can J Neurol Sci1983; 10:178-182. Criteria Met (2/6: 1{?},2) Thirty-six patients with either lumbosacral or cervical radiculopathies were included. Needle EMG had higher diagnostic yield (75%) than F waves and SEPs, and correlated better with motor deficits. See text.
- Eisen A, Schomer D, Melmed C: The application of F-wave measurements in the differentiation of proximal and distal upper limb entrapments. Neurology1977; 27:662-668. Criteria Met (3/6: 1,2,3) F-wave studies were abnormal in 67% of 23 patients with proximal entrapment neuropathy (including some patients with presumed cervical radiculopathy).
- Heiskari M, Siivola J, Heikkinen ER: Somatosensory evoked potentials in evaluation of decompressive surgery of cervical spondylosis and herniated disc. Ann Clin Res 1986; 18:107113. Criteria Met (2/6: 1,2) This study was devoted solely to SEP.
- Heiskari M, Tolonen U, Nystrom SHM: Comparison of somatosensory evoked responses from root and cord recorded by skin and epidural electrodes using stimulation of the median nerve in cervical radiculopathy and radiculomyelopathy. Acta Neurochirurgica 1986; 79:114-119. Criteria Met (2/6: 1,2) This study was devoted solely to SEP.
- Honet JC, Puri K: Cervical radiculitis: treatment and results in 82 patients. Arch Phys Med Rehab1976; 57:12-16. Criteria Met (2/6: 5,6) This study discussed primarily treatment results.
- Hong CZ, Lee S, Lum P: Cervical radiculopathy. Clinical, radiographic and EMG findings. Orthop Rev 1986; 15: 433439. Criteria Met (4/6: 2,4,5,6) This retrospective study reviewed the clinical, plain radiographic and needle EMG findings in 108 patients with cervical radiculopathy. See text.
- Jaskolski DJ, Jarratt JA, Jakubowski J: Clinical evaluation of magnetic stimulation in cervical spondylosis. Br J Neurosurg 1989; 3: 541-548. This is a study of only magnetic stimulation.
- Katirji MB, Agrawal R, Kantra TA: The human cervical myotomes: an anatomical correlation between electromyography and CT/myelography. Muscle Nerve 1988; 11: 1070-1073. Criteria Met (4/6: 3,4,5,6) The radiographic findings (metrizamide myelography/computed tomography) were correlated with needle EMG findings in 20 patients. See text.
- Khan MRH, McInnes A, Hughes SPF: Electrophysiological studies in cervical spondylosis. J Spinal Dis1989; 2:163-169. Criteria Met (3/6: 2,3,6) Forty-four of 57 patients had needle EMG examination. An abnormality rate of 50% was seen in those patients with clinical signs, as compared to 30% in those without neurologic signs. Abnormality was seen slightly less frequently in SEP and F-wave studies. See text.
- Kimura J: Electrodiagnosis in diseases of nerve and muscle. Philadelphia, F. A. Davis, 1989. Background Reference.
- Lane ME: Recent developments in the electrodiagnosis of radiculopathies. Bull Hosp Joint Dis Orthop Inst 1984; 44: 5664.
- Lane ME, Tamhankar MN, Demopoulos JT: Discogenic radiculopathy. Use of electromyography in multidisciplinary management. NY State J Med1978; 78:32-36.
- Lauder TD, Dillingham TR: The cervical radiculopathy screen: optimizing the number of muscles studied. Muscle Nerve 1996; 19:662-665. Criteria Met (3/6: 3,4,5) A retrospective study of patients with electrodiagnostically confirmed radiculopathy.
- Leblhuber F, Reisecker R, Boehm-Jurkovic H, Witzmann A, Deisenhammer E: Diagnostic value of different electrophysiologic tests in cervical disk prolapse. Neurology1988; 38:1879-1881. Criteria Met (5/6: 1,2,3,5,6) All 24 patients had radiologically verified cervical disk prolapse. Needle EMG was abnormal in 65%, dermatomal SEP in 85%, and F wave 38%. See text.
- Levin KH, Maggiano HJ, Wilbourn AJ: Cervical radiculopathies: comparison of surgical and EMG localization of single root lesions. Neurology1996; 46:1022-1025. Criteria Met (2/6: 5,6) The authors identified a highly selected group of 50 patients with surgically defined solitary root compression. Needle EMG was classified as abnormal only by the presence of fibrillation potentials. A relatively stereotyped pattern of abnormalities was seen with C5, C7 and C8 radiculopathies. See text.
- Makin GJ, Brown W F, Ebers GC: C7 radiculopathy: importance of scapular winging in clinical diagnosis. J Neurol Neurosurg Psychiat 1986; 49:640-644. Case reports.
- Marinacci AA: A correlation between the operative findings in cervical herniated discs with the electromyograms and opaque myelograms. Electromyography 1966; 6:5-20. Criteria Met: (2/6: 2,6) There was only a brief mention of needle EMG findings.
- Negrin P, Lelli S, Fardin P: Contribution of electromyography to the diagnosis, treatment and prognosis of cervical disc disease: a study of 114 patients. Electromyogr Clin Neurophysiol 1991; 31:173-179. Criteria Met (3/6: 3,5,6) The study included 114 patients with cervical radiculopathy and denervation on needle EMG examination. See text.
- Newman M, Nelson N: Digital nerve sensory potentials in lesions of cervical roots and brachial plexus. Can J Neurol Sci 1983; 10:252-255. Criteria Met (2/6: 1,2) This is a study of sensory nerve conduction and F-wave studies in patients with cervical root and plexus lesions.
- Partanen J, Partanen K, Oikarinen H, Niemitukia L, Hernesniemi J: Preoperative electroneuromyography and myelography in cervical root compression. Electromyogr Clin Neurophysiol 1991;31: 21-26. Criteria Met (5/6: 2,3,4,5,6) Seventy-seven patients with preoperative needle EMG and myelography were selected. Abnormal findings were seen in 67%, with localizing findings seen in 57%. See text.
- Peioglou-Harmoussi S, Fawcett PR, Howel S, Barwick DD: F response frequency in motor neuron disease and cervical spondylosis. J Neurol Neurosurg Psychiat 1987; 50:593-599. Criteria Met (2/6: 1,2) The authors found no significant difference in the frequency of ulnar F-wave response between patients with cervical spondylosis and controls.
- Perlik SJ, Fisher MA: Somatosensory evoked response evaluation of cervical spondylytic myelopathy. Muscle Nerve 1987; 10:481-489. Criteria Met (3/6: 1,2,5) Thirteen patients with cervical myelopathy were studied with tibial and median SEP. Eight patients had superimposed cervical radiculopathy and needle EMG abnormalities. Tibial SEPwas abnormal in all 13 patients. Median SEPwas abnormal in those with cord lesions at C5-6 or above.
- Radhakrishnan K, Litchy WJ, O'Fallon WM, Kurland LT: Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain 1994; 117:325-335. Background Reference.
- Raps SP, Rubin M: Proximal median neuropathy and cervical radiculopathy: double crush revisited. Electromyogr Clin Neurophysiol 1994; 34:195-196. Case reports only.
- Sabbahi MA, Khalil M: Segmental H-reflex studies in upper and lower limbs of patients with radiculopathy. Arch Phys Med Rehab1990; 71:223-227. Criteria Met (3/6: 1,3,5) (H reflex only).
- Schimsheimer RJ, Ongerboer de Visser BW, Kemp B: The flexor carpi radialis H reflex in lesions of the sixth and seventh cervical nerve roots. J Neurol Neurosurg Psychiat 1985; 48: 445-449. Criteria Met (1/6: 2) Extensive normal data on the H reflex of the flexor carpi radialis were presented. The H-reflex latency was abnormal only in lesions of the C6 or C7 roots.
- Schmid UD, Hess CW, Ludin HP: Somatosensory evoked potentials following nerve and segmental stimulation do not confirm cervical radiculopathy with sensory deficit. J Neurol Neurosurg Psychiat 1988; 51:182-187. Criteria Met (2/6: 1,2) This was devoted solely to SEP.
- Shea PA, Woods WW, Werden DH: Electromyography in diagnosis of nerve root compression syndrome. Arch Neurol Psychiat 1950; 64:93-104. Criteria Met (3/6: 4,5,6) One of the earliest investigations of needle EMG evaluation of patients with cervical radiculopathy. See text.
- So YT, Olney RK, Aminoff MJ: A comparison of thermography and electromyography in the diagnosis of cervical radiculopathy. Muscle Nerve 1990; 13:1032-1036. Criteria Met (5/6: 1,2,3,5,6) The authors assessed the usefulness of thermography in 14 patients with clinically defined cervical radiculopathy. Needle EMG was abnormal in 71% of patients, and was found to be more sensitive and specific than thermography. See text.
- Streib E, Daube JR: Electromyography of paraspinal muscles. Neurology1975; 386. Abstract only.
- Tackmann W, Radu EW: Observations on the application of electrophysiological methods in the diagnosis of cervical root compressions. Eur Neurol 1983; 22:397-404. Criteria Met (6/6: 1,2,3,4,5,6) Twenty patients with C6 and/or C7 radiculopathy were studied. Needle EMG was abnormal in 19 patients, but correlated with the clinically defined level of involvement in only 11 patients. See text.
- Teresi LM, Lufkin RB, Reicher MA, Moffit BJ, Vinuela FV, Wilson GM: Asymptomatic degenerative disk disease and spondylosis of the cervical spine: MR imaging. Radiology 1987; 164:83-88. Background Reference.
- Thacker AK, Misra S, Katiyar BC: Nerve conduction studies in upper limbs of patients with cervical spondylosis and motor neuron disease. Acta Neurol Scand1988; 78:45-48. Criteria Met (2/6: 1,2) Only nerve conduction studies were studied.
- Tsai CP, Huang CI, Wang V, Lin KP, Liao KK, Yen DJ, Wu ZA: Evaluation of cervical radiculopathy by cervical root stimulation. Electromyogr Clin Neurophysiol 1994; 34:363366. Criteria Met (4/6: 1,2,3,6) Thirty-two patients with clinical evidence of unilateral cervical radiculopathy were included. Cervical root stimulation was more sensitive (78.1%) than needle EMG examination (56.2%). See text.
- Waylonis GW: Electromyographic Findings in Chronic Cervical Radicular Syndromes. Arch Phys Med Rehab1968; 49:407-412. Criteria Met (3/6: 2,5,6) Needle electromyographic abnormality was seen in 72% of 113 patients with chronic cervical radiculopathy. Fibrillation potentials and/or positive waves were seen in 42%, and polyphasic motor unit potentials were encountered in all patients with abnormal needle EMG. See text.
- Wilbourn AJ, Aminoff MJ: AAEE minimonograph 32: the electrophysiologic examination in patients with radiculopathies. Muscle Nerve 1998; 21:1612-1631. Background Reference.
- Yiannikas C, Shahani BT, Young RR: Short-Latency Somatosensory-Evoked Potentials from Radial, Median, Ulnar, and Peroneal Nerve Stimulation in the Assessment of Cervical Spondylosis. Comparison With Conventional Electromyography. Arch Neurol 1986; 43:1264-1271. Criteria Met (4/6: 1,2,3,6) Needle EMG was normal in all 10 patients with only pain and no objective sign of cervical radiculopathy, whereas it was abnormal in 9 of 10 patients with signs of root compression. The sensitivity of needle EMG was better than those of SEPand F wave. See text.
- Yu YL, Jones SJ: Somatosensory evoked potentials in cervical spondylosis. Correlation of median, ulnar and posterior tibial nerve responses with clinical and radiological findings. Brain 1985; 108:273-300. Criteria Met (2/6: 1,2) Among the 34 patients studied, 15 had myelopathy alone, 6 had radiculopathy, and another 6 had combined radiculopathy and myelopathy. SEP abnormalities correlated strongly with myelopathy but not with radiculopathy.
Document History
Approved by the American Association of Neuromuscular & Electrodiagnostic Medicine: June 1998.
Endorsed by the American Academy of Physical Medicine and Rehabilitation: March 1999.
This guideline is greater than 5 years old. Every 5 years, an interim literature search is performed and the guideline is reviewed. While new studies have been published since this guideline was last reviewed, the Practice Issue Review Panel Committee of the AANEM has determined that these studies are not sufficient to mandate a revision of this guideline at the present time. The information contained in this guideline and the recommendations offered are still relevant to current practice.
Reaffirmed by the Practice Issue Review Panel: March 2015, October 2020
Muscle Nerve 22: Supplement 8: S209-S211, 1999
Creation of New Guidelines, Consensus Statements, or Position Papers
AANEM members are encouraged to submit ideas for papers that can improve the understanding of the field. The AANEM will review nominated topics on the basis of the following criteria:- Members’ needs
- Prevalence of condition
- Health impact of condition for the individual and others
- Socioeconomic impact
- Extent of practice variation
- Quality of available evidence
- External constraints on practice
- Urgency for evaluation of new practice technology
