2026 Medicare Physician Fee Schedule – What it Means for Your Practice
Published December 29, 2025
News Practice
AANEM continues to closely monitor and advocate Medicare payment policies that directly affect NM and EDX medicine. On October 31st, 2025, the Centers for Medicare & Medicaid Services (CMS) issued its annual 2026 Medicare Physician Fee Schedule (PFS) Final Rule that announces finalized regulatory changes for Medicare payments under the PFS effective on or after January 1, 2026. AANEM reviewed the final rule to assess its impact on NM and EDX services and physician reimbursement.
Even though the CY 2026 PFS includes a 1-year 2.5% increase and small baseline updates to the Medicare conversion factor, CMS’ new 2.5% “efficiency adjustment”, these offsetting policies result in effective payment reductions for EDX codes commonly billed by AANEM members. Below is a table comparing the CY 2026 RVUs for some commonly billed EDX codes with their CY 2025 RVUs to illustrate the impact of the PFS RVU and efficiency adjustments on AANEM members’ Medicare reimbursement.
Even with the CY 2026 increase, the conversion factor does not keep pace with inflation, and CMS’ continued reliance on imperfect budget neutrality forecasts threatens payment stability for NM and EDX subspecialists with high equipment and workforce costs. AANEM has repeatedly raised these concerns with CMS and Congress and remains committed to advocating for physician reimbursement by urging congressional action establishing a permanent, annual inflation-based update to the conversion factor tied to the MEI to protect physician practices and safeguard Medicare beneficiaries’ access to specialized neuromuscular and electrodiagnostic care.
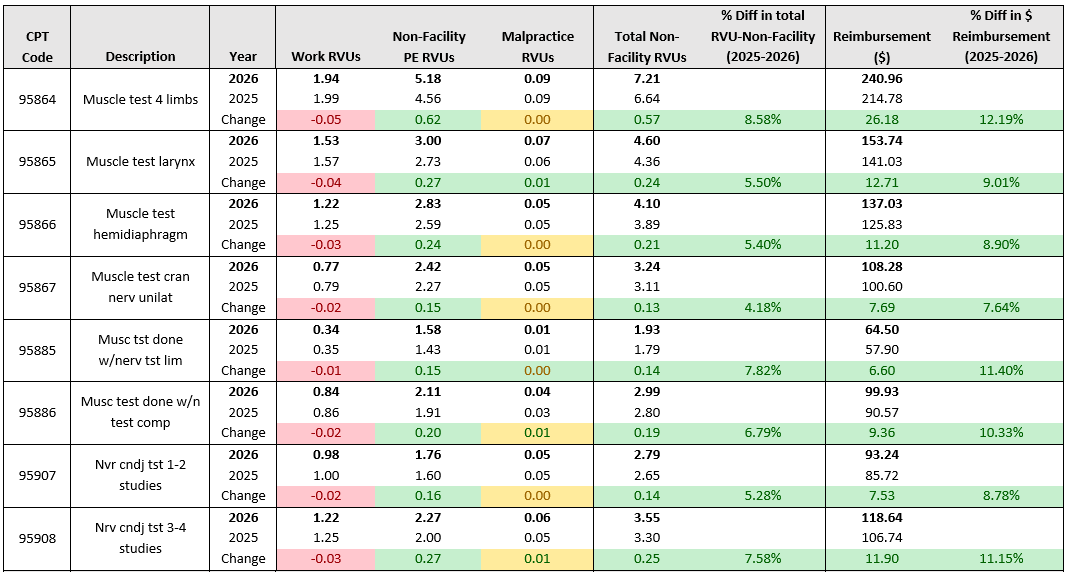
More RVU resources, including the full Medicare Physician Fee Schedule 2025/2026 RVU Comparison and Nerve Conduction Studies and Needle EMG 2025/2026 RVU Comparison documents can be found here.
AANEM is actively advocating for long term payment stability and supports congressional efforts to reform the Medicare payment system, including supporting:
· Medicare Patient Access and Practice Stabilization Act (HR 879), which seeks a 2% payment increase for physician services performed between April 1, 2025, and January 1, 2026; and
· The Strengthening Medicare for Patients and Providers Act (HR 6160) which would provide physicians with a permanent inflation update based on the Medicare Economic Index (MEI) starting in 2026.
These reforms are critical to protecting patient access to high-quality NM and EDX care, and AANEM will continue to advocate on behalf of its members and the patients they serve at CMS and on Capitol Hill.
